Abstract
Purpose
The role of initial conservative therapy with selective surgery for patients with suspected blunt bowel injury by radiologic evaluation is less clear. The aim of the study is to assess the outcomes of patients who received initial conservative therapy with selective delayed surgery, compared to emergency surgery.
Methods
During this 8-year study, a total of 77 patients who were hemodynamically stable were enrolled, in which computed tomography verified suspected bowel injury from blunt trauma (mesenteric hematoma, mesenteric fat infiltration, bowel wall thickening, and free fluid without solid organ injury) was managed with either initial conservative therapy with selective delayed surgery (group A; n = 42) or emergency surgery (group B; n = 35). The clinical outcomes including the rate of negative or nontherapeutic exploration and postoperative complications, between the groups were compared.
Results
The enrolled patients had a mean age of 41 years including 51 men and 26 women. No difference in the clinical characteristics was found between the groups. In group A, 18 patients underwent delayed surgery and 24 recovered without surgery. Among patients who underwent surgery, 3 (17%) underwent negative or nontherapeutic explorations. In group B, 13 (37%) underwent negative or nontherapeutic explorations. Postoperative complications occurred in 21 patients and there was no difference between the groups.
Bowel and mesenteric injury after blunt trauma can be difficult to assess at initial presentation, and this can result in significant morbidity and mortality. However, some patients with suspected injury may not require immediate surgical intervention.
Bowel and mesenteric injuries are a rare occurrence following blunt abdominal trauma. Typical locations of injury include the fixed segments of the bowel that undergo shearing forces during trauma. Initial clinical examination may yield benign results as peritoneal symptoms can be delayed.
The use of CT scans in the diagnosis of bowel and mesenteric injury is widespread [123]. However, this is not a reliable radiologic method for the prediction of bowel injury requiring surgery.
The optimal management of hemodynamically stable patients who have suspected blunt bowel injury, such as mesenteric hematoma, mesenteric fat infiltration, bowel wall thickening, or free peritoneal fluid is unclear [4]. Although imaging modalities have advanced, the potential for missed or hidden injuries were remained [5678].
Moreover, patients with suspected bowel injury after blunt trauma are relatively rare and heterogenous; thus, intensive analysis has scarcely been reported.
Although initial conservative therapy with selective delayed surgery has an increased risk of complications [91011], it may be beneficial in the clarification of precise diagnosis and appropriate treatment in the patients [12]. Additionally, it may also minimize nontherapeutic exploration, which carries a risk of substantial complications.
In the present study, we evaluated the clinical outcomes of initial conservative therapy with selective delayed surgery in hemodynamically stable patients with suspected bowel injury from blunt abdominal trauma, compared to emergency surgery.
This was conducted as a retrospective cohort study at 2 referral centers after receiving approval from the local ethic committee (13-1072).
Over a span of 8 years (2007–2014), a total of 126 patients were diagnosed with blunt bowel trauma from abdomino-pelvic CT scan and received inpatient management.
We excluded 49 patients who required emergency surgery for large pneumoperitoneum, bowel ischemia, other complicated solid organ injuries, or large extravasation of contrast from bowel or mesenteric injury by CT scan at the admission.
Finally, 77 patients with suspected bowel injury, which we defined as radiological evidence of mesenteric hematoma, mesenteric fat infiltration, bowel wall thickening, or free fluid in peritoneal cavity, were assessed. All patients were hemodynamically stable and had no combined injuries requiring emergency surgery.
To evaluate the severity of multiple injuries, the Injury Severity Score (ISS) was used. This is an anatomical scoring system that provides an overall score for patients with multiple injuries. Each injury is assigned an Abbreviated Injury Scale (from 1 minor to 6 maximum) and is allocated to one of 6 body regions. The 3 most severely injured body regions have their score squared and added together to produce the ISS score (range, 0–75). Major trauma is commonly defined using an ISS threshold of 15. This score is associated with trauma-related mortality [13].
Of 77 enrolled patients, 42 patients (55%) received initial nonoperative management which involved fasting and close observation with intravenous administration of antibiotics (group A). During the observation period, we repeated physical examinations and laboratory tests to re-evaluate the patient. We also performed repeat CT scans in all cases between 2 and 7 days after admission. CT scans were performed earlier in patients with progressive clinical symptoms or aggravated laboratory parameters.
Delayed surgery was performed selectively in patients with aggravated clinical symptoms, increasing laboratory parameters, including WBC and CRP, and radiological findings showing definite bowel injury, or progression of suspected bowel injury after a repeat CT scan.
The remaining 35 underwent emergency surgery (group B). Emergency surgery was performed within 24 hours after admission and initial evaluation.
Treatment was determined by either surgeon or patient preference after full clinical consideration and discussion. The clinical outcomes of this study included the rate of negative or nontherapeutic exploration and postoperative complications between 2 groups.
This study included 51 men and 26 women with a mean age of 41 ± 15 years (range, 17–78 years). The main clinical symptoms was whole abdominal pain with tenderness and there were 29 patients (38%) with fever (≥38.3℃).
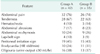
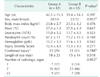
Table 1 demonstrated descriptions of initial physical examinations between the 2 groups. Traffic accidents, falls, and construction accidents were the major causes of blunt trauma. Other injuries involved bicycle accidents, heavy machinery, fighting, or playing. The mean ISS was 13 ± 4. Group A had a mean ISS 12.4 (range, 6–23) and group B had a mean 13.5 (range, 6–26) (P = 0.271). The clinic-laboratory characteristics of enrolled patients were summarized and there were no differences between the 2 groups (Table 2).
The specific radiologic signs included mesenteric hematoma, mesenteric fat infiltration, bowel wall thickening, or free fluid in peritoneal cavity and were polymorphic. Twelve patients had a single radiologic sign of suspected bowel trauma, 49 had 2 signs, and 16 had more than 3 signs.
In the group A, 18 (43%) underwent delayed surgery. After repeat CT scans, 4 patients had definite pneumoperitoneum or bowel ischemia signs and 12 had mild, progressive or equivocal findings with aggravation of clinical and laboratory findings. They subsequently underwent delayed surgery (2–4 days after admission). There were 2 patients with equivocal findings after repeat CT scans and improvement of clinical findings. However, they showed abrupt aggravation of clinical symptoms and underwent surgery on days 6 and 9 posttrauma, respectively. The delayed surgery was performed on 3 ± 2 days (range, 2–9 days) after admission.
In operative finding, negative or nontherapeutic surgical findings were observed in 3 patients who had only mesenteric hematoma and inflammation intraoperatively (3 of 18, 17%). Six patients had serosal tears with peritonitis, 4 had bowel ischemia, 4 had free perforation, and 1 had active hemorrhage from the bowel and mesentery. The affected sites were mostly the proximal jejunum and terminal ileum. Operative procedures included bowel resection, primary repair of injured site, and bleeding control.
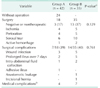
During the postoperative period, 3 patients developed wound infections, 2 had a prolonged ileus over 7 days, and 1 patient had intra-abdominal fluid collection treated with percutaneous drainage. Additionally, 1 patient was readmitted for adhesive ileus symptoms 4 months after trauma, and was treated conservatively.
The remaining 24 patients experienced an improvement of symptoms and signs after continuous conservative treatment until normalization of laboratory parameters and fasting until pain relief. They were discharged and followed-up at least 2 times. One patient experienced recurrent abdominal pain during the follow-up period, and was treated conservatively.
In group B, 13 (37%) had negative or nontherapeutic surgical findings. During the postoperative period, 5 patients had wound infections, 5 had prolonged ileus, 2 patients had intra-abdominal fluid collection and were treated with percutaneous drainage, and 1 had anastomotic leakage treated with reoperation. Additionally, 1 patient was readmitted for an incisional hernia and underwent surgery 11 months after trauma (Table 3).
Blunt bowel trauma may result in the formation of mesenteric hematomas, fat infiltration, bowel wall thickening, or free fluid. This poses a diagnostic dilemma given the potential for delayed bowel ischemia or perforation.
In our study, the decision to operate on patients treated conservatively was based on frequent clinical, laboratory, and radiologic examinations.
Although clinical examination can be easily conducted in patients with alert mental status, it is an unreliable method of assessing the severity of blunt bowel injury. Additionally, bowel trauma may be occurred either combined injuries or an isolated injury. Masked symptoms may inhibit the reliability of clinical examinations. Therefore, laboratory testing and CT scans are also required to make an accurate assessment.
Repeat CT scans can provide useful information in patients with suspected bowel injuries [14]. CT images were utilized in all our patients, and revealed some cases with progressive or definitive radiologic evidence of bowel injury. It is worth noting that initial suspicious signs can change and radiological findings may be delayed and seen only after the progression of bowel injury. Repeat CT scans are recommended for patients with initial suspected bowel injury.
Diagnostic laparoscopy may be a good treatment option in these patients [1516]. However, this would require general anesthesia, which may potentially aggravate the patient' condition, and the risk of unnecessary surgery or an invasive procedure still remains.
In addition, laparoscopic procedures may interfere with the spontaneous healing process, deteriorate bleeding focus from the pneumoperitoneum, or lead to iatrogenic injury for friable tissue. We experienced a case that required extensive resection for surgical injury during the dissection of inflammatory phlegmon.
Taking an initial nonoperative approach for suspected bowel injury seems to increase the rate of delayed diagnosis. To reduce morbidity or mortality, time to surgery has been emphasized. Long interval between presentation and surgery was found to be associated with complications [1718]. However, in this study, any difference was not found in postoperative complications between delayed and emergency surgery. We included only the cases with suspected bowel injury, thus, the result of complications from delayed surgery may be slightly different to other literature.
The risk factors of delayed surgery could not be fully evaluated due to relatively small number of patients. Among 42 patients with initial conservative therapy, 18 (43%) underwent delayed surgery. The proportion of patients with delayed surgery got increased as the radiological signs advanced (Table 4).
Additionally, patients with delayed surgery had younger age (36 years vs. 47 years) and higher WBC at admission (12.8 vs. 9.7 103/L) than patients without surgery, but it was not statistically significant.
The prompt or accurate diagnosis of bowel injury is challenging. Despite trying to decrease the missing rate, it could be inevitable. For timely diagnosis, many patients may endure the risk of unnecessary surgery or invasive procedures. This can be significant for patient management as well as to avoid long delays. We suggest that bowel trauma may resolve spontaneously or progress after initial injury. The missed injuries may include gradually advanced bowel lesions [1920].
Moreover, the outcome of delayed diagnosis is not always poor [21]. The rate of missed injuries after initial evaluation may be decreased through the use of advanced technology, and the risk of delayed diagnosis could be reduced through improvements to the intensive care system [2223].
In conclusion, it may not be possible to eliminate negative or nontherapeutic exploration, but they could be minimized by selective delayed surgery.
Our retrospective review revealed that more than half of patients successfully recovered without surgery. Although the clinical decision in the treatment of hemodynamically stable patients with suspected traumatic bowel injuries rests with surgeon, initial nonoperative management with selective delayed surgery is a good treatment option to avoid unnecessary surgery.
Figures and Tables
References
1. Pal JD, Victorino GP. Defining the role of computed tomography in blunt abdominal trauma: use in the hemodynamically stable patient with a depressed level of consciousness. Arch Surg. 2002; 137:1029–1032.

2. Petrosoniak A, Engels PT, Hamilton P, Tien HC. Detection of significant bowel and mesenteric injuries in blunt abdominal trauma with 64-slice computed tomography. J Trauma Acute Care Surg. 2013; 74:1081–1086.

3. Joseph DK, Kunac A, Kinler RL, Staff I, Butler KL. Diagnosing blunt hollow viscus injury: is computed tomography the answer? Am J Surg. 2013; 205:414–418.

4. Brownstein MR, Bunting T, Meyer AA, Fakhry SM. Diagnosis and management of blunt small bowel injury: a survey of the membership of the American Association for the Surgery of Trauma. J Trauma. 2000; 48:402–407.

5. Sherck J, Shatney C, Sensaki K, Selivanov V. The accuracy of computed tomography in the diagnosis of blunt small-bowel perforation. Am J Surg. 1994; 168:670–675.

6. Ekeh AP, Saxe J, Walusimbi M, Tchorz KM, Woods RJ, Anderson HL 3rd, et al. Diagnosis of blunt intestinal and mesenteric injury in the era of multidetector CT technology: are results better? J Trauma. 2008; 65:354–359.
7. Bhagvan S, Turai M, Holden A, Ng A, Civil I. Predicting hollow viscus injury in blunt abdominal trauma with computed tomography. World J Surg. 2013; 37:123–126.

8. Mahmood I, Tawfek Z, Abdelrahman Y, Siddiuqqi T, Abdelrahman H, El-Menyar A, et al. Significance of computed tomography finding of intra-abdominal free fluid without solid organ injury after blunt abdominal trauma: time for laparotomy on demand. World J Surg. 2014; 38:1411–1415.

9. Fischer RP, Miller-Crotchett P, Reed RL 2nd. Gastrointestinal disruption: the hazard of nonoperative management in adults with blunt abdominal injury. J Trauma. 1988; 28:1445–1449.
10. Fakhry SM, Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma. 2000; 48:408–414.
11. Malinoski DJ, Patel MS, Yakar DO, Green D, Qureshi F, Inaba K, et al. A diagnostic delay of 5 hours increases the risk of death after blunt hollow viscus injury. J Trauma. 2010; 69:84–87.

12. Ozturk H, Dokucu AI, Onen A, Otcu S, Gedik S, Azal OF. Non-operative management of isolated solid organ injuries due to blunt abdominal trauma in children: a fifteen-year experience. Eur J Pediatr Surg. 2004; 14:29–34.

13. Sim J, Lee J, Lee JC, Heo Y, Wang H, Jung K. Risk factors for mortality of severe trauma based on 3 years' data at a single Korean institution. Ann Surg Treat Res. 2015; 89:215–219.

14. Walker ML, Akpele I, Spence SD, Henderson V. The role of repeat computed tomography scan in the evaluation of blunt bowel injury. Am Surg. 2012; 78:979–985.

15. Kaban GK, Novitsky YW, Perugini RA, Haveran L, Czerniach D, Kelly JJ, et al. Use of laparoscopy in evaluation and treatment of penetrating and blunt abdominal injuries. Surg Innov. 2008; 15:26–31.

16. Johnson JJ, Garwe T, Raines AR, Thurman JB, Carter S, Bender JS, et al. The use of laparoscopy in the diagnosis and treatment of blunt and penetrating abdominal injuries: 10-year experience at a level 1 trauma center. Am J Surg. 2013; 205:317–320.

17. Faria GR, Almeida AB, Moreira H, Barbosa E, Correia-da-Silva P, Costa-Maia J. Prognostic factors for traumatic bowel injuries: killing time. World J Surg. 2012; 36:807–812.

18. Matsushima K, Mangel PS, Schaefer EW, Frankel HL. Blunt hollow viscus and mesenteric injury: still underrecognized. World J Surg. 2013; 37:759–765.

19. Subramanian V, Raju RS, Vyas FL, Joseph P, Sitaram V. Delayed jejunal perforation following blunt abdominal trauma. Ann R Coll Surg Engl. 2010; 92:W23–W24.

20. Ertugrul G, Coskun M, Sevinc M, Ertugrul F, Toydemir T. Delayed presentation of a sigmoid colon injury following blunt abdominal trauma: a case report. J Med Case Rep. 2012; 6:247.

21. Letton RW Jr, Worrell V, Tuggle DW. American Pediatric Surgical Association Committee on Trauma Blunt Intestinal Injury Study Group. Delay in diagnosis and treatment of blunt intestinal perforation does not adversely affect prognosis in the pediatric trauma patient. J Trauma. 2010; 68:790–795.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download