Abstract
Purpose
Because data as a basis for the determination of proper age and modality for screening of colorectal neoplasms is lacking, we evaluated detection rates and anatomical distribution of colorectal neoplasms according to age in healthy individuals who underwent total colonoscopy for health checkup.
Methods
A total of 16,100 cases that had received the colonoscopic examination from January to December in 2014 were analyzed. The total number of individuals who received total colonoscopy were divided by the number of individuals harboring colorectal adenoma to calculate the detection rate of colorectal adenoma. Individuals ≤50 years old were classified as young-age group and aged >50 were old-age group. Differences in anatomical locations of colorectal neoplasms were analyzed in the 2 age groups by chi-square test. Risk factors for colorectal adenoma in each age group were analyzed using univariate and multivariate logistic regression analyses.
Results
Detection rates of colorectal adenoma were 13.7% in all cases and 12.8% for those in their 40′s. The main anatomical location of colorectal adenoma was proximal colon in both age groups (P < 0.001). Hyperplastic polyp was mainly distributed to the distal colon in both age groups (P < 0.001). Distal colon was the major site for colorectal cancer in the old-age group (P = 0.001). Proximal location of neoplasms was a risk factor for colorectal adenoma in both age groups with multivariate analysis.
Colorectal cancer (CRC) was reported to be the 4th-leading cause of cancer mortality in South Korea in 2013. While some of major cancers such as lung, stomach, and liver cancer were reported to have decreased from 1999 to 2013, CRC steadily increased during the same period, and it is one of the greatest threats resulting from cancer mortality [1]. Although CRC is a major life-threatening disease, risk of death is known to be decreased by colonoscopy. A recent study comparing mortality between subjects with screening by colonoscopy or sigmoidoscopy and those without endoscopy reported a reduction of mortality by 68% in those who received colonoscopy [2]. Generally, it is known that the incidence of CRC increases with age, and more than 80% of patients with CRC are diagnosed after 55 years of age [3]. Due to the rarity of incidence of CRC in average-risk individuals under the age of 40, it has been recommended to start screening by endoscopy or stool-based study from 50 years of age [456]. However, several studies have reported increasing incidence of CRC in adults under the age of 50 years; meanwhile, incidence and mortality rates in individuals over 50 are decreasing [7891011]. Furthermore, the prevalence of adenoma in asymptomatic healthy young-aged adults of under 50 has been reported to range from 12.5%–36%, almost equivalent to that of the elderly aged 50–60 years [12131415]. Although most adenomas stabilize and regress, removal of low-risk adenomas is reported to be effective showing 25% reduction of mortality as compared with CRC mortality rates in the general population [16]. Because the frequency of colorectal adenoma in young-aged adults should not be overlooked given that the majority of CRC is known to develop from colorectal adenomas through the well-known process of adenomacarcinoma sequence [17], continuous efforts have been made to clarify the risk factors for development of adenoma in young-aged adults. Several studies have proposed male sex, current smoker, alcohol consumption, obesity, and screening for colorectal adenoma as common risk factors, and those clinical factors could be indications for screening of colorectal adenoma in young-aged individuals [1213141518].
Contrary to the enormous efforts on evaluation of risk factors for adenoma, data on detection rates of colorectal neoplasms or effective tools for screening according to age is lacking. Several different screening procedures such as colonoscopy, flexible sigmoidoscopy, computed tomography, or fecal-based screening are currently used, and colonoscopy is the most complete modality for both detection and removal of polyps found during the procedure. However, several issues such as relative invasiveness, inconvenience due to diet restriction and bowel preparation, possible adverse events resulting from sedation and colonoscopic procedures, like perforation or bleeding, or time-consuming features, limit the choice of total colonoscopy as the routine practice of colorectal screening. Flexible sigmoidoscopy might be a preferred method for endoscopists because sedation is rendered unnecessary and less bowel cleansing is required compared to total colonoscopy. Many previous data support the benefit of flexible sigmoidoscopy in reducing the mortality risk of CRC [19202122]. However, several studies have shown flexible sigmoidoscopy as an ineffective screening tool in reducing mortality from proximal colon cancer by showing reduction of mortality only after colonoscopic screening [22324].
For effective screening of CRC, base data for determination of appropriate age and modality for screening is of most importance. We believe evaluation on anatomical location and detection rates of colorectal neoplasms according to age could be solutions to address the presented issues. We also attempted to clarify the risk factors for colorectal adenoma according to age groups in this study.
A total of 16,100 asymptomatic patients who underwent total colonoscopy for the purpose of health checkup at Korea Medical Institute (KMI), Gangnam Center from January to December in 2014 were analyzed retrospectively. This study was carried out according to the principles in the Declaration of Helsinki 1964, and the Institutional Review Board (IRB) of Korea University Guro Hospital approved the study protocol (approval number: KUGH15202-001). Informed consent was waived by the IRB.
A total of 8 doctors performed colonoscopy during the study period. Diagnosis and classification of colorectal neoplasms were confirmed histopathologically. Subjects with inadequate colonoscopic examination due to poor bowel preparation and existing bowel disease such as inflammatory bowel disease were excluded. Cases were divided into 6 groups according to age (<30, 30–39, 40–49, 50–59, 60–69, and ≥70 years old) to analyze detection rates of colorectal adenoma. Characteristics of subjects and colorectal polyps, anatomical distribution of colorectal neoplasms, and risk factors of colorectal adenoma were analyzed between the 2 age groups: the young-age group (≤50 years old) and the old-age group (>50 years old).
Metabolic syndrome was defined according to the criteria of the International Diabetes Federation as central obesity and any 2 of the followings: (1) raised triglycerides levels of more than 150 mg/dL or ongoing treatment for this lipid abnormality, (2) decreased HDL cholesterol levels of less than 40 mg/dL in males and less than 50 mg/dL in females or treatment for this lipid abnormality, (3) elevated blood pressure (BP) with systolic BP > 130 mmHg or diastolic BP > 85 mmHg, or treatment on hypertension, or (4) elevated fasting plasma glucose of more than 100 mg/dL or previously diagnosed type II diabetes. Waist circumference ≥90 cm in males and ≥80 cm in females were used to define central obesity. Body mass index (BMI) was calculated as the individual's body mass (kg) divided by the square of height (m2). BMI >25 kg/m2 was defined as obese based on Asia-Pacific criteria.
The total number of individuals who received total colonoscopy were divided by the number of individuals harboring colorectal adenoma to calculate detection rate. Subjects with experience of previous colonoscopy were included. The detection rate was calculated according to age and sex. Characteristics of colorectal neoplasms including anatomical location were analyzed in 3,393 individuals. Colorectal neoplasms were classified as adenoma, hyperplastic polyp, inflammatory polyp, carcinoid tumor, and malignancy. Clinically insignificant colorectal neoplasms that did not belong to above classifications were categorized as other. We defined proximal colon as from the ileo-cecal valve through the ascending colon and transverse colon to the descending colon. Distal colon was defined as sigmoid colon and rectum considering limitations of the depth of insertion to the sigmoid-descending colon junction at sigmoidoscopy [1225]. Analysis of risk factors for colorectal adenoma was performed in 2,395 subjects with the following clinical variables: sex (male vs. female), smoking history (ex- or current smokers vs. never smokers), alcohol history, previously diagnosed diabetes, previously diagnosed hypertension, waist circumference (≥90 cm in males, ≥80 cm in females), BMI (>25 kg/m2), presence of metabolic syndrome, previous colonoscopy history, location of colorectal polyps (proximal vs. distal colon), triglyceride (≥150 mg/dL), HDL cholesterol (<40 mg/dL in males, <50 mg/dL in females), LDL cholesterol (>100 mg/dL), total cholesterol (≥200 mg/dL), CEA (>1 ng/mL), and hemoglobin level (>13 g/dL).
Laboratory variables were initially recorded as continuous variables and later dichotomized for ease of statistical analysis. Clinical characteristics were compared between 2 age groups using chi-square test and Student t-test. Chi-square test was also employed to evaluate the difference of anatomical locations of colorectal neoplasms according to pathologic findings. Univariate and multivariate logistic regression analyses were performed to identify significantly independent risk factors for adenoma. Significant risk factors found with univariate analysis were included in multivariate analysis. Results were expressed as odds ratio (OR) and 95% confidence intervals (CI). P < 0.05 was considered statistically significant. Statistical analysis was performed with IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA).
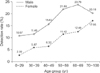
The detection rate of colorectal adnoma was 13.7% in all subjects. The rate increased according to age, and a detection rate of 9.49% was recorded in individuals in their 30′s, 12.75% in those in their 40′s, 18.48% in their 50′s, 18.81% in their 60's, and 19.02% in their 70′s. Statistical significance was noted up to 50 years of age, and no significant difference was observed between 50 and 60 years of age (P = 0.785), and 60 and 70 years of age (P = 0.929). Detection rates were higher in males than in females throughout all age groups. Of note, there was significant difference in the detection rate between 30 and 40 years of age (P < 0.001) in males while significant difference was noted between 40 and 50 years of age (P < 0.001) in females (Fig. 1).
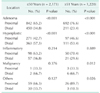
The ascending colon was the most frequent anatomical location of colorectal polyps in both groups. Adenoma was the most commonly described histology of colorectal neoplasms in both age groups, but a higher proportion of cases had adenoma in the old-age group (74.0%). Almost two-thirds of subjects are shown to harbor only one polyp through the whole colon (Table 1).
Difference in anatomical location of colorectal polyps according to the histologic classification was analyzed in both age groups. Significantly larger numbers of colorectal adenoma were located in the proximal colon in both age groups (65.2% in the young-age group, 76.6% in the old-age group, P < 0.001 in both age groups). The young-age group was classified into three groups (41–50 and 31–40 years old groups, and 1 group aged less than 30) again, and each group was analyzed on the location of the adenoma. Significantly larger numbers of subjects harbored adenomas in the proximal colon in those aged above 30 years (P < 0.001) (Supplementary Table 1). The larger proportion of hyperplastic polyps was located in the distal colon (57.3% in the young-age group, 53.4% in the old-age group, P < 0.001 in both age groups). The distribution of inflammatory polyps showed no statistically significant difference in both age groups. Distal colon was the major site for colorectal adenocarcinoma in the old-age group (66.7%, P = 0.012). Other unclassified clinically insignificant polyps were distributed mainly in the proximal colon (89.7%, P < 0.026) in the old-age group (Table 2).
The characteristics of each age group are summarized in Table 3. The median age at colonoscopic examination is 57 years (range, 5–78 years) and 41 years (range, 24–50 years) in the old-age and the young-age group, respectively. The proportions of cases with smoking and alcohol consumption are larger in the young-age group (P < 0.001). Cases with underlying medical diseases such as diabetes mellitus and hypertension are occupied with higher proportions in the old-age group (P < 0.001). A larger proportion of cases with previous colonoscopy were found in the old-age group (P < 0.001). There was no significant difference between the 2 age groups in the mean levels of HDL (P = 0.057), LDL (P = 0.835), and total cholesterol (P = 0.092).
Risk factors for colorectal adenoma were analyzed in both age groups (Tables 4, 5). Waist circumference (≥90 cm in males, ≥80 cm in females, P = 0.048), proximally located colorectal polyps (P < 0.001), total cholesterol level ≥200 mg/dL (P = 0.019), hemoglobin level higher than 13 g/dL (P = 0.021) were revealed to be significantly associated with colorectal adenoma in the young-age group by univariate analysis. Multivariate analysis showed colorectal neoplasms located in the proximal colon (P < 0.001; OR, 1.975; 95% CI, 1.599–2.440) and hemoglobin higher than 13 g/dL (P = 0.040; OR, 1.487; 95% CI, 1.017–2.173) were significant clinical factors independently associated with colorectal adenoma. In the old-age group, male gender (P = 0.034), cases with smoking history (P = 0.009), subjects who received previous colonoscopy (P = 0.013), proximal location of colorectal polyps (P < 0.001), and hemoglobin levels higher than 13 g/dL (P = 0.040) were shown to be significantly associated with colorectal adenoma by univariate analysis. Independently significant risk factors were presence of smoking history (P = 0.008; OR, 1.525; 95% CI, 1.115–2.086) and proximally located neoplasms (P < 0.001; OR, 3.091; 95% CI, 2.250–4.248) with multivariate analysis.
With the increase of incidence of sporadic CRC in young adults, several behavioral and environmental factors for CRC have been proposed. In addition to those etiologies, lack of screening on colorectal neoplasms in young adults and subsequent negligence regarding the premalignant lesion has been regarded as one of multiple reasons for the phenomenon. Our data showed approximately 13% of all individuals in their 40′s with total colonoscopy harbored colorectal adenoma, consistently providing reason for earlier start of colorectal adenoma screening. Furthermore, subgroup analysis of the young-age group showed statistically significant proximal distribution of adenoma in individuals aged more than 30 years. For a significant increase in colorectal adenoma detection rates up to the 50′s age group, initiation of colonoscopic screening from 30 years of age would be best, though cost-effectiveness should be further verified. Interestingly, a significant increase in the detection rate occurred 10 years earlier in males in their 40′s than in females in their 50′s. Therefore, in the least, we would suggest male individuals initiate colonoscopic screening in their 40′s, 10 years earlier than female subjects do.
Although detection rates of colorectal adenoma in this study are a little lower than those reported in previous studies [12131415], results in this study might be more accurate given that this cross-section study was performed by analyzing data of subjects who had received colonoscopy during only a short period of 1 year. As a matter of fact, we compared the number of patients with CRC detected by total colonoscopy in KMI, Gangnam Center to the expected incidence of CRC in a population with screening of CRC in KMI, Gangnam Center in 2014 (16,100 cases) by calculating from incidences of CRC reported in an annual report of cancer statistics in South Korea, 2013 (Supplementary Table 2). By comparing the calculated expected number of cases with CRC, the practically detected numbers of CRC patients using colonoscopy were not inferior; therefore, were able to conclude that the detection rates presented in this study were not underestimated values.
Given that a substantial portion of all subjects carrying colorectal adenoma is occupied by young-aged adults, the importance of screening with colonoscopic examination in those age groups has arisen. Sigmoidoscopy has benefits in the point that it is less invasive and more convenient. However, it was demonstrated that sigmoidoscopic screening did not reduce mortality rates from proximal CRC [19202122]. In addition, data in our study suggest the necessity of total colonoscopic examination in screening of adenomas in the young-age group. A higher proportion of colorectal adenomas were located in the proximal colon in both age groups, which was statistically significant. On the other hand, larger numbers of hyperplastic polyps were located in the distal colon in both age groups, meaning screening with sigmoidoscopy has the potential to omit detection of clinically significant colorectal polyps. The anatomical distribution clarified in this study could explain the reason why sigmoidoscopic screening failed to reduce the mortality rate from CRC in previous studies [19202122].
Significantly different distribution of colorectal adenocarcinoma was shown between proximal and distal colon in the old-age group, revealing a discrepancy between locations of adenoma. Recent studies have reported a tendency of increase in rectal cancer in adults aged less than 55 years. In addition, stable incidence of rectal tumor was also reported in individuals aged 50 to 64 years despite an overall decrease of CRC incidence in those subjects [1011]. Although our data does not provide the exact incidence of CRC, the tendency of distribution of CRC is consistent to those results. Not all colorectal adenomas develop into malignancy, but several clinical factors such as size, grade of dysplasia, and growth pattern are reported to be associated with malignant evolution [17]. Since size of adenoma is one of the most important factors for transformation into malignancy [17], we examined the distribution of colorectal adenomas >1 cm. Of 23 adenomas >1 cm, 12 were located in the proximal colon, and distal concentration of high-risk adenoma was not the reason for distal distribution of carcinoma. Although it has yet to be clarified, it has been known that there is biological difference between right- and left-side colon cancer in its pathogenesis, and this might be one of the reasons for the discrepant location of colorectal adenoma and carcinoma. Another consideration is too small number of patients with carcinoma, such that significance of distal distribution of carcinoma should be re-evaluated with a larger number of patients with CRC. Carcinoid tumors were also detected in 6 cases in our study; all of them were grade 1 and located in the distal colon, consistent with the previous results [26].
Risk factors for colorectal adenoma were also analyzed to
suggest possible indications for colorectal screening, especially in the young-age group. Proximal location of colorectal neoplasms was shown to be a risk factor in both age groups with multivariate analysis, consistently suggesting the importance of examination of the proximal colon with total colonoscopy. Hemoglobin levels higher than 13 g/dL was revealed to be another risk factor in the young-age group. Although controversial results were reported in previous studies which evaluated the association between iron deficiency anemia and colorectal adenoma [27282930], a study which investigated the relationship between plasma levels of ferritin and colorectal polyps suggested a weak positive association [30]. Because iron exposure was reported to be an independently significant risk factor in the study [30], it would be better to pay attention to individuals with high ferritin and hemoglobin levels [1213141518]. Smoking history was presented as a risk factor in the old-age group, consistent with results in previously reported studies [121518].
We presented results that could be the basis for the determination of appropriate age and modality for colorectal adenoma screening in this study, but there are several limitations. First, we included not only individuals who received initial colonoscopy but also those who had received previous colonoscopy, and we were not able to estimate an accurate incidence of colorectal neoplasms. Second, this study was performed with medical records of only one medical institution in South Korea, which might have caused selection bias.
In conclusion, results shown in this study could be one of several evidences for earlier screening of colorectal neoplasms using total colonoscopy regardless of the age group. Further study clarifying cost-effectiveness of earlier screening and association between behavioral patterns of the young and risk of colorectal neoplasms would support the necessity of earlier colonoscopic screening more concretely.
Figures and Tables
Notes
References
1. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016; 48:436–450.

2. Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013; 369:1095–1105.

3. U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008; 149:627–637.
4. Levin B, Lieberman DA, McFarland B, Smith RA, Brooks D, Andrews KS, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008; 58:130–160.

5. International Agency for Research on Cancer. Lansdorp-Vogelaar I, von Karsa L. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition--Introduction. Endoscopy. 2012; 44:Suppl 3. SE15–SE30.
6. Lee BI, Hong SP, Kim SE, Kim SH, Kim HS, Hong SN, et al. Korean guidelines for colorectal cancer screening and polyp detection. Clin Endosc. 2012; 45:25–43.

8. Centers for Disease Control and Prevention (CDC). Vital signs: colorectal cancer screening, incidence, and mortality: United States, 2002-2010. MMWR Morb Mortal Wkly Rep. 2011; 60:884–889.
9. Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015; 150:17–22.

10. Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017; 67:177–193.

11. Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, et al. Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017; 109:DOI: 10.1093/jnci/djw322.

12. Chung SJ, Kim YS, Yang SY, Song JH, Park MJ, Kim JS, et al. Prevalence and risk of colorectal adenoma in asymptomatic Koreans aged 40-49 years undergoing screening colonoscopy. J Gastroenterol Hepatol. 2010; 25:519–525.
13. Bae T, Ha Y, Kim C, Lee J, Ha K, Shin S, et al. Distribution of the colonoscopic adenoma detection rate according to age: is recommending colonoscopy screening for koreans over the age of 50 safe? Ann Coloproctol. 2015; 31:46–51.

14. Kwak JY, Kim KM, Yang HJ, Yu KJ, Lee JG, Jeong YO, et al. Prevalence of colorectal adenomas in asymptomatic young adults: a window to early intervention? Scand J Gastroenterol. 2016; 51:731–738.

15. Lee SE, Jo HB, Kwack WG, Jeong YJ, Yoon YJ, Kang HW. Characteristics of and risk factors for colorectal neoplasms in young adults in a screening population. World J Gastroenterol. 2016; 22:2981–2992.

16. Loberg M, Kalager M, Holme O, Hoff G, Adami HO, Bretthauer M. Long-term colorectal-cancer mortality after adenoma removal. N Engl J Med. 2014; 371:799–807.

18. Kim JY, Jung YS, Park JH, Kim HJ, Cho YK, Sohn CI, et al. Different risk factors for advanced colorectal neoplasm in young adults. World J Gastroenterol. 2016; 22:3611–3620.

19. Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010; 375:1624–1633.

20. Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, et al. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian Randomized Controlled Trial--SCORE. J Natl Cancer Inst. 2011; 103:1310–1322.

21. Holme O, Loberg M, Kalager M, Bretthauer M, Hernan MA, Aas E, et al. Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: a randomized clinical trial. JAMA. 2014; 312:606–615.
22. Brenner H, Stock C, Hoffmeister M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ. 2014; 348:g2467.

23. Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012; 366:2345–2357.
24. Wang YR, Cangemi JR, Loftus EV Jr, Picco MF. Risk of colorectal cancer after colonoscopy compared with flexible sigmoidoscopy or no lower endoscopy among older patients in the United States, 1998-2005. Mayo Clin Proc. 2013; 88:464–470.

25. Painter J, Saunders DB, Bell GD, Williams CB, Pitt R, Bladen J. Depth of insertion at flexible sigmoidoscopy: implications for colorectal cancer screening and instrument design. Endoscopy. 1999; 31:227–231.

26. Taghavi S, Jayarajan SN, Powers BD, Davey A, Willis AI. Examining rectal carcinoids in the era of screening colonoscopy: a surveillance, epidemiology, and end results analysis. Dis Colon Rectum. 2013; 56:952–959.
27. Joosten E, Meeuwissen J, Vandewinckele H, Hiele M. Iron status and colorectal cancer in symptomatic elderly patients. Am J Med. 2008; 121:1072–1077.

28. Sawhney MS, Lipato T, Nelson DB, Lederle FA, Rector TS, Bond JH. Should patients with anemia and low normal or normal serum ferritin undergo colonoscopy? Am J Gastroenterol. 2007; 102:82–88.

29. Kishida T, Shinozawa I, Tanaka S, Hoshino T, Tatsuguchi A, Feng L, et al. Significance of serum iron and ferritin in patients with colorectal adenomas. Scand J Gastroenterol. 1997; 32:233–237.

30. Bird CL, Witte JS, Swendseid ME, Shikany JM, Hunt IF, Frankl HD, et al. Plasma ferritin, iron intake, and the risk of colorectal polyps. Am J Epidemiol. 1996; 144:34–41.
SUPPLEMENTARY MATERIALS
Supplementary Tables can be found via https://www.astr.or.kr/src/sm/astr-94-36-s002.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download