Abstract
Gigantomastia is a rare condition characterized by excessive breast growth. It has been reported that the majority of gigantomastia cases occur during either pregnancy or puberty. We were presented with a rare case of gigantomastia associated with neither pregnancy nor puberty, and successfully treated it with reduction mammaplasty and free nipple graft. This idiopathic gigantomastia is the very first case in Korea, and adds to the worldwide total of 9 reported cases.
Gigantomastia is a rare but disabling condition characterized by excessive breast growth. Mammary gland hyperplasia leads to severe mastalgia, back pain and trophic lesions of the breast skin with ulceration and infection. The cosmetic defect causes emotional and psychological disturbances such as depression and sociophobia [1,2].
Previous reports show that juvenile and pregnancy-induced gigantomastia are the most common causes of this condition [3]. Only 9 cases of idiopathic gigantomastia unrelated to puberty or pregnancy have been reported in literature [3,4,5,6]. In this case report, we present a case with idiopathic gigantomastia. We successfully used a method of reduction mammaplasty and free nipple graft to obtain good results.
A 43-year-old woman presented with a 2-year history of progressive, painful enlargement of both breasts. She complained of marked bilateral breast enlargement with no palpable masses. She had reached menarche at the age of 11 years and her menstrual cycles had been regular. She had two children, the first child was born when she was 33 and the second at age 36. During her pregnancy no significant enlargement of the breasts was noted, and there was also no significant personal medical or family history. The patient complained of mastalgia, back pain, and breathing difficulties. She additionally had sociophobia. The patient's body weight was 62.6 kg, and her height was 156.5 cm, with a body mass index of 25.74 kg/m2.
At the time of examination, both breasts were extremely enlarged, reaching below the umbilicus while in the standing position (Fig. 1). The left breast was slightly larger than the right breast. The skin covering the breasts showed marked pigmentation and dilated veins. Laboratory assays for hormone levels (β-human chorionic gonadotropin, insulin-like growth factor, growth hormone, prolactin, progesterone, thyroidstimulating hormone, testosterone, follicle-stimulating hormone and luteinizing hormone) and antinuclear antibodies were normal. Breast ultrasonography and mammography demonstrated enlarged dense breasts.
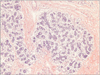
The histology underwent reduction mammaplasty with free nipple graft under general anesthesia (Fig. 2). Her postoperative course was uneventful. Both breast specimens appeared grossly normal and weighed 7.6 kg, the left breast weighing 5.1 kg and the right breast weighing 2.5 kg. The histology form showed a nodular, compact proliferation of small round tubules lined by epithelial and myoepithelial cells (Fig. 3). Immunohistochemistry staining for estrogen and progesterone receptor expression was positive in 10% of epithelial cells (Fig. 4). The patient had taken tamoxifen for one year after the surgery, and she was pleased with the outcome at the 18-month follow-up examination.
The term gigantomastia was first introduced by Palmuth in German literature in 1648. There is no universally accepted definition of gigantomastia, but many authors cite gigantomastia as breast enlargement that requires a reduction of over 1,500 g per breast. The largest recorded excised breast tissue weight to date is 27.5 kg per breast [7].
The exact pathogenesis of gigantomastia is still unclear. There are various hypotheses for pathophysiology: First, excessive release of endocrinologic hormones, such as estrogen or prolactin [8]. This is associated with the aspect that most gigantomastia develop during pregnancy or puberty. Second, gigantomastia is caused by hypersensitivity of associated hormonal receptors. Lanzon and Navarra [9] reported that immunohistochemistry staining results for estrogen and progesterone receptor expression were positive in more than 50% of epithelial cells. Unilateral gestational gigantomastia reported by Sakai et al. [10] might have been attributed to increased hypersensitivity of one breast over the other to the circulating hormones. With respect to other causes, it is known that gigantomastia may be induced by either autoimmune diseases, such as myasthenia gravis, systemic lupus erythematosus (SLE), Graves disease and rheumatoid arthritis or pharmacologic agents, such as penicillamine or cyclosporine.
Dancey et al. [3] attempted to classify gigantomastia using a literature review. In this study, 41 cases are gestational, 57 cases are juvenile, 13 cases are idiopathic, and 4 cases show drug-induced gigantomastia. Of the idiopathic cases, 3 were noted to have concurrent immunological diseases, and 1 was later found to have some features of SLE, suggesting an autoimmune origin. Only 9 cases had no obvious triggering cause. Our case also shows normal hormone levels and no other causes.
Treatments for gigantomastia are still controversial. Currently available treatment methods encompass conservative hormonal therapy, reduction mammaplasty, and simple mastectomy. In this reported case, the treatment of choice was surgery due to the enormous size of the breast and pain. This patient asked for a reduction mammaplasty despite the risk of recurrent hypertrophy. There is the possibility of recurrent hypertrophy of remaining breast tissues after reduction mammaplasty. Nevertheless, unlike cases of gigantomastia during pregnancy that have the risk of complications, such as abortion or maternal mortality, up to now, 8 out of 9 patients with idiopathic gigantomastia reported in literature underwent reduction mammaplasty, and none of them had recurrence [3,5,6]. Skillman et al. [4] reported a case of idiopathic gigantomastia that had developed cellulitis of the breast that had led to sepsis, for which urgent bilateral simple mastectomy was undertaken. In recurrent cases or cases of gigantomastia of anticipated pregnancy or puberty, simple mastectomy or nipple saving subcutaneous mastectomy with implants may be considered. Some reports described the management of juvenile and pregnancy-induced gigantomastia with hormonal therapy, such as bromocriptine, tamoxifen, danazol, and medroxyprogesterone. Therapeutic responses to pharmacologic agents are not consistent and more often temporary. There was a case of idiopathic gigantomastia, for which goserelin was administered before surgery but was ineffective [4]. While there was no other case for which hormonal therapy was carried out, our patient was administered with tamoxifen for one year after surgery. However, the aspect of effectiveness of tamoxifen could not be concluded.
The cause of idiopathic gigantomastia has not yet been elucidated and clinicians need to differentiate other causes of breast hypertrophy utilizing various tests. Continuous symptomatic manifestation requires surgical intervention and reduction mammaplasty should be considered as the first line of treatment. Continuous long-term follow-up observations are required to monitor for recurrences after surgery.
Figures and Tables
Fig. 1
Gigantomastia in a 43-year-old woman. Patient before reduction mammaplasty: (A) frontal and (B) lateral view.

References
1. Taylor CJ, Chester DL. Bilateral breast reduction surgery in elderly women: a retrospective review of outcomes. J Plast Reconstr Aesthet Surg. 2012; 65:304–311.
2. Beischer NA, Hueston JH, Pepperell RJ. Massive hypertrophy of the breasts in pregnancy: report of 3 cases and review of the literature, 'never think you have seen everything'. Obstet Gynecol Surv. 1989; 44:234–243.
3. Dancey A, Khan M, Dawson J, Peart F. Gigantomastia: a classification and review of the literature. J Plast Reconstr Aesthet Surg. 2008; 61:493–502.
4. Skillman J, Beechey-Newman N, Hamed H. Gigantomastia unrelated to pregnancy or puberty: a case report. Breast. 2002; 11:179–180.
5. Chrominski W, Madej B, Maciejewski R, Torres K, Ciechanek R, Burdan F. A developmental anomaly of the mammary glands - gigantomastia. A case report. Folia Morphol (Warsz). 2003; 62:517–518.
6. Ship AG. Virginal and gravid mammary gigantism: recurrence after reduction mammaplasty. Br J Plast Surg. 1971; 24:396–401.
7. Shoma A, Elbassiony L, Amin M, Zalata K, Megahed N, Elkhiary M, et al. "Gestational gigantomastia": a review article and case presentation of a new surgical management option. Surg Innov. 2011; 18:94–101.
8. Wolner-Hanssen P, Palmer B, Sjoberg NO, Astedt B. Gigantomastia. Acta Obstet Gynecol Scand. 1981; 60:525–527.
9. Lanzon AE, Navarra SV. Gigantomastia in a patient with systemic lupus erythematosus successfully treated by reduction mammoplasty. Lupus. 2009; 18:1309–1312.
10. Sakai T, Fujimori M, Tominaga Y, Kanai T, Ito K, Shingu K, et al. A case of unilateral gravid macromastia in 23-year-old Japanese woman associated with elevated serum CA19-9. Breast Cancer. 2005; 12:238–242.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download