This article has been corrected. See "Erratum: Changes in the Prevalence of Childhood Asthma in Seoul from 1995 to 2008 and Its Risk Factors" in Volume 3 on page 283.
Abstract
Purpose
To investigate the prevalence of asthma and determine its risk factors in elementary school students in Seoul.
Methods
A modified International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire was used to survey 4,731 elementary school students from five areas in Seoul between April and October, 2008.
Results
In elementary school children, the lifetime and recent 12-month prevalence of wheezing were 11.7% and 5.6%, respectively. The lifetime prevalence of asthma diagnosis was 7.9%, and the recent 12-month prevalence of asthma treatment was 2.7%. Male sex (adjusted odds ratio [aOR], 1.90; 95% confidence interval [CI], 1.36-2.66), history of atopic dermatitis (AD) (aOR, 2.76; 95% CI, 1.98-3.84), history of allergic rhinitis (AR) (aOR, 3.71; 95% CI, 2.61-5.26), history of bronchiolitis before 2 years of age (aOR, 2.06; 95% CI, 1.39-3.07), use of antibiotics during infancy for >3 days (aOR, 1.88; 95% CI, 1.35-2.62), parental history of asthma (aOR, 2.83; 95% CI, 1.52-5.27), exposure to household molds during infancy (aOR, 1.84; 95% CI, 1.18-2.89), and the development or aggravation of asthma symptoms within 6 months after moving to a new house (aOR, 11.76; 95% CI, 5.35-25.86) were the independent risk factors for wheezing within 12 months.
Conclusions
The prevalence of wheezing and asthma in elementary school students in 2008 was similar to that in the past decade. Male sex, history of AD, history of AR, history of bronchiolitis before 2 years of age, parental asthma, use of antibiotics during infancy, exposure to molds in the house during infancy, and development or aggravation of asthma symptoms within 6 months after moving to a new house, could be risk factors for wheezing within 12 months.
Bronchial asthma is caused by a combination of genetic and environmental factors, and presents with various symptoms and signs such as cough, wheezing, dyspnea, and chest tightness.1 The prevalence of asthma has increased for several decades, particularly in childhood,2 and it is the most common chronic disease in children and adolescents. To elucidate the mechanisms of asthma and other allergic diseases and to develop methods for reducing their prevalence, it is necessary to understand their accurate prevalence, their natural course, and their risk factors.
The International Study of Asthma and Allergies in Childhood (ISAAC), which Korea joined in 1995, has enabled us to compare prevalence between countries. According to the third ISAAC study in 2005, the prevalence of asthma and asthma symptoms increased in most countries that showed a low prevalence in 1995, whereas it remained stationary or dropped in most countries that had shown a high prevalence.3 Korea has participated in three ISAAC surveys: two nationwide surveys in 1995 and 2000, and one regional survey in Seoul City in 2005. The second survey results have recently been reported.4 According to the survey results of Seoul City, the last 12-month prevalence of wheezing decreased from 10.5% in 1995 to 5.2% in 2000, and then to 5.5% in 2005; the lifetime prevalence of asthma diagnosis has been relatively constant: 8.7% in 1995, 9.4% in 2000, and 7.6% in 2005.4-6
Risk factors for asthma include sensitization to airborne allergens during infancy, history of atopic dermatitis or allergic rhinitis, maternal smoking during pregnancy, exposure to secondhand smoking, viral lower respiratory infections, air pollution, and various genetic polymorphisms.7 In Korea, the first and second ISAAC surveys demonstrated that risk factors for asthma are obesity, secondhand smoking, diet patterns, raising pets, fever in infancy, and the use of antibiotics.4 However, because these were large-scale but cross-sectional studies, prospective cohort studies on growth patterns from prenatal through postnatal periods are needed to elucidate accurate risk factors.
This study was conducted as the Seoul City project of "Atopy-Free Seoul." We determined the prevalence of wheezing and asthma among elementary school children in five areas of Seoul, and compared it to the results reported by the 1995, 2000, and 2005 ISAAC surveys in Korea. In addition, we compared the prevalence among the aforementioned five areas and investigated the risk factors for wheezing and asthma.
This study recruited a total of 5,036 students (from first to sixth grade) from five elementary schools that were randomly selected from five areas of Seoul City (central, northeast, southeast, southwest, and northwest) After the students underwent physical examination, 4,731 responded to a questionnaire (response rate, 93.9%). There were 752 children in the downtown area, 1,376 in the southeastern area, 769 in the southwestern area, 1,028 in the northwestern area, and 806 in the northeastern area. Of the 4,731 respondents, 4,554 (2,317 [50.9%] boys and 2,237 [49.1%] girls) were ultimately included in the study.
A modified ISAAC questionnaire was used. The questionnaire consisted of three main items: 1) general characteristics including name, sex, date of birth, height, and weight; 2) history of symptoms related to asthma, allergic rhinitis, atopic dermatitis, allergic conjunctivitis, and food allergy; and 3) environmental factors associated with allergic diseases. After the content of the questionnaire was explained to the parents or guardians of the students, written consent was obtained. The parents or guardians completed the questionnaires, and we collected them. This study was approved by the Institutional Review Board of Asan Medical Center, University Ulsan College of Medicine, Seoul, Korea.
The prevalence of the following cases were determined: 1) those that experienced one or more wheezing episodes in their lifetime; 2) those that experienced one or more wheezing episodes within 12 months of the survey; 3) those that were diagnosed with asthma in their lifetime; and 4) those that received treatment within 12 months of the survey. The prevalence was compared in terms of age, sex, and geographical area. Current asthma was defined when children had been diagnosed with asthma in their lifetime and experienced wheezing within 12 months of the survey.
Comparisons were made in terms of sex, age, school grade, and geographical area between the children using the χ2 test. In the risk factor analysis, adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were obtained using logistic regression analysis. All statistical analyses were performed using SPSS version 14.0 (SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant.
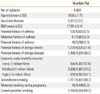
The mean age of the children was 9.50±1.73 years. There were 2,317 boys and 2,237 girls with a male to female ratio of 50.9:49.1. The parental history of asthma was 3.1%. A history of allergic rhinitis (AR) and any allergic disease (asthma, AR, or atopic dermatitis [AD]) was noted in 31.8% and 36.2% of the parents, respectively. Exposure to secondhand smoking was observed in 38.7% of the children (Table 1).
The lifetime prevalence of wheezing was 11.7%, and the last 12-month prevalence was 5.6%. The lifetime prevalence of asthma diagnosis was 7.9%, and the last 12-month prevalence of asthma treatment was 2.7%. The prevalence of current asthma was 2.5%. Prevalence of wheezing and asthma was higher in male than in female subjects (Table 2).
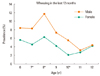
The last 12-month prevalence of wheezing increased from 7.0% (males, 8.4%; females, 5.6%) at age 6 years and 6.5% (males, 8.3%; females, 4.5%) at age 7 years to 9.0% (males, 11.7%; females, 6.3%) at age 8 years. Thereafter, it decreased to 5.8% (males, 7.3%; females, 4.2%) at age 9 years, to 3.8% (males, 5.5%; females, 2.1%) at age 10 years, and then to 2.9% (males, 3.2%; females, 2.7%) at age 11 years. There were significant differences in the prevalence at ages 7, 8, and 10 years between the sexes (Figure).
The lifetime prevalence of wheezing was highest in the north-east area (14.1%, 89/632) and lowest in the southwest (8.7%, 54/621), with a significant difference (P=0.006). However, there were no significant differences in the prevalence of the last 12-month wheezing and asthma treatment, lifetime prevalence of asthma diagnosis, and prevalence of current asthma between the five areas (Table 3).
The independent risk factors for the last 12-month wheezing were male sex (aOR, 1.90; 95% CI 1.36-2.66), history of AD (aOR, 2.76; 95% CI, 1.98-3.84), history of AR (aOR, 3.71; 95% CI, 2.61-5.26), history of bronchiolitis before 2 years of age (aOR, 2.06; 95% CI, 1.39-3.07), use of antibiotics during infancy for >3 days (aOR, 1.88; 95% CI, 1.35-2.62), parental history of asthma (aOR, 2.83; 95% CI, 1.52-5.27), exposure to household molds during infancy (aOR, 1.84; 95% CI, 1.18-2.89), and development or aggravation of asthma symptoms within 6 months after moving to a new house. The risk for the last 12-month wheezing in older children was lower than that in younger children (aOR, 0.83; 95% CI, 0.75-0.91) (Table 4).
The lifetime prevalence of wheezing decreased from 19.3% in 1995 to 14.4% in 2000, but it was constant in 2005 and 2008 (13.0% and 11.7%, respectively), with no significant differences compared to the data from 2000. The last 12-month prevalence of wheezing decreased from 10.5% in 1995 to 5.2% in 2000, but it was relatively constant thereafter (5.5% in 2005, 5.6% in 2008). However, the lifetime prevalence of asthma diagnosis was 8.7% in 1995, and 9.4% in 2000, and then it decreased to 7.6% in 2005 and 7.9% in 2008 compared to the data from 2000. The last 12-month prevalence of asthma treatment showed similar trends, such as 3.5% in 1995, 3.3% in 2000, 3.0% in 2005, and 2.7% in 2008 (Table 5).
According to the 1995 and 2005 ISAAC survey results, the prevalence of asthma varied among countries. The prevalence of asthma in 2005 increased in most countries that showed a low prevalence in the 1995 survey, whereas it was remained constant or decreased slightly in most countries that showed a high prevalence in the 1995 survey.3 As for Asian countries, in Japan, the last 12-month prevalence of wheezing was constant at 17.4% in 1995 and 18.2% in 2005.3 Also in Taiwan, it was 9.6% in 1995 and 9.8% in 2005, which is not a significant difference.3 As for European countries, in the Ukraine, it was 12.2% in 1995 and 12.5% in 2005, which was similar to the results reported in Korea.3 In Russia, it was 11.1% in 1995 and 11.4% in 2005, which is not a significant difference.3 In Korea, the nationwide prevalence of asthma decreased from 13.3% in 1995 to 5.8% in 2005.3 The last 12-month prevalence of wheezing confined to Seoul City decreased from 10.5% in 1995 to 5.2% in 2000 and 5.5% in 2005 according to the 1995, 2000, and 2005 ISAAC surveys,6 and it was 5.6% according to our study, which suggests that the last 12-month prevalence of wheezing decreased markedly after 1995, but there was no significant change in the prevalence of asthma after 2000 in Seoul, Korea. We cannot determine the reason for these changes, but this result may be attributed to measurement errors according to survey time or differences in public information and understanding of asthma and allergic diseases. Considering that there was no significant difference in the last 12-month prevalence of wheezing between the 2000, 2005, and 2008 surveys, and also no difference in doctor-related prevalence, such as the prevalence of diagnosis or last 12-month treatment among the 1995, 2000, 2005, and 2008, the last 12-month prevalence of wheezing in 1995 appears to have been overestimated. In addition, it is possible that because patients received medication, such as inhalation agents, regularly through public information activities and education by academic societies and various institutions after the 1995 survey, the last 12-month wheezing was successfully controlled. In Korea, wheezing symptoms appeared to decrease due to changes in social conditions and air pollution, as well as underestimated answers to the questionnaire from increased mother's social activities in the 2000s. Further studies are needed to confirm our results.
In the ISAAC survey, parents answered the questionnaire based on their memories, and therefore, recall biases should be considered when interpreting the answers. In fact, there is a discrepancy between actual bronchial hyperresponsiveness and the prevalence of asthma obtained by a questionnaire.8,9 Furthermore, such discrepancy can be induced by differences in the methods of a questionnaire survey, which should be improved for future ISAAC surveys.10,11
In the present study, it was found that prevalence of wheezing and asthma in elementary school students in Seoul City was significantly higher in male than in female subjects. Previous studies have demonstrated that asthma develops more frequently in male subjects before adolescence and in females after adolescence, and that these differences become smaller after menopause without any change in sexual predilection.12-17 In addition, it is generally known that in childhood, bronchial hyperresponsiveness to methacholine is higher in boys than in girls. Although this difference has been shown to correlate with changes in anatomical structures from birth through adolescence and differences in growth hormone levels, its exact mechanisms have not yet been elucidatied.18,19
The prevalence of allergic diseases tends to be lower in rural areas, which may have high exposure rates to microbial environments, than in urban areas.20 Moreover, the prevalence of allergic diseases varies among urban areas due to differences in socioeconomic status, concentrations of indoor allergens, and the level of atopy.21 In our study, lifetime prevalence of wheezing was lower in the downtown and southwestern areas than in the other areas, which suggests that there may be differences in socioeconomic status, life environments/traffic conditions, and effective medical care among the areas. However, our results should be interpreted carefully because the response rate to the questionnaire was significantly lower in the downtown area (82.0%).
A recent Tucson cohort study demonstrated that risk factors for chronic asthma from childhood through adulthood are wheezing after age 3 years, sensitization to Alternaria at age 6 years, bronchial hyperresponsiveness, and decreased pulmonary function at age 6 years, and that independent risk factors for newly diagnosed asthma at age 22 years are hyperresponsiveness and decreased pulmonary function at age 6 years, late-onset wheezing after age 3 years, and early persistent wheezing from under age 3 to age 6 years.22 Thus, because asthma develops in infancy, the asthma predictive index (API) is very useful for evaluating risk factors for asthma after infancy.23 In the modified API, history of AD, parental asthma, and sensitization to aeroallergens have been suggested as major risk factors.24 In our study, history of AD and parental asthma were independent risk factors for wheezing within 12 months. Our finding that the risk for asthma was higher in male than in female subjects might have been due to a higher prevalence of asthma and bronchial hyperresponsiveness before adolescence.18,19 In our study, a history of bronchiolitis before age 2 years was a risk factor for wheezing and asthma. A previous investigation proposed that a history of respiratory syncytial virus bronchiolitis in infancy is a risk factor for asthma.25 More work is currently being carried out on the interactions between genes and viruses in patients with recurrent virus-induced wheezing.26
Many epidemiological studies have shown that, after exposure to microbial environments during infancy, T-helper 2 immune responses are inhibited and T-helper 1 immune responses are induced with subsequent prevention of allergic diseases, whereas the excessive use of antibiotics during infancy alters the intestinal flora with subsequent reduction in the preventive effect.27,28 The 2000 ISAAC survey conducted in Korea found that the use of antibiotics during infancy is an independent risk factor for allergic disease.29 Similarly, our study showed that the use of antibiotics for ≥3 days was an independent risk factor for wheezing within 12 months. Some investigations have indicated that there is no significant correlation between the use of antibiotics and the development of asthma.28 Further studies are warranted.
Maternal smoking during pregnancy might be related to decreased pulmonary function and the development of asthma in children.30 Exposure to secondhand smoke might correlate with the prevalence, severity, and acute exacerbation of asthma, and the number of visits to the emergency department.31 However, in this study, there was no significant association between secondhand smoke and the last 12-month wheezing or current asthma. Although asthma is reported to occur more frequently as the degree of exposure to secondhand smoke increases, the cutoff value of exposure to smoke has not yet been determined. Therefore, complete avoidance of secondhand smoke is mandatory.31 In this study, the last 12-month prevalence of wheezing was significantly related to the development or aggravation of asthma symptoms within 6 months after moving to a new house. This result implies that components released from construction material and wallpaper aggravate asthma symptoms.32 To elucidate the relationship between asthma symptoms and materials in new houses, more research into environmental factors is warranted.
In a recent meta-analysis, dampness and mold in homes were associated with a variety of respiratory outcomes including wheezing and asthma.33 Also in our study, early childhood exposure to molds was a significant risk factor for wheezing in primary school children. Indoor molds such as Aspergillus or Penicillium are important aeroallergens. However, because early exposure to fungal agents such as extracellular polysaccharides from Aspergillus or Penicillium might protect against asthma,34 further investigations about the effect of molds on the development of asthma are needed.
The main difference in the study populations of the present study and the ISAAC surveys is that all of the students from the first to sixth grade of elementary school were included in the present survey, whereas only first-grade students were included in the ISAAC studies. The present study focused on elementary school students using a questionnaire that was answered by their parents or guardians through recall; therefore, there could be discrepancies between the actual prevalence and our data. These points should be considered in the interpretation of the results. Additional biological indicators, including bronchial provocation, hematological, and skin prick tests, should be performed to compare accurately the actual prevalence with the results of the questionnaire studies.
The primary limitation of this study is that, because it was conducted as the Seoul City project of "Atopy-Free Seoul," its prevalence did not represent nationwide prevalence. However, the results of this study can be used as reference data for the following reasons: 1) a relatively large number of children were surveyed; 2) the response rate was relatively high; 3) first to sixth grade elementary school children were included; and 4) the population of Seoul City is approximately 30% of the total population of Korea. More information on asthma in school-age children can be obtained by conducting continual longitudinal studies at regular intervals, along with follow-up studies. Prospective cohort studies with a large sample size based on such longitudinal study results are required to determine accurate risk factors for asthma.
Figures and Tables
Figure
Prevalence of wheezing according to age and gender during the last 12 months before the survey. *P value <0.05 in comparison between males and females.
ACKNOWLEDGMENTS
This study was supported by the "Atopy-Free Seoul Project" of the Seoul Metropolitan Government. The authors would like to thank all of the study participants, their parents, and their school teachers, all joint research workers, and the ISAAC epidemiological survey committee of the Korean Academy of Pediatric Allergy and Respiratory Disease, as well as In Guk Kim, director of the Songpa-gu Community Health Center, for his assistance with school recruitment.
References
1. Panettieri RA Jr, Covar R, Grant E, Hillyer EV, Bacharier L. Natural history of asthma: persistence versus progression-does the beginning predict the end? J Allergy Clin Immunol. 2008. 121:607–613.
2. Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006. 355:2226–2235.
3. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, Williams H. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006. 368:733–743.
4. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008. 51:343–350.
5. Lee SI. Prevalence of childhood asthma in Korea: international study of asthma and allergies in childhood. Allergy Asthma Immunol Res. 2010. 2:61–64.
6. Hong SJ. Epidemiology of childhood asthma and allergic diseases. Pediatr Allergy Respir Dis. 2007. 17:Suppl 1. S55–S66.
7. Arruda LK, Solé D, Baena-Cagnani CE, Naspitz CK. Risk factors for asthma and atopy. Curr Opin Allergy Clin Immunol. 2005. 5:153–159.
8. Pattemore PK, Asher MI, Harrison AC, Mitchell EA, Rea HH, Stewart AW. The interrelationship among bronchial hyperresponsiveness, the diagnosis of asthma, and asthma symptoms. Am Rev Respir Dis. 1990. 142:549–554.
9. Dales RE, Ernst P, Hanley JA, Battista RN, Becklake MR. Prediction of airway reactivity from responses to a standardized respiratory symptom questionnaire. Am Rev Respir Dis. 1987. 135:817–821.
10. Hong SJ, Kim SW, Oh JW, Rah YH, Ahn YM, Kim KE, Koh YY, Lee SI. The validity of the ISAAC written questionnaire and the ISAAC video questionnaire (AVQ 3.0) for predicting asthma associated with bronchial hyperreactivity in a group of 13-14 year old Korean schoolchildren. J Korean Med Sci. 2003. 18:48–52.
11. Lai CK, Chan JK, Chan A, Wong G, Ho A, Choy D, Lau J, Leung R. Comparison of the ISAAC video questionnaire (AVQ3.0) with the ISAAC written questionnaire for estimating asthma associated with bronchial hyperreactivity. Clin Exp Allergy. 1997. 27:540–545.
12. Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, Scalia MR, Akinbami LJ. National surveillance for asthma--United States, 1980-2004. MMWR Surveill Summ. 2007. 56:1–54.
13. Anderson HR, Pottier AC, Strachan DP. Asthma from birth to age 23: incidence and relation to prior and concurrent atopic disease. Thorax. 1992. 47:537–542.
14. Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax. 1999. 54:1119–1138.
15. de Marco R, Locatelli F, Sunyer J, Burney P. Differences in incidence of reported asthma related to age in men and women. A retrospective analysis of the data of the European Respiratory Health Survey. Am J Respir Crit Care Med. 2000. 162:68–74.
16. Luyt DK, Burton PR, Simpson H. Epidemiological study of wheeze, doctor diagnosed asthma, and cough in preschool children in Leicestershire. BMJ. 1993. 306:1386–1390.
17. Venn A, Lewis S, Cooper M, Hill J, Britton J. Questionnaire study of effect of sex and age on the prevalence of wheeze and asthma in adolescence. BMJ. 1998. 316:1945–1946.
18. Peat JK, Salome CM, Woolcock AJ. Factors associated with bronchial hyperresponsiveness in Australian adults and children. Eur Respir J. 1992. 5:921–929.
19. Le Souéf PN, Sears MR, Sherrill D. The effect of size and age of subject on airway responsiveness in children. Am J Respir Crit Care Med. 1995. 152:576–579.
20. Alfvén T, Braun-Fahrländer C, Brunekreef B, von Mutius E, Riedler J, Scheynius A, van Hage M, Wickman M, Benz MR, Budde J, Michels KB, Schram D, Ublagger E, Waser M, Pershagen G. Allergic diseases and atopic sensitization in children related to farming and anthroposophic lifestyle--the PARSIFAL study. Allergy. 2006. 61:414–421.
21. Kitch BT, Chew G, Burge HA, Muilenberg ML, Weiss ST, Platts-Mills TA, O'Connor G, Gold DR. Socioeconomic predictors of high allergen levels in homes in the greater Boston area. Environ Health Perspect. 2000. 108:301–307.
22. Stern DA, Morgan WJ, Halonen M, Wright AL, Martinez FD. Wheezing and bronchial hyper-responsiveness in early childhood as predictors of newly diagnosed asthma in early adulthood: a longitudinal birth-cohort study. Lancet. 2008. 372:1058–1064.
23. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med. 2000. 162:1403–1406.
24. Guilbert TW, Morgan WJ, Zeiger RS, Bacharier LB, Boehmer SJ, Krawiec M, Larsen G, Lemanske RF, Liu A, Mauger DT, Sorkness C, Szefler SJ, Strunk RC, Taussig LM, Martinez FD. Atopic characteristics of children with recurrent wheezing at high risk for the development of childhood asthma. J Allergy Clin Immunol. 2004. 114:1282–1287.
25. Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B. Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am J Respir Crit Care Med. 2000. 161:1501–1507.
26. Singh AM, Moore PE, Gern JE, Lemanske RF Jr, Hartert TV. Bronchiolitis to asthma: a review and call for studies of gene-virus interactions in asthma causation. Am J Respir Crit Care Med. 2007. 175:108–119.
27. Foliaki S, Pearce N, Björkstén B, Mallol J, Montefort S, von Mutius E. Antibiotic use in infancy and symptoms of asthma, rhinoconjunctivitis, and eczema in children 6 and 7 years old: International Study of Asthma and Allergies in Childhood Phase III. J Allergy Clin Immunol. 2009. 124:982–989.
28. Marra F, Lynd L, Coombes M, Richardson K, Legal M, Fitzgerald JM, Marra CA. Does antibiotic exposure during infancy lead to development of asthma?: a systematic review and metaanalysis. Chest. 2006. 129:610–618.
29. Ahn KM, Lee MS, Hong SJ, Lim DH, Ahn YM, Lee HR, Lee MI, Lee MH, Shin YK, Kim KE. Fever, use of antibiotics, and acute gastroenteritis during infancy as risk factors for the development of asthma in Korean school-age children. J Asthma. 2005. 42:745–750.
30. Gilliland FD, Berhane K, Li YF, Rappaport EB, Peters JM. Effects of early onset asthma and in utero exposure to maternal smoking on childhood lung function. Am J Respir Crit Care Med. 2003. 167:917–924.
31. DiFranza JR, Aligne CA, Weitzman M. Prenatal and postnatal environmental tobacco smoke exposure and children's health. Pediatrics. 2004. 113:1007–1015.
32. Redlich CA, Sparer J, Cullen MR. Sick-building syndrome. Lancet. 1997. 349:1013–1016.
33. Fisk WJ, Lei-Gomez Q, Mendell MJ. Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air. 2007. 17:284–296.
34. Douwes J, van Strien R, Doekes G, Smit J, Kerkhof M, Gerritsen J, Postma D, de Jongste J, Travier N, Brunekreef B. Does early indoor microbial exposure reduce the risk of asthma? The Prevention and Incidence of Asthma and Mite Allergy birth cohort study. J Allergy Clin Immunol. 2006. 117:1067–1073.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download