Abstract
Gastric tuberculosis accounts for approximately 2% of all cases of gastrointestinal tuberculosis. Diagnosis of gastric tuberculosis is challenging because it can present with various clinical, endoscopic, and radiologic features. Tuberculosis manifesting as a gastric subepithelial tumor is exceedingly rare; only several dozen cases have been reported. A 30-year-old male visited emergency room of our hospital with hematemesis and melena. Abdominal CT revealed a 2.5 cm mass in the gastric antrum, and endoscopy revealed a subepithelial mass with a visible vessel at its center on gastric antrum. Primary gastric tuberculosis was diagnosed by surgical wedge resection. We report a rare case of gastric tuberculosis mimicking a subepithelial tumor with acute gastric ulcer bleeding.
Gastric tuberculosis is extremely rare even in countries with a high prevalence of tuberculosis. Although difficult to determine with certainty, gastric tuberculosis constitutes around 2% of gastrointestinal tuberculosis cases.12 Its most common symptoms are nonspecific and indistinguishable from those of other ulcerative and obstructive gastric diseases, such as peptic ulcer, neoplasm, and Crohn's disease.3 The ulcerative and hypertrophic infiltrative types of gastric tuberculosis are most frequently encountered endoscopically,4 and few cases of gastric tuberculosis mimicking a subepithelial tumor have been reported.5678 It is important that gastric tuberculosis be differentiated from other tumorous conditions because antitubercular treatment is effective against the former but not the latter. We report a case of gastrointestinal bleeding caused by primary gastric tuberculosis presenting as a subepithelial tumor that was diagnosed by surgical resection and provide a review of relevant literature.
A 30-year-old male visited emergency department of our hospital due to hematemesis and melena, which had developed the previous day. His vital signs were: body temperature 36.4℃, respiration rate 20 breaths/min, pulse rate 120/min, and blood pressure 90/60 mmHg. A physical examination demonstrated anemic conjunctiva but without palpable lymph nodes or a mass on his body. Laboratory investigations revealed a low hemoglobin level (9.2 g/dL) and a slightly elevated CRP level (3.02 mg/dL). Other laboratory test results were within normal limits.
Contrast-enhanced abdominal CT revealed a 2.5 cm relatively well-defined soft tissue mass on the anterior wall of the gastric antrum (Fig. 1A, B), an enlarged lymph node with peripheral rim enhancement and a hypodense center in the periportal area (Fig. 1A), and low attenuating masses with thickened walls in both subphrenic spaces (Fig. 1B). In addition, a CT scan of the chest revealed airspace consolidation in the right lower lobe (Fig. 1C).
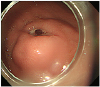
At endoscopy, a smooth protruding mass with central ulceration and a visible vessel was observed in the gastric antrum along the greater curvature (Fig. 2). The mass was not soft when pressed with forceps and had a negative rolling sign. Active bleeding from the mass was not observed. We decided to resect the gastric subepithelial tumor for diagnostic and therapeutic purposes because we could not rule out the possibility of malignancy. Exploratory laparotomy revealed a subepithelial mass on the greater curvature of the gastric antrum, which was subjected to wedge resection. Whitish miliary nodules were observed in peritoneum and omentum and biopsied for histopathologic examination.
Gross inspection of the surgical specimen revealed a well-defined subepithelial mass with central ulceration and intact surrounding overlying mucosa (Fig. 3A). Histopathologic examination demonstrated chronic granulomatous inflammation with caseating necrosis consistent with tuberculosis (Fig. 3B). The histopathologic findings of the whitish nodules were similar to those of the gastric mass.
Gastrointestinal tuberculosis is a rare manifestation of tuberculosis that is most frequently encountered in the ileocecal region. Other sites of involvement include, in descending order of frequency, the ascending colon, jejunum, appendix, duodenum, stomach, sigmoid colon, and rectum.9 The rarity of gastric tuberculosis may be due to the bactericidal activity of gastric acid, resistance of gastric mucosa to tubercular infection, scarcity of lymphoid tissue in gastric mucosa, and rapid gastric emptying.10 The incidence of gastric involvement in patients with tuberculosis is approximately 2%.12 The mucosal layer of the gastrointestinal tract may be infected following ingestion of contagious material, such as sputum or milk containing Mycobacterium bovis or Mycobacterium tuberculosis, whereas the most common route of gastric infection is lymph nodal spread via adjacent lymph nodes.6 The majority of cases of gastric tuberculosis are associated with pulmonary tuberculosis and its incidence depends on the severity of pulmonary involvement.11
The common clinical presentations of gastric tuberculosis are non-specific, with complaints of epigastric pain, vomiting, and weight loss.6 Morphologically, there are various types of gastric involvement, but ulcerative is the most common and constitutes approximately 80% of cases, because caseous necrosis of tubercles in lymphoid tissue of submucosa leads to ulceration of overlying mucosa.4 Ulcers rarely penetrate beyond submucosa or the muscle layer. Generally, tuberculosis manifesting as gastric ulcer does not perforate or bleed. As the disease progresses, fibrosis and necrosis may lead to transformation to the less common hypertrophic infiltrating type, which in appearance mimics scirrhous gastric cancer.4
Gastric tuberculosis presenting as a subepithelial tumor has only been rarely reported,5678 and the underlying mechanism is unclear. According to Shibagaki et al.,12 granuloma formation and liquefactive necrosis of caseating lesions may lead to subepithelial mass formation in patients with tuberculosis. In some reports, gastric tuberculosis manifesting as a subepithelial tumor was found to be caused by a tuberculous lymph node eroding the gastric wall.1314 Endoscopic ultrasonography is the modality of choice for evaluating gastric subepithelial masses as it facilitates the determination of layer of origin, classification, differential diagnosis, and follow up. However, endoscopic ultrasonography may depict gastric tuberculosis as hypoechoic lesions within the muscularis propria that are indistinguishable from gastrointestinal stromal tumors (the most common gastric mesenchymal tumors).6 Given its rarity, varied clinical presentations, and lack of specific endoscopic or radiological features, the correct diagnosis of gastric tuberculosis is difficult.
Histopathologic confirmation of tuberculosis remains a challenge. The presence of acid-fast bacilli in endoscopic biopsies or surgical specimens leads to a definitive diagnosis of gastric tuberculosis, but acid-fast bacilli are observed in only one-third of cases. However, in the absence of acid-fast bacilli, the presence of caseating granuloma may be considered diagnostic. According to the criteria proposed by Paustian and Marshall,15 the presence of at least one of the following findings is indicative of intestinal tuberculosis; caseating granuloma, acid-fast bacilli, or positive bacterial cultures.
Although it is difficult to diagnose, some have suggested the possibility of tuberculosis should be considered when an ulcer exhibits no therapeutic response or a tuberculous lesion is present at another site.16 In our case, pulmonary and abdominal lesions were presumed to be tuberculosis. Antitubercular agents are the mainstay of treatment. Surgery is frequently required for complications such as pyloric obstruction, perforation, bleeding, and fistula17 and should be followed by treatment with an antituberculosis drug regimen.
In conclusion, although gastric tuberculosis can manifest in various ways, its presentation as a subepithelial tumor, as in our case, is rare. However, physicians should be aware of the possibility of gastric tuberculosis in patients with tuberculosis in other organ(s), especially in lungs. We report an unusual case of gastric tuberculosis mimicking subepithelial tumor on endoscopic and imaging studies that was ultimately diagnosed histopathologically following surgical resection.
Figures and Tables
Fig. 1
(A) Axial contrast-enhanced CT image revealed a relatively well-defined soft tissue mass (arrow) on the anterior wall of antrum and an enlarged lymph node with peripheral rim enhancement and a hypodense center (arrowhead) in the periportal area. (B) Coronal reformatted contrast-enhanced CT scan showing low attenuating masses with thickened walls (arrowheads) in both subphrenic spaces and an exophytic, enhancing mass in gastric antrum (arrow). (C) CT images taken with lung window setting showing airspace consolidation (arrow) in the right lower lobe. CT, computed tomography.

References
1. Singh V, Jain AK, Agrawal AK, et al. Clinicopathological profile of abdominal tuberculosis. Br J Clin Pract. 1995; 49:22–24.
2. Subei I, Attar B, Schmitt G, Levendoglu H. Primary gastric tuberculosis: a case report and literature review. Am J Gastroenterol. 1987; 82:769–772.
3. Petroianni A, Mugnaini L, Laurendi G, et al. Abdominal tuberculosis mimicking Crohn's disease: a difficult diagnosis. Report of a case. Panminerva Med. 2002; 44:155–158.
4. Talukdar R, Khanna S, Saikia N, Vij JC. Gastric tuberculosis presenting as linitis plastica: a case report and review of the literature. Eur J Gastroenterol Hepatol. 2006; 18:299–303.

5. Rana SS, Bhasin DK, Srinivasan R, Singh K. Gastric outlet obstruction caused by tuberculosis and diagnosed by endoscopic ultrasound-guided fine needle aspiration. Endoscopy. 2011; 43:Suppl 2 UCTN. E117–E118.

6. Kim SH, Park JH, Kang KH, et al. Gastric tuberculosis presenting as a submucosal tumor. Gastrointest Endosc. 2005; 61:319–322.

7. Gupta V, Goel MM, Noushif M, Rai P, Gupta P, Chandra A. Primary gastric tuberculosis mimicking gastrointestinal stromal tumor. Am J Gastroenterol. 2012; 107:1269–1270.

8. Ardengh JC, Vaiciunas S, Kemp R, Venco F, Lima-Filho ER, dos Santos JS. Upper endoscopy versus endosonography in differential diagnosis of gastrointestinal bulging. Arq Gastroenterol. 2011; 48:236–241.

9. Kruijshaar ME, Abubakar I. Increase in extrapulmonary tuberculosis in England and Wales 1999–2006. Thorax. 2009; 64:1090–1095.

10. Tromba JL, Inglese R, Rieders B, Todaro R. Primary gastric tuberculosis presenting as pyloric outlet obstruction. Am J Gastroenterol. 1991; 86:1820–1822.
11. Mitchell RS, Bristol LJ. Intestinal tuberculosis: an analysis of 346 cases diagnosed by routine intestinal radiography on 5,529 admissions for pulmonary tuberculosis, 1924–49. Am J Med Sci. 1954; 227:241–249.
12. Shibagaki K, Miyaike J, Onji M, et al. Submucosal tumor-like lesion originating from colon tuberculosis: a case report and review of the literature. Clin J Gastroenterol. 2015; 8:207–211.

13. Kim DY, Bang S, Park BK, et al. Tuberculous mesenteric lymphadenitis involving the gastric wall: case report. Gastrointest Endosc. 2005; 62:799–802.

14. Lee TH, Cho JY, Bok GH, Cho WY, Jin SY. Intra-abdominal tuberculous lymphadenitis diagnosed using an endoscopic ultrasonography-guided Procore needle biopsy. Clin Endosc. 2013; 46:77–80.

15. Paustian FF, Marshall JB. Intestinal tuberculosis. In : Berk JE, editor. Gastroenteroscopy. Volume 3. 4th ed. Philadelphia: WB Saunders;1985. p. 2018–2036.
17. Rao YG, Pande GK, Sahni P, Chattopadhyay TK. Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg. 2004; 47:364–368.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download