Abstract
Background/Aims
Recently, variable gastrointestinal track tumors including early stage malignancies are treated by endoscopic procedure. However, the discrepancy of histologic diagnosis may sometimes exist between the pretreatment forceps biopsy results and those of post treatment specimen. So the prediction of malignant lesion is important in the aspect of treatment selection. In this study, we investigated the predictable factors of the histologic discrepancy through the clinical, endoscopic features of the lesion diagnosed as adenocarcinoma in the post-endoscopic treatment specimen after the adenoma was diagnosed by the endoscopic forceps biopsy.
Methods
From March 2005 to April 2009, 129 gastric tumor lesions (129 patients) which were not diagnosed as malignancy and treated with endoscopic procedure were enrolled retrospectively. We compared the pretreatment endoscopic forceps biopsy results and post-treatment specimen biopsy results, then, analyzed the tumor characteristics.
Results
Twenty-one cases (16.3%) were diagnosed as malignancy after endoscopic treatment. Especially, discrepancy occurred more frequently in depressed lesions than in flat or elevated lesions (41.7% vs. 13.7%, p=0.012), and in lesions diagnosed as high grade adenomas than low or moderate grade adenomas (33.3% vs. 11.1%. p=0.004).
Conclusions
In cases of depressed type lesions in the pretreatment endoscopy or those diagnosed as high grade adenoma in the pretreatment forceps biopsy, we should consider combined malignant lesion. Therefore, treatment modalities ensuring accurate diagnosis and potentially curative resection, should be carefully selected and performed in cases which have these features.
Gastric adenoma is defined as a raised lesion composed of dysplastic epithelium that is flat-topped, villiform, or forms a pedunculated polyp.1 Adenomas are reportedly associated with synchronous gastric carcinomas with varying frequencies, ranging from 8% to 59%. The reported incidence of carcinoma arising within adenomas also varies considerably, from 4% to 60%.2 In 1963, early gastric cancer (EGC) was defined as adenocarcinoma confined to the mucosa or submucosa, irrespective of lymph node involvement.1 Surgical resection was once considered to be the only curative standard procedure for gastric cancer.3 However, EGC that is smaller than 2 cm and limited to the mucosal layer rarely involves lymph node metastasis.4 In countries with a high prevalence of EGC, such as Japan and Korea, the focus of treatment is therefore shifting from radical curative procedures to new technologies that allow for a better quality of life. Endoscopic mucosal resection (EMR) of superficial early cancers of the upper gastrointestinal tract and gastric adenoma is thus a standard technique in Japan. The use of EMR is increasing in other developed countries. The treatment indications of EMR are further extended by endoscopic submucosal dissection (ESD).4
Reliable histological results from forceps biopsies with regard to the entire lesion are essential to making accurate diagnoses and appropriate therapeutic decisions. While vigorous efforts have been made to improve diagnostic rates for gastric adenomas and EGC through new technologies (such as magnifying endoscopy, autofluorescence imaging, infrared imaging, and narrow-band imaging), discrepancies remain between pre-endoscopic and post-endoscopic resection diagnoses.5 In addition, endoscopic forceps biopsy sampling often yields tissue that is inadequate for accurate histological diagnosis, and the foci of dysplasia may not be identified.6-8
In several previous studies, diagnosis of gastric epithelial neoplasms using tissues from endoscopic forceps biopsy versus post-endoscopic specimens has shown discrepancy rates of 25-35%.9,10 Detailed pathological examination of resected specimens may permit refinement of the diagnosis made via histological examination of forceps-biopsied samples, allowing more accurate prognosis determination. However, application of EMR/ESD for all gastric adenomatous lesions would excessively increase the time and cost of care, possibly limiting the number of patients who could be candidates for these procedures. Therefore, if we could identify factors predictive of discrepancies between endoscopic forceps-biopsied and post-endoscopic treatment specimens, EMR/ESD could be efficiently performed in properly selected cases.
To this end, we retrospectively reviewed patients whose lesions were diagnosed as non-malignant by forceps biopsies and were subsequently treated with EMR or ESD. We then investigated the factors predictive of a histologic discrepancy between forceps-biopsied and post-endoscopic treatment specimens. We analyzed the cases that were diagnosed as adenoma using specimens obtained by forceps biopsy, but as adenocarcinomas by using endoscopically resected specimens.
From March 2005 to April 2009, 129 patients with a total of 129 gastric adenomatous lesions were enrolled retrospectively. All enrolled patients had an initial diagnosis that was not carcinoma and all were diagnosed and treated with endoscopic procedures. Pre-treatment forceps biopsies were performed by 5 gastroenterologists using biopsy forceps (MTW Endoscopie, Goldsbergstrasse, Germany). We classified the biopsy sites as nodular elevated, flat, or depressed mucosal lesions compared to the surrounding mucosa. We obtained at least 3 pieces of the lesion by forceps biopsy. We analyzed characteristics of the patients such as gender and age, and the size, type, site and histologic features of the lesions. Paris classification of gastric neoplastic lesions was used to classify the gross tumors as type 1 (protruded), type 2a (superficial elevated), type 2b (flat), type 2c (superficial depressed), or type 3 (excavated). Types 1, 2a, and a combination of these 2 types, such as type 1+2a and 2a+2c, were classified as the elevated type. Type 2c and 3 lesions and combined lesions, such as type 2c+2a, were classified as the depressed type. A type 2b lesion was classified as the flat type.11 This study was approved by the Seoul Veterans Hospital Institutional Review Board.
EMR/ESDs were performed in a single center (Seoul Veterans Hospital). Pharyngeal anesthesia was induced with lidocaine, and sedation was induced with midazolam. After the precise margin of the lesion was established by chromoendoscopy (flexible spectral imaging color enhancement [FICE]), specimens were sprayed with 0.1-0.5% Indigo carmine dye and marked with electrocautery using a needle knife (MTW Endoscopie) or argon plasma coagulation. Hypertonic saline mixed with epinephrine (5-30 mL) was injected into the submucosal layer to produce a mucosal bleb. The lesion was incised (precut) along the outer border of the marked lesion using a needle knife. EMR/ESD was carried out with inject-and-cut or cap-fitted methods.12,13 The lesion was then resected with a snare (EMR, 4 cases) or dissected (ESD, 125 cases) with a flexible knife (Kachu Technology, Seoul, Korea), IT knife (MTW Endoscopie), or a needle knife. During the procedure, a high-frequency generator (VIO 300D; ERBE Elekromedizin, Tubingen, Germany) was used as the electrosurgical unit. Resected specimens were washed in normal saline, oriented using small pins, fixed in 8% buffered formaldehyde solution, and embedded in paraffin. The tissues were sliced into 2-mm sections and submitted for histologic diagnosis. After EMR/ESD, the patients participated in sucralfate and proton pump inhibitor therapy. Aspirin or other anticoagulant treatment was discontinued 7 days before the procedure and re-introduced 7 days after the procedure.
One pathologist reviewed the specimens obtained by forceps biopsy and EMR/ESD. The diagnosis was determined on the basis of the Vienna classification system for gastric dysplasia and carcinoma.14 Gastric adenomas were characterized by mild architectural complexity with glands lined by crowded, elongated cells that had hyperchromatic and basilar pseudostratified nuclei. High-grade dysplasia presented with more architectural abnormalities that involved gland branching and budding. The diagnosis of an intramucosal carcinoma required a high nuclear grade and either a prominent back-to-back or syncytial growth pattern, abortive microglands, or small clusters of epithelial cells within the lamina propria between glands. The combined findings of adenoma and carcinoma were classified as a carcinoma.
Pearson's chi-square test was performed to compare the EMR/ESD histological results with other clinical features such as patient age and gender, tumor size, type, site, and pre-treatment forceps biopsy results. Multivariate analysis was performed for the evaluation of factors predictive of histologic discrepancy using a logistic regression model. Analysis was performed with SPSS 10.1 for Windows (SPSS Inc., Chicago, IL, USA). A p-value of 0.05 or less was considered statistically significant.
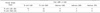
Using endoscopic forceps-biopsied specimens, 99 (76.7%) of the enrolled cases were diagnosed as adenoma with low or moderate grade dysplasia and 30 (23.3%) as adenoma with high grade dysplasia (Table 1).
ESD was used to treat 125 cases (96.9%), and 4 cases (3.1%) were treated with EMR with a snare (EMR-p). When we compared the post-treatment histologic results with the pre-treatment diagnosis, histologic discrepancies were found in 21 cases (16.3%).
Most of the patients were male, and there was no difference between the groups with respect to gender (2/12, 16.7% vs. 19/117, 16.2%) (p=0.970). The mean age of enrolled patients was 69 years (range, 38-85 years), and 82.9% of the patients (107/129 lesions) were over 60 years of age. Although histologic discrepancies were found more frequently in patients over 60 years of age (20/107, 18.7%) than those under 60 (1/22, 4.5%), this finding was not statistically significant (p=0.102) (Table 2).
The size, site, and endoscopic features of the lesions were analyzed (Table 1). Of the 129 lesions studied, 99 (76.7%) were smaller than 2 cm and 30 (23.3%) were larger than 2 cm. Histologic discrepancies were more frequent in the group of lesions below 2 cm (18/99, 18.2%) than in the group of lesions above 2 cm (3/30, 10.0%), although this result was statistically insignificant (p=0.288) (Table 2). With regard to endoscopic features of the lesions, 117 (90.7%) were of the flat or elevated type and 12 (9.3%) were of the depressed type. Histologic discrepancies were significantly more frequent in the depressed type lesions (5/12, 41.7%) than in those of the flat or elevated type (16/117, 13.7%; p=0.012). In other words, the depressed type lesions might have a higher risk of containing malignant components even in cases diagnosed as premalignant lesions before treatment (Table 2). Most of the lesions were located in the lower third of the stomach (120 lesions, 93.0%). Two (1.6%) and 7 (5.4%) cases were located in the upper and mid-third of the stomach, respectively. Histologic discrepancies were more frequent in the group with lesions in the lower third (20/120, 16.7%) than in the group with lesions in the mid-third of the stomach (1/7, 14.3%). None of the lesions in the upper third showed histologic discrepancies. There was no statistical difference between the groups (p=0.810) (Table 2).
Using forceps-biopsied specimens, pre-treatment diagnosis classified 99 lesions (76.7%) as adenoma with a low or moderate grade and 30 lesions (23.3%) as adenoma with high grade dysplasia (Table 1). Histologic discrepancies were more frequent in lesions diagnosed as adenoma with high grade dysplasia (10/30, 33.3%) than in lesions diagnosed as low or moderate grade dysplasia (11/99, 11.1%; p=0.004) (Tables 2, 3).
On multivariate analysis, depressed type lesions (OR, 5.873; p=0.023) and a pretreatment histologic finding of high grade dysplasia (OR, 4.734; p=0.007) were also found to be meaningful predictive factors (Table 4). In short, lesion type and grade of dysplasia as determined by pretreatment forceps biopsy were factors predictive of histologic discrepancies between pre- and post-treatment diagnosis.
The prevalence of gastric adenomas varies widely in different populations. The reported prevalence is about 0.5% to 3.75% in Western countries and about 9% to 20% in Asian countries, where the prevalence of gastric cancer is high.15,16 Surgical resection had been considered to be the only curative, standard procedure for gastric cancer. After EMR and ESD were introduced in Japan, its use rapidly expanded to neighboring countries because of its safety, diagnostic and therapeutic efficacy, and minimal invasiveness.13,17,18 Currently, EMR and ESD are performed worldwide and are accepted as a treatment option for gastroesophageal mucosal lesions.18
The EMR/ESD procedure cannot be performed during a routine diagnostic endoscopy due to the relatively long length of the procedure and potential complication risks. Patients with cardiac and pulmonary compromise and those taking anticoagulants are at high risk for complications.19-21 Therefore, the risks and benefits must be considered before performing EMR/ESD in those cases. Clinicians can decide to perform the procedure based on the results of endoscopy and forceps biopsy results.22 However, it is well known that endoscopic mucosal biopsies obtained with standard biopsy forceps can yield false-negative results, especially if the transmural epithelial layer is not involved in the pathological process. Hidden foci of malignancy can be missed by forceps biopsy, also leading to false-negative results.
According to the results of several studies,23-26 the discrepancy rates between endoscopic forceps biopsied samples and post-treatment resected specimens are 10-25%. The concordance rate between endoscopic forceps biopsied samples and entirely resected specimens after ESD are reported to be low as 65-76% in Japan.9,27 EMR and ESD involve en bloc resection of the entire lesion, the histological examination of which is clearly more reliable than forceps biopsy. However, EMR and ESD are not frequently used for diagnostic purposes in developed countries.28
There are few studies on the factors predictive of this histologic discrepancy, especially regarding the diagnosis of malignancy. We therefore planned this study to determine whether there were factors predictive of this histologic discrepancy and to thus improve the management of gastric adenomatous lesions.
Of the 129 cases included in our retrospective study, 21 (16.3%) had histologic discrepancies between forceps biopsy samples and post- EMR/ESD specimens. In other words, some of the tumor lesions were misdiagnosed before treatment. Our study showed that the rate of histologic discrepancies was higher in depressed-type lesions and in those that involved high grade dysplasia. These results indicate that when gastric adenoma is found in combination with these features, treatment modalities assuring en bloc resection should be considered.
Our study has the following limitation. The possibility of selection bias resulted from the fact that consecutive cases were not analyzed, as this study was performed retrospectively. As such, a further large-scale prospective study is necessary to overcome this limitation.
In conclusion, our study suggests that depressed-type tumor morphology and high grade dysplasia are factors predictive of a histologic discrepancy between diagnostic forceps biopsy results and post-treatment specimen diagnosis of gastric adenomatous lesions in terms of malignancy. Therefore, treatment modalities ensuring accurate diagnosis and potentially curative resection, such as ESD, should be carefully selected and performed in cases that involve these features.
Figures and Tables
References
1. Goldstein NS, Lewin KJ. Gastric epithelial dysplasia and adenoma: historical review and histological criteria for grading. Hum Pathol. 1997. 28:127–133.
2. Park DI, Rhee PL, Kim JE, et al. Risk factors suggesting malignant transformation of gastric adenoma: univariate and multivariate analysis. Endoscopy. 2001. 33:501–506.
3. Kim JJ, Jung HC, Song IS, et al. Preoperative evaluation of the curative resectability of gastric cancer by abdominal computed tomography and ultrasonography: a prospective comparison study. Korean J Intern Med. 1997. 12:1–6.
4. Kim YD, Cho JY, Jung IS, et al. Comparison of endoscopic forcep biopsy and the histopathologic diagnosis after endoscopic submucosal dissection. Korean J Gastrointest Endosc. 2009. 38:188–192.
5. Rösch W, Elster K, Ottenjann R. Diagnosis of gastric polyps by means of endoscopic biopsy. Minerva Med. 1972. 63:4145–4147.
6. Remmele W, Kolb EF. Malignant transformation of hyperplasiogenic polyps of the stomach-case report. Endoscopy. 1978. 10:63–65.
7. Ginsberg GG, Al-Kawas FH, Fleischer DE, Reilly HF, Benjamin SB. Gastric polyps: relationship of size and histology to cancer risk. Am J Gastroenterol. 1996. 91:714–717.
8. Muehldorfer SM, Stolte M, Martus P, Hahn EG, Ell C. Multicenter Study Group "Gastric Polyps". Diagnostic accuracy of forceps biopsy versus polypectomy for gastric polyps: a prospective multicentre study. Gut. 2002. 50:465–470.
9. Hansson LE, Lindgren A, Nyrén O. Can endoscopic biopsy specimens be used for reliable Laurén classification of gastric cancer? Scand J Gastroenterol. 1996. 31:711–715.
10. Palli D, Bianchi S, Cipriani F, et al. Reproducibility of histologic classification of gastric cancer. Br J Cancer. 1991. 63:765–768.
11. Participants in the Paris workshop. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003. 58:6 Suppl. S3–S43.
12. Tada M, Murakami A, Karita M, Yanai H, Okita K. Endoscopic resection of early gastric cancer. Endoscopy. 1993. 25:445–450.
13. Inoue H, Takeshita K, Hori H, Muraoka Y, Yoneshima H, Endo M. Endoscopic mucosal resection with a cap-fitted panendoscope for esophagus, stomach, and colon mucosal lesions. Gastrointest Endosc. 1993. 39:58–62.
14. Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000. 47:251–255.
15. Serck-Hanssen A. Precancerous lesions of the stomach. Scand J Gastroenterol Suppl. 1979. 54:104–105.
16. Zhang YC. Geographic pathology of gastric dysplasia in China. Semin Surg Oncol. 1994. 10:100–106.
17. Tada M, Murakami A, Karita M, Yanai H, Okita K. Endoscopic resection of early gastric cancer. Endoscopy. 1993. 25:445–450.
18. Lambert R. Treatment of esophagogastric tumors. Endoscopy. 2003. 35:118–126.
19. Kakushima N, Fujishiro M, Kodashima S, et al. Technical feasibility of endoscopic submucosal dissection for gastric neoplasms in the elderly Japanese population. J Gastroenterol Hepatol. 2007. 22:311–314.
20. Fujishiro M, Yahagi N, Kakushima N, et al. Successful nonsurgical management of perforation complicating endoscopic submucosal dissection of gastrointestinal epithelial neoplasms. Endoscopy. 2006. 38:1001–1006.
21. Kakushima N, Fujishiro M, Kodashima S, Muraki Y, Tateishi A, Omata M. A learning curve for endoscopic submucosal dissection of gastric epithelial neoplasms. Endoscopy. 2006. 38:991–995.
22. Jung MK, Jeon SW, Park SY, et al. Endoscopic characteristics of gastric adenomas suggesting carcinomatous transformation. Surg Endosc. 2008. 22:2705–2711.
23. Palli D, Bianchi S, Cipriani F, et al. Reproducibility of histologic classification of gastric cancer. Br J Cancer. 1991. 63:765–768.
24. Ichiyoshi Y, Toda T, Minamisono Y, Nagasaki S, Yakeishi Y, Sugimachi K. Recurrence in early gastric cancer. Surgery. 1990. 107:489–495.
25. Hakim NS, Sarr MG, van Heerden JA. Does endoscopy really help the surgeon evaluate gastric cancer? Can J Surg. 1989. 32:175–177.
26. Namieno T, Koito K, Higashi T, et al. Assessing the suitability of gastric carcinoma for limited resection: histologic differentiation of endoscopic biopsy. World J Surg. 1998. 22:865–868.
27. Habu H, Takeshita K, Sunagawa M, Endo M. Lymph node metastasis in early gastric cancer. Int Surg. 1986. 71:244–247.
28. Everett SM, Axon AT. Early gastric cancer in Europe. Gut. 1997. 41:142–150.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download