Abstract
The prevalence of metabolic syndrome (MetS) in Korea has been increasing in adults, as well as in adolescents. Recently the prevalence of MetS in children has been reported to strongly link that of MetS in parents. Families are known to share similar food environment so that eating habits of parents closely resemble that of the children's. Therefore, the aim of this study to examine metabolic risk factors and dietary intake in children by with respect to mother's metabolic syndrome, based on the data from Korean National Health and Nutrition Examination Survey (KNHANES) 2007-2010. Using the household variable and the eldest child per household, 1,341 pairs of mothers and children were selected. The mothers were defined by MetS criteria, and then the children were classified into the following three groups in accordance to the mothers' MetS; children whose mothers had none, 1-2, and 3 or more components of MetS. All dietary data were evaluated using the data from a food frequency questionnaire. The mean age was 42.6 ± 4.2 years for the mothers, and 14.9 ± 2.0 years for the children. Children whose mothers had 3 or more components of MetS showed a significantly higher prevalence of overweight and higher level of fasting triglyceride; conversely, they showed a lower level of serum HDL-cholesterol compared to the other two groups. Regarding an agreement of food consumption between the mothers and children, most food groups showed high agreement, except in the category of beverages. Regarding the dietary habits and family meals, children whose mothers had 3 or more components of MetS were more likely to skip breakfast and less likely to have family meals at breakfast or snack. In conclusion, the children's metabolic risk factors and dietary factors were different with respect to the status of mothers' MetS. Further studies are necessary to examine the causal effect of family environment in children's health status.
Figures and Tables
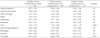
Table 2
The basic and metabolic syndrome characteristics in adolescent children by the status of mothers' metabolic syndrome

1) Defined by age and gender specifc BMI percentile in 2007 Korean Children and Adolescents Growth Standard. 2) HOMA-IR = [Fasting plasma glucose (mmol/L) × Fasting plasma insulin (µIU/mL)]/22.5 3) Mean values were significantly different after adjusted for children's age, BMI, and physical activity by Generalized Linear Model and mean values with different letters were tested by Duncan's multiple range test (NS: not significant).
References
2. Jung HJ, Song WO, Paik HY, Joung H. Dietary characteristics of macronutrient intake and the status of metabolic syndrome among Koreans. Korean J Nutr. 2011; 44(2):119–130.

3. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009; 32(11):2016–2020.
4. Park HS, Park JY, Cho SI. Familial aggregation of the metabolic syndrome in Korean families with adolescents. Atherosclerosis. 2006; 186(1):215–221.

5. Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, Choi SH, Cho SI, Park KS, Lee HK, Jang HC, Koh KK. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011; 34(6):1323–1328.
6. Chung JY, Kang HT, Shin YH, Lee HR, Park BJ, Lee YJ. Prevalence of metabolic syndrome in children and adolescents - the recent trends in South Korea. J Pediatr Endocrinol Metab. 2013; 26(1-2):105–110.

7. Cook S, Weitzman M, Auinger P, Nguten M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescent: findings from the third National Health and Nutrition Examination Survey 1998-1994. Arch Pediatr Adolesc Med. 2003; 157:821–827.
8. Kim JH, Lee GR, Chong CU. Metabolic syndrome and associated factors in Korean adolescents: 1998~2008 Korean National Health and Nutrition Examination Survey. Korean J Orient Prev Med. 2011; 15(1):89–98.
9. Baik I. Studies on dietary patterns in the prevention of metabolic syndrome. Food Ind Nutr. 2011; 16(2):45–48.
10. Choi MK, Jun YS, Bae YJ, Sung CJ. A study on nutrient intakes and blood parameters of adult men and women with metabolic syndrome. J Korean Soc Food Sci Nutr. 2007; 36(3):311–317.

11. Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am J Clin Nutr. 2006; 84(6):1489–1497.

12. Kim J. Dairy food consumption is inversely associated with the risk of the metabolic syndrome in Korean adults. J Hum Nutr Diet. 2013; 26:Suppl 1. 171–179.

13. Park J, Kweon S, Kim Y, Jang MJ, Oh K. Dietary behaviors related to metabolic syndrome in Korean adults. Korean J Community Nutr. 2012; 17(5):664–675.

14. Kim YJ, Lee JG, Yi YH, Lee SY, Jung DW, Park SK, Cho YH. The influence of breakfast size to metabolic risk factors. J Life Sci. 2010; 20(12):1812–1819.

15. Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr. 2010; 92(6):1316–1325.

16. Kim MS. Effects of mothers' dietary behavior on growth and nutrient intakes of elementary school children [dissertation]. Seoul: Kukmin University;2006.
17. Jung JY. Relationship between eating behaviors of parents and their adolescent children [dissertation]. Iksan: Wonkwang University;2010.
18. Timperio A, Salmon J, Ball K, Baur LA, Telford A, Jackson M, Salmon L, Crawford D. Family physical activity and sedentary environments and weight change in children. Int J Pediatr Obes. 2008; 3(3):160–167.

19. MacFarlane A, Cleland V, Crawford D, Campbell K, Timperio A. Longitudinal examination of the family food environment and weight status among children. Int J Pediatr Obes. 2009; 4(4):343–352.

20. Bauer KW, Berge JM, Neumark-Sztainer D. The importance of families to adolescents' physical activity and dietary intake. Adolesc Med State Art Rev. 2011; 22(3):601–613. xiii

21. Shin A, Lim SY, Sung J, Shin HR, Kim J. Dietary intake, eating habits, and metabolic syndrome in Korean men. J Am Diet Assoc. 2009; 109(4):633–640.

22. Na DW, Jeong E, Noh EK, Chung JS, Choi CH, Park J. Dietary factors and metabolic syndrome in middle-age men. J Agric Med Community Health. 2010; 35(4):383–394.
23. You MA, Son YJ. Prevalence of metabolic syndrome and associated risk factors among Korean adolescents: analysis from the Korean national survey. Asia Pac J Public Health. 2012; 24(3):464–471.
24. Kim HM, Park J, Kim HS, Kim DH. Prevalence of the metabolic syndrome in Korean adolescents aged 12-19 years from the Korean National Health and Nutrition Examination Survey 1998 and 2001. Diabetes Res Clin Pract. 2007; 75(1):111–114.

25. Yoo EG, Park SS, Oh SW, Nam GB, Park MJ. Strong parent-offspring association of metabolic syndrome in Korean families. Diabetes Care. 2012; 35(2):293–295.

26. Lee MH, Kim HC, Thomas GN, Ahn SV, Hur NW, Choi DP, Suh I. Familial concordance of metabolic syndrome in Korean population--Korean National Health and Nutrition Examination Survey 2005. Diabetes Res Clin Pract. 2011; 93(3):430–436.

27. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112(17):2735–2752.
28. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, Kim DY, Kwon HS, Kim SR, Lee CB, Oh SJ, Park CY, Yoo HJ. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75(1):72–80.

29. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28(7):412–419.
30. Hong S, Song Y, Lee KH, Lee HS, Lee M, Jee SH, Joung H. A fruit and dairy dietary pattern is associated with a reduced risk of metabolic syndrome. Metabolism. 2012; 61(6):883–890.

31. Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr. 2009; 12(2):267–283.

32. Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004; 113(1 Pt 1):112–118.

33. Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescentadolescents. J Am Diet Assoc. 2003; 103(3):317–322.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download