Abstract
It is thought that calcium (Ca) and magnesium (Mg) may be related to mental disorders such as depression; however, there have been few studies investigating the association between Ca and Mg nutrition status with depression in middle-aged female adults. Study subjects in this study included 105 women between the ages of 41 and 57 years. The subjects were divided into three groups according to the Zung Self-rating Depression Scale (SDS) score: Group I (SDS score < 33 percentile; n = 32), Group II (33 percentile ≤ SDS score < 67 percentile; n = 37), and Group III (67 percentile ≤ SDS score; n = 36). Anthropometric measurements, dietary intake survey using 3-day dietary records, SDS questionnaire and measurement of serum Ca and Mg were obtained and analyzed. No differences were observed in Ca, plant Ca, and Mg intake among the three groups. However, animal Ca intake by Group III was 141.3 mg, which was significantly lower than 207.6 mg by Group I and 198.3 mg by Group II (P = 0.0345). There were no significant differences in serum levels of Ca, and Mg among the three groups. Correlation analysis indicated that the SDS score had negative correlations with Ca intake (r = -0.2927, P < 0.01) and animal Ca (r = -0.3411, P < 0.001) after adjusting for age, menopause and energy intake. In conclusion, dietary Ca and animal Ca had negative associations with SDS score among middle-aged Korean female adults. Additional analysis of factors related to the association of calcium and magnesium nutritional status and depression is necessary.
Depression is an important cause of morbidity, and the World Health Organization (WHO) has predicted that depression will be the second leading contributor to the global burden of disease by 2020. Depressive symptoms are common symptoms impairing the quality of life of people, and it has been widely established that depression is more common for females (21%) than males (13%) [1].
Depression is caused by numerous factors, including age, dietary factors, menopause, alcohol drinking patterns and so on, which are thought to contribute negatively to depression [2-4]. There are several studies reporting that some nutrient and a number of herbal treatments have alleviating effects on depression and anxiety disorder symptoms [5,6]. In particular, there are studies about the association of nutritional status of vitamins and minerals, which contributes to various metabolic regulations of the body for patients with depression. In a cross-sectional study, it was reported that an inverse association of vitamin D intake from foods and the occurrence of depressive symptoms in older women aged 50-79 years [7]. Also, a nested case-control study suggested that lower dietary selenium intakes are associated with an increased risk of subsequent de novo major depressive disorder [8]. A randomized, double-blinded, placebo-controlled, crossover study conducted on average 32-year-old women concluded that supplying both vitamin B6 and magnesium relieved symptoms such as nervous tension, mood swings, irritability, or anxiety [9]; another study on adult men reported that supplement of oral multivitamins in combination with calcium, magnesium, and zinc had an effect on relieving anxiety and perceived stress [10].
There are researches reporting the effects of minerals such as calcium (Ca) and magnesium (Mg) on depression. Ca dysregulation is critical in nervous system disorders such as dementia and depression [11-15]. It is reported that in the hippocampus of a rat, the calcium/calmodulin-dependent protein kinase II mediates the activity of Group I metabotropic glutamate receptors (mGluRs) which derives the development of long-term depression [16]. Changes in extracellular Ca concentration could have stimulatory effects on neuromuscular junctions, and irritability, mania and agitation have been reported in conjunction with hypocalcemia [17]. It was reported that the low-depression-level group of pregnant women showed a significantly high level of total Ca and plant Ca intake compared to that of the high-depression-level group of pregnant women [18]. In another study which researched the effect of Ca supplement on premenstrual syndrome symptoms (PMS) of women in early adulthood, the depression level was markedly decreased compared to the placebo group when calcium carbonate was supplied 500 mg a day for 3 months. [19]. Accordingly, it is thought that Ca intake is related to depression and mental disorder, while there are only few studies which reports the association of Ca nutrition status with depression of pre- and post-menopause middle aged women.
Mg is a positively charged ion, a cation, which has been linked to anxiety-related disorders [20-22]. Mg is also a calcium antagonist and a voltage-dependant blocker of the N-methyl-D-aspartate channel, which plays a role in the entrance of calcium into neurons. In the case of adult women, the tertile group which had the lowest serum Mg concentration showed a significantly higher OR of depressive mood disorder compared to that of the highest tertile group with the highest serum Mg concentration. (OR = 3.92, 95% CI 1.11-13.83) [23]. In addition, a study conducted on adult women reported that Mg intake decreased OR of major depression/dysthymia remarkably (OR = 0.60, 95% CI 0.37-0.96) [24]. However, the data were inconsistent since both increases and decreases in blood and dietary Mg have been observed [25].
The role of several minerals has been recognized in depressive symptoms. Ca and Mg have been involved in depression; however there are few data on these mineral nutritional statuses concerning depression and data from human-studies are limited. The goal of the present study was to determine whether calcium and magnesium nutritional status is associated with depressive symptoms in elderly female individuals. For this study, 105 female were recruited and divided into three groups as related to their self-rated depression. The intake and serum levels of Mg and Ca was compared among groups that were divided by self-rated depression level, and then analyzed the relation of Mg and Ca nutrition status (dietary intakes, blood levels) with self-rated depression.
The study involved 105 females aged 41-57 years. Premenopausal women (n = 51) and postmenopausal women (n = 54) were recruited from Soonchunhyang University Hospital, South Korea between January and June 2006. The inclusion criteria were that subjects were in good apparent health and did not consume nutritional supplements or medications. After sufficiently explaining the objectives and details of this research, written informed consent was obtained from participants. After this, a questionnaire, dietary intake surveys and blood sampling were conducted on subjects.
Height was measured using a height-measuring instrument on which the subjects stood without shoes. Weight and percent of body fat were measured using InBody 3.0 (Biospace, Seoul, Korea) with survey targets dressed in light clothing. Body mass index was calculated as body weight in kilograms divided by height in meters squared. Waist circumference was measured at the smallest circumference between the rib cage and the iliac crest with the subject in standing position. All measurements were taken twice and the mean values were collected.
A dietary intake survey was conducted using the 3-day dietary records method through individual interview by trained researchers. That is, the types and quantities of all food items and food materials ingested as breakfast, lunch, dinner, and snacks from first awaking in the morning to bedtime at night on the day before the survey were investigated. Results of the dietary intake survey were analyzed in terms of the quantities of nutrient intake by using Can-Pro 3.0 (The Korean Nutrition Society, 2005). Magnesium intakes were calculated using magnesium contents databases produced by the food composition table of the National Rural Living Science Institute, Korea [26].
Depression symptoms were assessed with Self-rating Depression Scale (SDS) (Zung method), which comprises 20 items describing depression symptoms [27]. This self-completed questionnaire is in wide use and has been shown to have satisfactory reliability and validity. Respondents described how frequently they experienced each symptom on a 4-point scale: 'a little of the time', 'some of the time', 'good part of the time', or 'most of the time'. The frequency was converted into an integer between 1 and 4, and the total SDS score was calculated as the sum of the numbers obtained in response to the 20 questions. Zung SDS scores are interpreted as follows: < 50, within normal range; 50-59, minimal to mild depression; 60-69, moderate to severe depression; > 70, severe depression. In this study, 68.6% of the subjects were in the normal range, 21.0% in minimal to mild depression, 7.6% in moderate to severe depression, and 2.8% in severe depression. Like this, when self-rated depression of the subjects was classified according to the SDS score, the ratio of the subjects which belongs in normal range, minimal to mild, and moderate to serve depression group showed difference and accordingly the groups were classified by the tertile of SDS score. Therefore, the study subjects were divided into three groups according to the total SDS score: Group I (SDS score mean 36.2; n = 32), Group II (SDS score mean 44.4; n = 37), and Group III (SDS score mean 57.7; n = 36).
Blood samples were drawn in the morning after a 12-h overnight fast. The samples were left at room temperature for 30 min, centrifuged for 15 min at 3,000 rpm to separate serum, and then stored at -80℃. After wet decomposition with a microwave digestion system (Ethos 1600; Milestone Inc., Shelton, USA), the amounts of serum Ca, and Mg were analyzed using an inductively coupled plasma spectrometer (Thermo Jarrell Ash, MA, USA).
For all results obtained in this study, the mean and standard deviation values were calculated by the SAS program (version 9.2, SAS Inc., Cary, USA). For comparison among the three groups according to total SDS score (Group I: SDS score mean 36.2, Group II: SDS score mean 44.4, and Group III: SDS score mean 57.7), significance was verified by the one-way analysis of variance (ANOVA) test. When ANOVA indicated a significant difference among the means, the difference was further evaluated using Duncan's multiple range tests. To find out the relation between Ca, and Mg nutrition status with the depression symptom score, correlation coefficients analysis was performed. In addition, in the case of energy intake, age and menopause status, there was no significant difference in the self-rated depression score among groups, while it was reported to have effect in the precedent study. For that, a partial correlation analysis which adjusted energy intake, age, and menopause status was done. Multivariate logistic regression analysis was used to estimate the adjusted odds ratios (OR) and 95% confidence intervals of the calcium and magnesium nutrition status, predicting depression. All statistical significance verifications were conducted at the level of P < 0.05.
The general information of the subjects is shown in Table 1. The mean age of all the subjects was 48.9 years. The mean height, weight, BMI, percent body fat, and waist circumference were 156.3 cm, 60.9 kg, 25.0 kg/m2, 32.4% and 86.8 cm, respectively. However, there were no differences in weight, BMI, percent body fat, and waist circumference among the three groups. Group III had a larger proportion of subjects who were in menopause compared to other groups, but no significant difference was observed in the proportion subjects in menopause (P = 0.0683).
Energy and nutrients intakes per day by the subjects in each group are shown in Table 2. The mean energy intakes of the subjects were 1,491.0 kcal in Group I, 1,603.5 kcal in Group II, and 1,621.3 kcal in Group III. No significant difference was found in energy intake among the three groups. Also, no differences were observed in Ca, plant Ca, and Mg intakes among the three groups. However, animal calcium intake by Group III was 141.3 mg, which was significantly lower than 207.6 mg by Group I and 198.3 mg by Group II (P = 0.0345). The levels of serum Ca, and Mg in study subjects are shown in Fig. 1. There were no significant differences in serum levels of Ca, and Mg among the three groups.
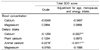
Pearson's partial coefficients of correlation among the depression scores, serum mineral concentrations and rnineral intakes are shown in Table 3. Correlation analysis indicated that SDS had negative correlations with calcium intake (r = -0.2927, P < 0.01), and animal calcium (r = -0.3411, P < 0.001) after adjusting for age, menopause and energy intake. Also, the levels of serum Ca, and Mg had no correlations with self-rated depression. The relationships between calcium and magnesium nutrition status (dietary intake and blood level) and the risk of self-rated depression are shown in Table 4. No significant association between serum Ca and Mg levels and the risk of self-rated depression was found. But total calcium intake was inversely associated with the risk of self-rated depression after adjusting for potential confounders (4th vs. 1st quartile, OR = 0.05, 95% CI = 0.01-0.34, P for trend = 0.0225). Also, animal calcium intake was inversely associated with the risk self-rated depression after adjusting for potential confounders (4th vs. 1st quartile, OR = 0.12, 95% CI = 0.03-0.54, P for trend = 0.0320).
To evaluate the association between calcium, magnesium nutritional status with depression of middle-aged women who are exposed to the risk of depression, serum calcium, magnesium concentrations, and its intakes by food was measured and compared by groups according to the self-rated depression scale scores. Various scales to measure the level of depression are reported, and among them there are the Beck Depression Inventory (BDI), Major Depression Inventory (MDI), Geriatric Depression Scale (GDS), Hamilton Depression Rating Scale (HDRS), Zung Self-Rating Scale for Depression (SDS) and so on. In this study, the Zung Self-Rating Scale for Depression (SDS) was used. Zung SDS comprises 20 items that measure effective, psychological and somatic symptoms related with depression, and is known for high reliability while showing a high interrelationship on the validity study of DSM classification (Diagnostic and Statistical Manual of Mental Disorders) [28,29]. Zung SDS scores are interpreted as follows: < 50, within normal range; 50-59, minimal to mild depression; 60-69, moderate to severe depression; > 70, severe depression. In this study, 68.6% of the subjects were in the normal range, 21.0% in minimal to mild depression, 7.6% in moderate to severe depression, and 2.8% in severe depression. When the subjects were divided into three groups according to the percentile of the SDS scores, all subjects of Group I and almost all of Group II (91.9%) belonged to the normal range.
Calcium functions as a neurotransmitter in body metabolism; and a causal link between disturbances in cellular calcium and effective disorders in mood has been proposed in the past. Changes in the extracellular calcium concentration may affect the excitability of neuromuscular tissues involved in emotional regulation [30]. However, most mental disorder studies related with calcium are about the relief of PMS symptoms [19,31,32]. Penland et al. [31] reported that high dietary calcium intake in the amount of 1,336 mg per day significantly benefited mood, behavior, pain and water retention symptoms during the menstrual cycle. In addition, in a case-controlled study nested within a prospective study, calcium intake by food was reported to have a significant negative correlation with PMS. In comparison with women with a low intake (median, 529 mg/d), participants with the highest intake (median, 1,283 mg/d) had a relative risk of 0.70 (95% confidence interval, 0.50-0.97) [33]. In this study, there were no significant differences of dietary total calcium intake among the groups which were divided by SDS scores, but the daily calcium intake of all subjects were 456.4 mg, which is similar to 458.9 mg, the calcium intake level of KNHANES female subjects aged 40-49 years [34].
In this study, by analyzing the relation of calcium intake and depression level of middle-aged women, higher total calcium and animal calcium intake were shown to significantly lower depression scores, and this remained consistent after adjusting for confounding factors such as age, menopause and energy intake. However, serum calcium concentration by groups according to the tertile of depression scores did not show meaningful differences. In a study conducted on 212 adults whose mean age were 60 (women 78%), the criteria of classifying depression symptoms, such Beck Depression Inventory-II, Brief Symptom Inventory-18, were investigated and analyzed the relations of serum calcium, intact parathyroid hormone (iPTH), and thyroid stimulating hormone. As a result, a high relation of the change of iPTH and depression symptom was shown, but relation with serum calcium was not observed which is consistent with the results of this study [35]. In this study, there were no subjects who were detected to be out of the normal range of serum calcium of 8.8~10.2 mg/dl [36], and considering the mechanism of serum calcium homeostasis in dynamic conditions, meaning continuous response to the inner-/outer changes [37], it appears that the subjects were able to keep their serum calcium concentration level in the normal range, maintained homeostasis, and showed no connection to depression regardless of the amount of calcium intake. Especially since vitamin D, parathyroid hormone and various factors maintain the calcium concentration in the body, a follow-up study about the relation between depression symptoms and factors with the effects of calcium concentration in the body of middle-aged women should be conducted.
Magnesium is a positively charged ion, a cation that is involved in many important molecular functions in the body, which has been linked to anxiety-related disorders [10,20-22,38]. There are studies reporting about the effect of magnesium mediation on relieving depression symptoms. In the study on 80 healthy men in the early adulthood, Mg, Ca, Zn and multivitamins were supplied together for 28 days. In the results, magnesium supply did not have a unilateral effect but showed a complex supplement led dramatic decrease of psychological distress [10]. In addition, when 44 women, whose mean age was 32, were supplied with magnesium, vitamin B6 for a month, a single supplement of magnesium showed a placebo effect on relieving PMS, but when the combination of magnesium and vitamin B6 was supplied, a significant synergistic effect was observed [9]. These findings are similar with the present study, which concluded that magnesium intake and depression level do not have a significant correlation.
Meanwhile, the mean daily supplement of magnesium in this study was 300.3 mg, which is slightly higher than the Recommended Nutrient Intake (RNI) level of adult women above 20 (280mg) on the Dietary Reference Intakes (DRI), meaning that magnesium intake was in good condition. A prior study about serum magnesium concentration and depression symptoms used the Hospital Anxiety Depression Scale and the Modified Brief Encounter Psychosocial Instrument Stress Scale on 126 adult women to classify and measure the depression level to observe the relation with magnesium. As a result, compared to the highest tertile group which had the highest serum Mg concentration, the group which had the lowest serum Mg concentration showed a significantly higher OR of depression mood disorder (OR = 3.92, 95% CI 1.11-13.83) [23]. This result is in disagreement with this main study, which did not observe significant difference of serum magnesium concentration by groups according to the depression symptoms. The discrepancy occurred by the different depression symptom classification criteria, but it seems that the normal magnesium concentration of the subjects in this study was also a cause [39].
In this study, self-rated depression level of middle-aged women and calcium intake was related. However, the calcium intake level was remarkably lower compared to DRI, and the depression level that was measured by Zung Self-Rating Scale for Depression (SDS) was not so severe, which may mean that these factors may affect the result of study. Also, in this study, the risk of self-rated depression according to the nutrition status of Ca and Mg was analyzed using logistic regression analysis, but the case numbers of subject classified as depression by Zung Self-Rating Scale for Depression (SDS) was less compared to the control group which made it difficult to bring a meaningful conclusion.
Accordingly, it is necessary to have a follow-up study about the association of calcium intake and depression using more various depression scales on women with adequate calcium intake amounts. In addition, in this study, magnesium intake and serum level does not show significant relation, but serum magnesium is affected by calcium, phosphorus and various minerals so it is thought that additional study considering these diet factors is necessary.
Figures and Tables
Fig. 1
The serum calcium (a) and magnesium (b) of three groups by self-rating depression scale (SDS) score. Significance as determined by ANOVA test according to the total SDS depression score risk score; No significant difference (α = 0.05)
Table 1
General characteristics of the subjects according to the total self-rating depression scale (SDS) score

Table 2
Daily intakes of energy and nutrients in the subjects according to the total self-rating depression scale (SDS) score

References
1. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003. 289:3095–3105.
2. Prado Jde A, Kerr-Corrêa F, Lima MC, da Silva GG, Santos JL. Relations between depression, alcohol and gender in the metropolitan region of São Paulo, Brazil. Cien Saude Colet. 2012. 17:2425–2434.

3. Bromberger JT, Kravitz HM. Mood and menopause: findings from the Study of Women's Health Across the Nation (SWAN) over 10 years. Obstet Gynecol Clin North Am. 2011. 38:609–625.

4. Exebio JC, Zarini GG, Exebio C, Huffman FG. Healthy Eating Index scores associated with symptoms of depression in Cuban-Americans with and without type 2 diabetes: a cross sectional study. Nutr J. 2011. 10:135.

5. Saeed SA, Bloch RM, Antonacci DJ. Herbal and dietary supplements for treatment of anxiety disorders. Am Fam Physician. 2007. 76:549–556.
6. Weeks BS. Formulations of dietary supplements and herbal extracts for relaxation and anxiolytic action: Relarian. Med Sci Monit. 2009. 15:RA256–RA262.
7. Bertone-Johnson ER, Powers SI, Spangler L, Brunner RL, Michael YL, Larson JC, Millen AE, Bueche MN, Salmoirago-Blotcher E, Liu S, Wassertheil-Smoller S, Ockene JK, Ockene I, Manson JE. Vitamin D intake from foods and supplements and depressive symptoms in a diverse population of older women. Am J Clin Nutr. 2011. 94:1104–1112.

8. Pasco JA, Jacka FN, Williams LJ, Evans-Cleverdon M, Brennan SL, Kotowicz MA, Nicholson GC, Ball MJ, Berk M. Dietary selenium and major depression: a nested case-control study. Complement Ther Med. 2012. 20:119–123.

9. De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000. 9:131–139.

10. Carroll D, Ring C, Suter M, Willemsen G. The effects of an oral multivitamin combination with calcium, magnesium, and zinc on psychological well-being in healthy young male volunteers: a double-blind placebo-controlled trial. Psychopharmacology (Berl). 2000. 150:220–225.

11. Konopka LM, Cooper R, Crayton JW. Serotonin-induced increases in platelet cytosolic calcium concentration in depressed, schizophrenic, and substance abuse patients. Biol Psychiatry. 1996. 39:708–713.

12. Demuro A, Mina E, Kayed R, Milton SC, Parker I, Glabe CG. Calcium dysregulation and membrane disruption as a ubiquitous neurotoxic mechanism of soluble amyloid oligomers. J Biol Chem. 2005. 280:17294–17300.

13. Doherty TM, Asotra K, Fitzpatrick LA, Qiao JH, Wilkin DJ, Detrano RC, Dunstan CR, Shah PK, Rajavashisth TB. Calcification in atherosclerosis: bone biology and chronic inflammation at the arterial crossroads. Proc Natl Acad Sci U S A. 2003. 100:11201–11206.

15. Plein H, Berk M, Eppel S, Butkow N. Augmented platelet calcium uptake in response to serotonin stimulation in patients with major depression measured using Mn2+ influx and 45Ca2+ uptake. Life Sci. 2000. 66:425–431.

16. Mockett BG, Guévremont D, Wutte M, Hulme SR, Williams JM, Abraham WC. Calcium/calmodulin-dependent protein kinase II mediates group I metabotropic glutamate receptor-dependent protein synthesis and long-term depression in rat hippocampus. J Neurosci. 2011. 31:7380–7391.

17. Jimerson DC, Post RM, Carman JS, van Kammen DP, Wood JH, Goodwin FK, Bunney WE Jr. CSF calcium: clinical correlates in affective illness and schizophrenia. Biol Psychiatry. 1979. 14:37–51.
18. Bae HS, Kim SY, Ahnv HS, Cho YK. Comparison of nutrient intake, life style variables, and pregnancy outcomes by the depression degree of pregnant women. Nutr Res Pract. 2010. 4:323–331.

19. Ghanbari Z, Haghollahi F, Shariat M, Foroshani AR, Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan J Obstet Gynecol. 2009. 48:124–129.

20. Durlach J, Pagès N, Bac P, Bara M, Guiet-Bara A. Importance of magnesium depletion with hypofunction of the biological clock in the pathophysiology of headhaches with photophobia, sudden infant death and some clinical forms of multiple sclerosis. Magnes Res. 2004. 17:314–326.
21. Abraham GE. Nutritional factors in the etiology of the premenstrual tension syndromes. J Reprod Med. 1983. 28:446–464.
22. German-Fattal M, Lecerf F, Sabbagh F, Maurois P, Durlach J, Bac P. Neuroprotective gene profile in the brain of magnesium-deficient mice. Biomed Pharmacother. 2008. 62:264–272.

23. Jung KI, Ock SM, Chung JH, Song CH. Associations of serum Ca and Mg levels with mental health in adult women without psychiatric disorders. Biol Trace Elem Res. 2010. 133:153–161.

24. Jacka FN, Maes M, Pasco JA, Williams LJ, Berk M. Nutrient intakes and the common mental disorders in women. J Affect Disord. 2012. 141:79–85.

25. Derom ML, Martínez-González MA, Sayón-Orea Mdel C, Bes-Rastrollo M, Beunza JJ, Sánchez-Villegas A. Magnesium intake is not related to depression risk in Spanish university graduates. J Nutr. 2012. 142:1053–1059.

26. Rural Resources Development Institute. Food Composition Tables. 2006. 7th edition. Seoul: Hyoil books.
28. Knight RG, Waal-Manning HJ, Spears GF. Some norms and reliability data for the State--Trait Anxiety Inventory and the Zung Self-Rating Depression scale. Br J Clin Psychol. 1983. 22:245–249.

29. Maes M, De Ruyter M, Claes R, Suy E. Self rated depression in relation to DSM-III classification: a statistical isolinear multiple components analysis. Acta Psychiatr Scand. 1988. 77:27–31.

30. Carman JS, Wyatt RJ. Calcium: bivalent cation in the bivalent psychoses. Biol Psychiatry. 1979. 14:295–336.
31. Penland JG, Johnson PE. Dietary calcium and manganese effects on menstrual cycle symptoms. Am J Obstet Gynecol. 1993. 168:1417–1423.

32. Khajehei M, Abdali K, Parsanezhad ME, Tabatabaee HR. Effect of treatment with dydrogesterone or calcium plus vitamin D on the severity of premenstrual syndrome. Int J Gynaecol Obstet. 2009. 105:158–161.

33. Bertone-Johnson ER, Hankinson SE, Bendich A, Johnson SR, Willett WC, Manson JE. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Arch Intern Med. 2005. 165:1246–1252.

34. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. 2009 National Health Statistics: The 4th Korea National Health and Nutrition Examination Survey, the third year. 2010. Cheongwon: Korea Centers for Disease Control and Prevention;239.
35. Roman SA, Sosa JA, Pietrzak RH, Snyder PJ, Thomas DC, Udelsman R, Mayes L. The effects of serum calcium and parathyroid hormone changes on psychological and cognitive function in patients undergoing parathyroidectomy for primary hyperparathyroidism. Ann Surg. 2011. 253:131–137.

36. Tietz NW. Fundamentals of Clinical Chemistry. 1987. 3rd edition. Philadelphia: W.B. Saunders.
37. Schuette SA, Linkswiler HM. Calcium. Present Knowledge in Nutrition. 1984. 15th edition. Washington D.C.: The Nutrition Foundation Inc.;400–412.
38. Fromm L, Heath DL, Vink R, Nimmo AJ. Magnesium attenuates post-traumatic depression/anxiety following diffuse traumatic brain injury in rats. J Am Coll Nutr. 2004. 23:529S–533S.

39. Aikawa JK. Magnesium: Its Biological Significance. 1981. Florida: CRC Press Inc..




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download