Introduction
Congestive heart failure (CHF) is a common clinical syndrome that results from a variety of disease processes in dogs, and a number of pharmaceuticals are used in the management of CHF cases. The standard treatment of CHF in dogs includes “triple therapy”, consisting of a combination of the diuretic furosemide, an angiotensin-converting enzyme (ACE) inhibitor (ACEI), and pimobendan [
1]. Benazepril (Fortekor; Elanco Animal Health, USA) is an ACEI that reduces concentrations of angiotensin-2 and aldosterone [
1416], while pimobendan (Vetmedin; Boehringer Ingelheim Vetmedica, Japan) is an inodilator that produces a combination of vasodilation via inhibition of phosphodiesterase III and inotropy through calcium sensitization [
6]. Benazepril and pimobendan, administered independently, have been shown to improve clinical signs and increase survival time in dogs with CHF caused by valvular disease [
3111518], and both drugs are registered in the European Union, Japan, and other countries for the treatment of CHF in dogs. Recently pimobendan was reported to prolong the preclinical period in dogs with myxomatous mitral valve disease (MMVD) [
5].
A consequence of the use of triple therapy is the need to administer at least three medicines orally to dogs with CHF. In human medicine, compliance in patients taking their medicines as directed is inversely related to the complexity of the regimen and the number of doses prescribed per day [
7]. Fixed-dose combination products have been shown to reduce the risk of non-compliance in humans, including those with cardiovascular disease, and a number of such products are available [
2].
Elanco Animal Health (Greenfield, USA) developed fixed-dose combination tablets of benazepril and pimobendan (Fortekor Plus; Elanco Animal Health) on the basis of the drugs' complementary therapeutic actions and in order to increase treatment compliance and ease animal handling. Fortekor Plus is available in two tablet sizes, containing 2.5 or 10 mg of benazepril hydrochloride and 1.25 or 5 mg of pimobendan, respectively. Benazepril (Fortekor) is registered to be administered once daily (SID) in a dosage range of 0.25 to 1.0 mg/kg, allowing a starting dosage of 0.25 to 0.5 mg/kg to be doubled to 0.5 to 1.0 mg/kg if needed. Pimobendan (Vetmedin) is registered in Japan at a dosage of 0.25 mg/kg twice daily (BID) with a range of 0.17 to 0.35 mg/kg on the dosage chart. Pimobendan must be administered BID due to its short half-life [
6]. Therefore, in the fixed-dose combination, benazepril is administered BID with no possible doubling of the dose.
The aim of the present study was to test the field efficacy and safety of Fortekor Plus tablets in dogs with CHF caused by MMVD and, specifically, to support the registration of Fortekor Plus in Japan. The first objective was to compare the effects of Fortekor Plus with those of a combination of Fortekor and Vetmedin. A second objective was to compare the effects of benazepril when dosed BID and SID. The study was a prospective, multi-center, parallel-group, three-arm, masked, randomized, non-inferiority design clinical trial.
Materials and Methods
The study was conducted in compliance with Good Clinical Practice guidelines [Ministry of Agriculture, Forestry and Fisheries, Japan, Ordinance nos. 75 (1997) and 36 (amendment 2005)]. The study protocol was reviewed and approved by the Elanco Animal Health Global Animal Welfare Officer (JPN-12-001). This manuscript was prepared after consulting the checklist in the extension of the CONSORT statement for reporting of non-inferiority trials [
17].
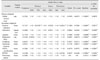
The study schedule is shown in
Table 1. Dogs were examined at day (D)0 and their case histories recorded. Animals were included in the study after confirmation of their eligibility and written owner consent had been obtained.
Inclusion criteria
Dogs with CHF associated with MMVD were recruited. All of the following criteria had to be present at baseline: 1) characteristic murmur associated with mitral regurgitation; 2) cardiac enlargement on chest X-ray; 3) modified New York Heart Association (NYHA) Functional Classification Class III or IV heart failure [
11]. Note that for NYHA Class III or IV, all dogs had to have clinical signs consistent with CHF and radiographic evidence of pulmonary edema; and 4) body weight ≥ 2.5 kg (to permit accurate dosing of the test articles).
Exclusion criteria
Dogs meeting any of the following criteria were not eligible for enrollment: 1) clinically relevant heart disease other than acquired MMVD (e.g., congenital heart disease). Note that dogs with tricuspid valve disease were also eligible provided that the primary cause of CHF was MMVD; 2) clinically relevant concurrent systemic disease judged likely to negatively affect the clinical status or survival of the dog in the next 3 months (e.g., diabetes mellitus, neoplasia, kidney or liver disease). Pre-renal azotemia was not considered an exclusion criterion; 3) clinically relevant gastrointestinal disease likely to affect the absorption of the test articles; 4) females that were pregnant, lactating, or intended for breeding; or 5) known sensitivity to benazepril or pimobendan.
Randomization
The dogs were randomized to one of three groups (
Table 2); investigational veterinary product (IVP), Control I, and Control II groups in a 2:1:1 ratio. Within groups, dogs were stratified according to previous treatment or no treatment with pimobendan. Separate randomization lists were generated for each site by a statistician. The block length for each stratum was 4 dogs.
Test articles
The IVP consisted of flavored tablets containing, respectively, 2.5/1.25 mg or 10/5 mg of benazepril hydrochloride/pimobendan (Fortekor Plus). The control products (CPs) consisted of flavored tablets containing 2.5 or 5 mg of benazepril hydrochloride (Fortekor 2.5 and 5 mg) or 1.25 or 5 mg of pimobendan (Vetmedin).
The IVP group received benazepril (0.25–0.5 mg/kg BID) and pimobendan (0.125–0.25 mg/kg BID) at dosages registered for Fortekor Plus in Japan (
Table 2). The Control II group received benazepril (starting dosage 0.25–0.5 mg/kg SID with the option to increase to 0.5–1.0 mg/kg SID if judged necessary by a veterinarian) and pimobendan (0.25 mg/kg BID) at the dosages registered in Japan. The Control I group received the same daily dosages as the Control II group; however, the benazepril was administered BID (0.125–0.25 mg/kg BID with the option to increase to 0.25–0.5 mg/kg BID).
All test articles were administered orally for 56 ± 3 days starting on D0. To be in compliance with the Vetmedin label, the IVP and CPs were administered at least 1 h before providing any feed. Drugs administered BID were given approximately 12 h apart.
If a dog was already receiving an ACEI or pimobendan or both at inclusion, then, for animal welfare reasons, those drugs were discontinued only on the day before starting treatment with IVP or CPs with no wash-out period.
Blinding
The IVP and CPs have different appearances and packaging. Masking of the investigators who made the clinical evaluations was achieved via the use of a dispenser at each site who dispensed the test articles to the owners, checked the owner dosing forms, and performed the reconciliation of products dispensed to and returned by the owners. Owner assessments were not blinded.
Concomitant treatments
Standard concomitant therapy for CHF (including furosemide, digoxin, spironolactone, and amlodipine) or treatments with no reported effect on the cardiovascular system (e.g., antiparasite agents, vaccines) were permitted throughout the study. With the exception of the IVP or CPs, the following were prohibited: pimobendan, levosimendan or similar inotropes or inodilators, benazepril or any other ACEI, angiotensin II receptor antagonists, renin inhibitors, and xanthines.
Follow-up
If enrolled into the study, the dogs were examined again at D7 ± 1, D14 ± 2, D28 ± 2 and D56 ± 3, and at the time of any premature withdrawal. On each examination day, a physical examination was performed, and body weight, rectal temperature, body condition score (BCS), and signs of CHF were recorded.
Cases could be prematurely withdrawn from the study for various reasons including adverse events (AEs) that were serious or could interfere with the evaluation of the test articles, major protocol deviations, or worsening of signs of CHF. Treatment failure was defined as the occurrence of: death or euthanasia; one or more of persistent dyspnea, progressive ascites, severe cachexia, or marked exercise intolerance, attributed to a cardiac cause, despite receiving or failing to tolerate furosemide (up to a maximum of 12 mg/kg/day orally) plus spironolactone (up to a maximum of 6 mg/kg/day orally) in addition to the test articles; or the need for additional cardiac medications not permitted in the protocol. The cause and the relationship or not to heart failure of any death or euthanasia were recorded, and it was noted if death was sudden or a result of progressive deterioration in the dog's health.
Efficacy assessment
Assessments were made at D0, D7 ± 1, D14 ± 2, D28 ± 2, and D56 ± 3, and at times of premature withdrawal.
The primary endpoint was the global clinical score (GCS), which was the unweighted sum of the numerical rating scale scores determined by the investigator for exercise tolerance (range, 1–4), demeanor (range, 1–4), appetite (range, 1–4), respiratory effort (range, 1–4), coughing (range, 1–4) and nocturnal dyspnea (range, 1–3) using the scoring schemes described by Häggström et al. [
11]. The GCS ranged from 6 to 23, with a lower score indicating milder signs of CHF.
Secondary endpoints were the investigators' assessments of individual parameters of the GCS [
11], the owners' assessment of functional evaluation of cardiac health (FETCH) score [
10], and the proportion of dogs with an improvement in modified NYHA classification score [
11]. In addition, right lateral and dorsoventral thoracic radiographs were taken at D0, D28 ± 2, and D56 ± 3, and assessments made of heart size and pulmonary edema using 1 to 4 scales. The pulmonary edema scoring scheme was 1 = none; 2 = mild interstitial opacity; 3 = moderate interstitial opacity; and 4 = alveolar pattern, severe consolidation [
11].
Safety assessment
Safety was assessed from the nature and occurrence of AEs. In addition, venous blood samples for routine hematology and clinical chemistry were taken on D0, D28 ± 2, and D56 ± 3 (and at the time of any premature withdrawal). Lastly, investigators examined the dogs at each visit and recorded general condition (appetite, vigor, and fecal consistency) and BCS using a 1 to 5 scale (cachectic, thin, optimal, overweight, or obese). If an arrhythmia was suspected on auscultation, an electrocardiogram was recorded.
Statistics
Data are presented as mean ± SD values or a range unless otherwise stated. All statistical tests were performed by using SAS software (ver. 8.2; SAS Institute, USA).
Groups were compared at baseline by performing analysis of variance (ANOVA) as appropriate for normally distributed data, or by using Mann-Whitney, Kruskal-Wallis, or Fisher exact probability tests.
Efficacy, clinical chemistry, and hematology variables were analyzed by using repeated measures analysis of covariance (RMANCOVA) with the following covariates: treatment; previous and concomitant treatment with ACEI, pimobendan, diuretic (spironolactone excluded), spironolactone or amlodipine; time in study (week), time × treatment interaction, and baseline. Since spironolactone and amlodipine treatments were in all cases continuations of previous therapy, use of each of these drugs was evaluated in a single category. Backward variable selection was employed so that if p > 0.1 for any covariate, the covariate with the highest p value was removed from the model, which was repeated until p values for all remaining covariates were < 0.1. Treatment and baseline value remained in the model regardless of their p values.
Variables were transformed (log or square root), if appropriate, to give the best estimate of a normal distribution, which was assessed by using the Shapiro-Wilk test. Non-inferiority for efficacy variables was concluded when the lower limit of the two-sided 95% confidence interval (CI) for the ratio of efficacy of IVP/Control was higher than 1–δ, with δ = 0.20. The selected δ was based on the assumption that a difference of 20% or less in clinical scores between groups would not be relevant clinically. As most variables deviated significantly from a normal distribution in the RMANCOVA analyses, groups were compared at each assessed time by using the non-parametric Mann-Whitney or Kruskal-Wallis tests. Change from baseline was assessed by using the Wilcoxon signed-rank test. The occurrence of AEs was compared between groups by using the Fisher exact probability test.
For efficacy and safety assessments, the IVP group was compared separately to each of the Control I and Control II groups. In addition, the two control groups were compared and, if there was no significant difference, results from the two groups were combined (denoted Control I + II) and compared to those of the IVP group.
All statistical tests were two-sided on a 5% level of significance (α = 0.05) with no correction for multiple analyses, in order not to inflate the type II error.
A minimum inclusion of 60 dogs was planned, as was required by the Japanese regulatory authorities.
Results
Animals
The biological phase of the study ran from November 2013 to September 2014. A total of 67 dogs were enrolled in the study across 16 sites in Japan and all were included in the demographic and safety analyses, representing an “all-randomized animals” dataset. Age, body weight, gender, and breed were similar in the three groups (
Table 3). A total of 15 breeds were included, the most common being Shih Tzu (n = 10), Cavalier King Charles Spaniel (n = 9), Chihuahua (n = 8), Maltese (n = 8), Miniature Dachshund (n = 5), and mixed breed (n = 10).
Two cases in the Control II group were removed from the efficacy dataset due to major protocol deviations (dosing of benazepril or pimobendan was ≤ 80% of scheduled). A total of 65 cases were therefore included in the efficacy dataset; all were fully compliant with the inclusion and exclusion criteria. Cases with missed doses (but with > 80% scheduled dosing) or minor deviations from examination and observation schedules occurred in all three groups and were included in the efficacy analyses.
For the efficacy dataset, there were no differences between groups for age, body weight, breed, diet, or gender (
p > 0.40, data not shown). At baseline, 56 dogs were in NYHA class III and 9 in class IV heart failure (
Table 4).
Concomitant treatments and test items
Prior to D0, 53 dogs (79.1%) had previously received an ACEI, 33 dogs (49.3%) pimobendan, 19 dogs (28.4%) a diuretic, and 4 dogs (6.0%) amlodipine (
Table 3). Six dogs had previously received ACEI, pimobendan, and diuretic, 12 ACEI and diuretic, 25 ACEI and pimobendan, 10 ACEI alone, 1 pimobendan alone, and 1 diuretic alone. With regard to ACEIs, dogs had received benazepril (n = 19), enalapril (n = 14), temocapril (n = 13), alacepril (n = 6), or ramipril (n = 1) (
Table 3). Mean (range) daily dosages in mg/kg/day administered prior to the study were: 0.59 (0.32–1.11) for benazepril, 0.75 (0.2–1.59) for enalapril, 0.16 (0.1–0.3) for temocapril, 3.4 (1.2–5.8) for alacepril, 0.1 (0.1–0.1) for ramipril, 0.53 (0.098–1.24) for pimobendan, and 0.38 (0.36–0.42) for amlodipine. Prior to the study, furosemide was used significantly more frequently in the Control I and II groups than in the IVP group.
The mean (range) dosages of benazepril and pimobendan administered during the study are shown in
Table 2. In the study, diuretics were used in 22 dogs (32.8%) and at similar dosages to those prior to enrollment in the study. The mean (range) daily dosages in mg/kg/day prior to and during the study were, respectively, 2.7 (0.44–4.8) and 3.0 (1.4–6.0) for furosemide and 0.19 (0.027–0.33) and 0.31 (0.1–0.55) for torasemide. Spironolactone was administered to 3 dogs (4.5%) at the same dosages (0.6, 1.33, and 1.95 mg/kg BID) before and during the study. Amlodipine was administered to 4 dogs (6.0%) at the same dosages (0.625 mg/kg BID n = 3, 1.25 mg/kg BID n = 1) before and during the study.
Withdrawal of cases from the study
Four cases were withdrawn from the study before the scheduled D56 visit, all related to death or worsening of CHF. All 4 dogs had NYHA Class IV CHF at baseline. The cases were withdrawn on D52 (death from acute pulmonary edema) and D40 (worsening of CHF) in the IVP group (n = 2, 5.9%), on D52 (death from worsening of CHF) in Control I (n = 1, 7.1%), and on D51 (death from bronchopneumonia secondary to pulmonary edema) in Control II (n = 1, 5.3%). The withdrawal frequency was not different between groups (
p = 0.98). Since all 4 cases that were prematurely withdrawn related to a lack of efficacy of the test articles, values for GCS, body weight, BCS, pulmonary edema score, and NYHA class at the time of withdrawal were used in the analyses at later times based on the last observation carried forward method [
13].
Primary endpoint: global clinical score
There was no significant difference between the Control I and Control II groups for GCS (
p = 0.46, RMANCOVA, data not shown) or any of the secondary variables; therefore, the two groups were combined to form the Control I + II group. There were significant decreases from baseline (D0) in GCS on all days (D7, D14, D28, and D56) in the IVP, Control II, and Control I + II groups (
Table 5).
The RMANCOVA results for GCS revealed a significant effect of baseline (
p < 0.0001) correlating with the change from baseline, but no significant effect of treatment, previous and/or concomitant use of ACEI, pimobendan, diuretic, spironolactone, or amlodipine, time, or time × treatment interaction (
Table 6). Although use of diuretics prior to the trial was significantly different between groups (
Table 3), this had no significant effect on any efficacy variable (
Table 6). The RMANCOVA results also demonstrated no significant differences in GCS between the IVP group and the Control I (
p = 0.91), Control II (
p = 0.17), and combined Control I + II (
p = 0.33) groups. There were also no significant differences at any assessment time detected in the non-parametric Mann-Whitney analyses (data not shown). Non-parametric analyses are relevant since distribution of the GCS data approached significance from normality in the RMANCOVA analysis (
p = 0.088;
Table 6).
Mean ± SD GCS scores at D0 and D56 were 12.1 ± 3.1 and 10.6 ± 3.6 in the IVP group; 11.5 ± 4.0 and 10.1 ± 4.1 in Control I; and 13.7 ± 5.0 and 10.1 ± 4.0 in Control II, respectively.
Results of the non-inferiority analysis are shown in
Table 7. Since the lower limit of the 95% CI for the ratio of efficacy of IVP/Control was higher than 0.80, non-inferiority of the IVP was demonstrated when compared to the Control I, Control II, and combined Control I + II groups.
Secondary efficacy endpoints
There were significant decreases from baseline (D0) in NYHA class, FETCH and pulmonary edema scores, as well as in some of the other variables in the IVP and control groups (
Table 5).
In the RMANCOVA analyses, no significant overall treatment effect for any secondary variable was detected (
Table 6). In the non-parametric analyses using the Mann-Whitney
U test, no statistically significant differences were observed for any of individual clinical scores, NYHA class, and the FETCH and pulmonary edema scores at any of the assessment times between the groups (IVP
vs. Control I, II, and I + II, and Control I
vs. II,
p > 0.05, data not shown). The results of the non-parametric analyses are relevant since the distributions of all 8 secondary variables deviated significantly from normality in the RMANCOVA analyses (
Table 6).
The NYHA classification distribution is shown in
Table 4; the improvement rate from baseline ranged from 35.7% to 58.8%. There was no significant treatment effect (
p = 0.56;
Table 6), and non-inferiority was shown for the IVP group
vs. Control I, II, and I + II groups (
Table 7).
With regard to pulmonary edema scores, there was a significant change (improvement) from D0 to both D28 and D56 in all groups: IVP from 2.24 ± 0.50 to 1.56 ± 0.61 and 1.65 ± 0.73; Control I from 2.29 ± 0.61 to 1.7 ± 0.61 and 1.57 ± 0.65; and Control II from 2.41 ± 0.71 to 1.41 ± 0.51 and 1.65 ± 0.79, respectively. There was no significant overall treatment effect (
p = 0.30;
Table 6), and non-inferiority was demonstrated for the IVP
vs. the Control I and combined Control I + II groups (
Table 7).
Safety
All 67 dogs in the all-randomized animal dataset were included in the safety analyses.
Adverse events: There were no significant differences between groups in the frequency of all AEs: 17 cases (50.0%) in the IVP group, 11 cases (78.6%) in Control I, 12 cases (63.2%) in Control II, and 23 cases (69.7%) in Control I + II (
Table 8).
The only AE with a significant difference between groups was emesis, which was significantly less frequent in the IVP group than in the Control I (p = 0.0034) and Control I + II (p = 0.0042) groups; significance was approached (p = 0.056) for the difference in emesis between the IVP and Control II groups. The number (%) of dogs with emesis was 3 (8.8%) in the IVP group, 7 (50.0%) in Control I, 6 (31.6%) in Control II, and 13 (39.4%) in Control I + II.
Clinical chemistry: With the exception of an effect on plasma glucose, there was no significant overall treatment effect or differences between the IVP and Control I or Control II groups for any clinical chemistry or hematology variable (data not shown). The p values for the overall treatment effect in the RMANCOVA model did not approach significance for the most clinically relevant variables: alanine aminotransferase (p = 0.80), creatinine (p = 0.68) or urea (p = 0.64). For potassium, there were numerically higher concentrations (mEq/L) in the Control I (5.1 ± 0.5) and Control II (5.0 ± 0.5) groups vs. the IVP group (4.9 ± 0.6), but the overall treatment effect was not significant (p = 0.12). For glucose, values (mg/dL) were significantly (p = 0.016) higher in the IVP group (92.9 ± 17.6) than in the Control II group (78.9 ± 15.4). Regardless, mean values for glucose and potassium remained within the reference range in all groups.
For plasma creatinine, the number of cases with increases from baseline by > 0.3 mg/dL, > 20%, or > 30% were calculated. There were no significant treatment effects or differences between groups. At day 28, the number of cases, respectively, in the IVP, Control I, and Control II groups with increases from baseline by > 0.3 mg/dL was 3, 0, and 4 (p = 0.14); by > 20% was 8, 2, and 7 (p = 0.32); and by > 30% was 5, 0, and 5 (p = 0.11).
Other: There was no significant overall treatment effect or differences between groups in the results of the RMANCOVA or non-parametric analyses for BCS and body weight (data not shown).
Discussion
The aim of this study was to compare the field efficacy and safety of the new combination tablet of benazepril and pimobendan (Fortekor Plus) to the reference products (Fortekor and Vetmedin) in order to support the registration of Fortekor Plus in Japan. The number of dogs recruited (67) was determined by a regulatory requirement of a minimum of 60 cases. The study achieved its objective by demonstrating non-inferior efficacy and good safety of Fortekor Plus compared to the reference products in dogs with CHF caused by MMVD.
It has been shown in bioequivalence studies that plasma concentrations of benazepril, pimobendan, and their metabolites do not exhibit biologically relevant differences after administration of Fortekor Plus tablets from those of Fortekor and Vetmedin in healthy beagle dogs (Elanco Animal Health; unpublished data). Regardless, field testing of Fortekor Plus was important for several reasons. First, bioequivalence studies may not detect all clinically relevant differences in efficacy or safety. Second, the weight bands in the dosing charts for Fortekor and Vetmedin differ, and the maximum daily dosage for pimobendan in Fortekor Plus (0.5 mg/kg) is slightly lower than for Vetmedin in Japan (0.7 mg/kg). In addition, for benazepril in Fortekor, the minimum starting dosage of 0.25 mg/kg SID can be doubled to 0.5 mg/kg SID. Since no doubling of the dosage of benazepril can be accommodated by using Fortekor Plus, as it is not permitted for pimobendan in Vetmedin, the upper end of the dosage range for benazepril,
i.e., 0.5 to 1.0 mg/kg/day, is recommended for Fortekor Plus. In this study, the dose regimens intended for Fortekor Plus were compared to those presently registered for Fortekor and Vetmedin in Japan. As a consequence, in the IVP group compared to the control groups, the daily mean dosage of benazepril was higher (respectively, 0.72
vs. 0.52 mg/kg) and the dosage of pimobendan slightly lower (0.36
vs. 0.48 mg/kg). It should be noted that the dosage ranges for pimobendan tested in this study (IVP, 0.26–0.5 mg/kg/day; control groups, 0.36–0.6 mg/kg/day) are lower than those that were tested in the QUEST and EPIC studies (0.4–0.6 mg/kg/day) [
511]. Third, benazepril is registered with SID dosing in Fortekor, but needs to be administered BID in Fortekor Plus in order to be compatible with pimobendan. Effects of BID and SID dosing of benazepril have been compared in healthy dogs by examining plasma or serum ACE activity, but those results do not predict all actions of ACEIs in clinical cases [
19]. Therefore, in this study, we compared SID and BID dosing of benazepril, in combination with pimobendan, via the use of two control groups. There were no significant differences in efficacy variables between groups and non-inferiority was demonstrated between the IVP and the control groups (both analyzed separately and combined) for the primary endpoint, indicating no clinically relevant differences in efficacy between the test articles and the dosage regimens.
Dogs in the IVP and both control groups showed significant improvement from baseline for the GCS and some secondary endpoints including NYHA class, and FETCH and pulmonary edema scores. This can be explained by the fact that all dogs were treated with an ACEI (benazepril) and pimobendan after D0, whereas prior to D0 only 79.1% of dogs received an ACEI and 49.3% received pimobendan, reflective of first opinion practice in Japan. Frequency of use and dosages of amlodipine, furosemide, spironolactone, and torasemide were similar prior to and after D0. The improvement
vs. baseline in all groups provides some evidence that benazepril and pimobendan in combination are effective in improving clinical signs in dogs with CHF caused by MMVD. To our knowledge, the combination of benazepril and pimobendan in dogs with CHF has not been tested previously in controlled prospective studies, although their combined use in a retrospective study has been reported [
9].
An important limitation of the study is that the primary and secondary efficacy endpoints relied on subjective assessments of the dog's clinical condition, made by an investigator after examining the dog and questioning the owner. We employed the same scoring schemes as were used previously in the QUEST and EPIC studies [
511]. Since there was no negative control group to provide internal validity, there is nevertheless a risk that the efficacy of all test articles was overestimated via the well-established “caregiver placebo effect” [
8]. In addition, the owners were not blinded to the test articles and there is a risk that they could have influenced the assessments made by the veterinarians. The pulmonary edema results are useful, therefore, since their assessment (of radiographs using a standard scheme) was more objective than the subjective scoring assessments. The pulmonary edema results support the conclusions of the other efficacy endpoints, with clinically relevant and significant improvement from baseline in all groups and non-inferior efficacy of the IVP compared to the Control I and Control I + II groups.
The safety of Fortekor Plus at its recommended dosing regimen was at least as good as that associated with the administration of Fortekor and Vetmedin. The frequency of all AEs was lower in the IVP group (50.0%) than in the control groups (78.6% and 63.2%), but the differences were not significant (p = 0.14). Most of the reported AEs were likely associated with the primary disease (CHF) or were incidental and not specifically related to the administration of IVP or control drugs. The frequency of emesis was lower in the IVP group (8.8%) than in the control groups (50.0% and 31.6%), and the magnitude of difference was clinically relevant and highly significant (p < 0.01). Reduced emesis could be the result of fewer tablets dosed and/or different excipients in Fortekor Plus compared to those in Fortekor and Vetmedin.
With the exception of plasma glucose, which could have indicated a type I error considering the multiple analyses, there were no significant differences between groups for any clinical chemistry or hematology variable. For plasma creatinine, the p values did not approach significance for overall treatment effect (p = 0.68) or comparisons between groups (p ≥ 0.52). These results suggest no marked differences between groups in the risk of acute kidney injury, which might have been of concern considering the higher dosage of benazepril in the IVP group. There is also the theoretical risk that a higher dosage of benazepril could lead to a higher frequency of hyperkalemia. There were, however, no significant differences between groups in plasma potassium concentrations, no cases in any group with marked increases in concentrations, and the mean values descended in the order Control I > Control II > IVP. Therefore, no special risks related to plasma creatinine or potassium were associated with Fortekor Plus treatment.
As noted previously, the daily dosage of benazepril is higher in Fortekor Plus compared to Fortekor, and it is administered BID. The results from the present study suggest no disadvantages for either efficacy or safety with the higher daily benazepril dosage of 0.72 mg/kg, administered in the IVP group, compared to the 0.50 or 0.54 mg/kg dosages used in the Control I or II groups. Toutain et al. [
19] predicted, from modeling, that administration of benazepril at half of the dosage BID should inhibit plasma ACE activity over 24 h at least as well as the full dosage SID, and this suggestion was confirmed recently by King et al. (unpublished paper) examining serum ACE. In the BENCH study, doubling of the dosage of benazepril from 0.25 to 0.5 mg/kg SID to 0.5 to 1.0 mg/kg SID did not increase the frequency of reported AEs [
34]. However, no conclusions on relative efficacy of different dosages of benazepril can be made from the BENCH study due to the study design.
In addition to those mentioned previously, the principal limitations of the present study are discussed below.
First, a study population size of 67 dogs is relatively low for a field study. The sample size was determined by the regulatory requirement for a minimum of 60 cases, and proved to be sufficient to test the primary objective of the study, i.e., demonstration of non-inferior efficacy for the primary endpoint with the defined δ of 20%. The limited number of dogs means that the study had low power to detect subtle differences in efficacy between the groups or to detect uncommon AEs; for example, the study had only 49% power to detect AEs with a true incidence of 1%.
Second, statistical analysis of the efficacy data was a challenge since ordinal scores were used and assessed repeatedly. To our knowledge, good non-parametric statistical methods for testing non-inferiority are not available. Therefore, the data were analyzed primarily by applying the parametric RMANCOVA method. Despite transforming data where appropriate, the distribution of all secondary endpoints deviated significantly from normality in the RMANCOVA analyses, and the distribution of the primary endpoint approached significance (
p = 0.088). However, ANOVA models are relatively robust even in the absence of normality [
12]; therefore, the results of the RMANCOVA analyses are judged to be reliable. Furthermore, the conclusion of lack of significant differences between groups for efficacy variables was confirmed by non-parametric analyses.
Third, we studied dogs at Japanese clinics with CHF in NYHA classes III and IV caused by MMVD. Diuretics were used in fewer cases (~30%) than is standard in many other countries, even though all dogs had evidence of pulmonary edema at baseline. The results, therefore, cannot be simply generalized to other settings.
Fourth, it was noted that furosemide was used prior to the study significantly more frequently in Control I and II groups than in the IVP group. Although this might have resulted from differences in disease severity at baseline, there was no detected effect on study conclusions as there was no significant association between previous use of diuretics and outcomes for any endpoint (
Table 6).
Fifth, limitations of non-inferiority studies have been well described, notably that the absence of significant differences between groups can be due to similar efficacy or similar lack of efficacy if there is no negative control to provide internal validity [
17]. However, the significant improvement from baseline in multiple variables, including the GCS and pulmonary edema scores, supports the conclusion that the IVP and both control groups had similar beneficial efficacy.
Finally, our study did not address in any way the possible advantages of using an ACEI with pimobendan over those of either drug alone. Further studies into the combination of benazepril and pimobendan are recommended.






 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download