Abstract
The development of veterinary dentistry has substantially improved the ability to diagnose canine and feline dental abnormalities. Consequently, examinations previously performed only on humans are now available for small animals, thus improving the diagnostic quality. This has increased the need for technical qualification of veterinary professionals and increased technological investments. This study evaluated the use of cone beam computed tomography and intraoral radiography as complementary exams for diagnosing dental abnormalities in dogs and cats. Cone beam computed tomography was provided faster image acquisition with high image quality, was associated with low ionizing radiation levels, enabled image editing, and reduced the exam duration. Our results showed that radiography was an effective method for dental radiographic examination with low cost and fast execution times, and can be performed during surgical procedures.
The development of veterinary dentistry has substantially improved diagnostic quality and efficiency, resulting in more satisfactory indexes for treatments performed on the stomatognathic system of domestic animals. In addition to demands for technological investment on the part of equipment manufacturing companies, this veterinary specialty requires technical qualification of medical personnel through training programs, continuing professional development, and the acquisition of state-of-the-art equipment. As a result of these advancements, dental procedures that were previously performed without the aid of diagnostic resources (especially imaging studies) are currently used in the daily routine of veterinary clinics and hospitals. This has significantly contributed to the success of interventions with this diagnostic modality.
Despite the increased diagnostic quality resulting from scientific discoveries, the high cost of dental exams is a limiting factor that can prevent the implementation of new technologies in the veterinary environment. Therefore, intraoral radiography (IOR) remains the chosen method for imagenologic examination for assessing abnormalities of the teeth and other oral cavity structures. If possible, this procedure should be performed during the animals' first dental appointment [22]. However, procedures such as tomography, which may seem economically impractical at first, might be routinely included in examination performed at veterinary clinics and hospitals if deemed necessary. Cone beam computed tomography (CBCT), routinely used in human medicine, has recently become a viable and cost-effective diagnostic alternative that can identify several different types of oral abnormalities in domestic animals [19].
Even though a previous report has shown that CBCT should only be recommended for diagnosing oral diseases in domestic animals [19], the first reports about the use of this technique in humans date back to the 1990s [5,10]. CBCT is a diagnostic modality in which the X-ray tube-detector system rotates 360° around the patient's head and acquires images that will be analyzed by a specific computer program [5,20]. Volumetric data obtained by tomography consist of three-dimensional blocks of small cuboid structures known as voxels. In CBCT, this block is isometric in that the height, width, and depth are equal [3].
Although CBCT has been included in the diagnostic routine for identifying dental diseases in human patients since the end of the last century, scientific reports have stated that standardization of the technique for animals is a very recent development in veterinary medicine. Nevertheless, it has become a reliable auxiliary method for diagnosing canine and feline odontostomatological abnormalities [19]. Due to the success of this technique, we recommend that it be used as an auxiliary exam for diagnosing infirmities such as feline dental resorptive lesions (FDRLs), temporomandibular joint abnormalities, facial trauma, and periodontal disease as well as planning dentistry implantation. Nevertheless, new research is required to validate the use of CBCT and to promote its use in the routine veterinary clinic practices. The purpose of this study was to evaluate the ability of CBCT and IOR to assess canine and feline dental abnormalities.
All protocols for this project were submitted for approval by the Animal Use Ethics Committee of the Institute of Biological Sciences of the University of Brasília, Brazil. Our study was carried out in accordance with ethical and animal welfare guidelines recommended by the Brazilian College of Animal Experimentation, Brazil. The project was approved and registered (No. UNBDOC 12339/2008).
Our study was carried out from June to September 2008. We included 25 male and female animals (19 dogs and 6 cats) that were treated at the dental health service of Centro Veterinário do Gama in Brasília, Brazil. All animals showed abnormalities that required imagenologic exams of the stomatognathic system for a conclusive diagnosis. CBCT and conventional IOR were selected as the auxiliary diagnostic methods (Table 1).
Each animal was examined by IOR and CBCT. Our analysis contrasted the image acquisition processes, image editing, and analyses. Both techniques were applied for diagnosing FDRLs or periodontal disease, and used for implant dentistry planning in dogs. Patients associated with evidence of dental abnormalities, albeit without signs of the diseases in question, were also included in the study to assist the diagnosis of other anomalies that affect the stomatognathic system.
CBCT was performed with a scanner (i-CAT; Xoran Technologies, Imaging Sciences International, USA) with the following specifications: 6 cm scan height, 40 sec scan time, 0.2 voxel (maximum resolution), 120 kV, and 46.72 mA/sec. During the exam, the animals were placed on a polyvinyl chloride tube with a diameter compatible with their thoracic perimeter. Afterwards, the animals were placed in an upright position so that the height of the tube matched their cervical and lumbar length. The animals were immobilized inside the tube by high density foam inserted between the body of the animal and tube wall [19]. Once the animals were positioned for tomography (Fig. 1), the device was activated. The captured images were transmitted to a microcomputer installed in an adjacent room from where it was possible to view the patients through lead glass. The images were analyzed by the computer programs of the scanner (3DVR and i-CAT vision; Imaging Sciences International, USA). The examination also enabled a 3D evaluation and implant simulation using specific software (Dental Slice; Bioparts, Brazil).
Intraoral X-rays were obtained with a dental X-ray machine (Spectro 70X; Dabi-Atlante, Brazil) and adult periapical and occusal radiographic film (Insight; Kodak, USA) for 0.05 to 0.1 sec. The film was placed according to parallel and bisecting techniques. The X-rays were processed in a dental darkroom with three receptacles containing developer (Kodak, USA), water, or fixer (Kodak, USA). The film was developed for 20 sec and fixed for 40 sec. After development, the film was washed and left to air dry [17,27].
The acquisition process and the volumetric tomographic images obtained were compared to those of the intraoral X-rays, regardless of the abnormality being evaluated. Specific elements were evaluated for the comparison including the time required for image processing, ease of patient positioning during the exam, possibility of image manipulation, structure identification, complementary factors related to the performance of the diagnostic procedures, and ionizing radiation. Comparison of the last parameter was based solely on data extracted from the literature. The animals were placed under general anesthesia during both exams according to a standard protocol [13].
Our study did not attempt to compare CBCT and IOR, but was conducted to describe the intraoral abnormalities that could be identified by these imaging methods. Thus, the results are presented as frequencies. For the statistical analysis, we used SPSS 11.0.4 (IBM SPSS, USA) for Mac OSX.
The average time required to obtain a CBCT image after patient positioning was 40 sec whereas an average of 0.06 sec was needed to obtain an IOR image. However, it took up to 20 min to correctly position the patients and film during the IOR examination, and the patients' recumbent position also needed to be changed during the exam. The CBCT examination did not require image processing, repeated scans, or the use of chemical substances. Images acquired by this technique were superior in quality and could be edited as a panoramic X-ray of the sagittal, frontal, and transverse sections. This permitted the creation of millimetrical sections, application of specific image enhancement filters, 3D image reconstruction, and analysis from all angles.
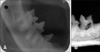
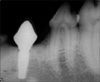
Conventional IOR enabled the analysis of a single dental element whereas CBCT facilitated the panoramic analysis of all dental elements in a single image. Head abnormalities such as trauma could also be viewed on the CBCT scans (Fig. 2). Fast and accurate CBCT image processing enabled surgical planning and correction of the abnormalities diagnosed; this process also provided faster, safer, and more effective patient diagnosis. Both CBCT and IOR enabled the accurate diagnosis of periodontal disease and FDRL in the six cats analyzed (Fig. 3). However, a single CBCT scan provided images of all dental elements, thus showing other teeth affected with abnormalities.
A full-mouth scan of a dog diagnosed with dental resorption was required. A single CBCT scan allowed us to determine an accurate diagnosis of the disease and of all dental elements involved. For the three dogs requiring dental implants, CBCT allowed assessment of the implant site via images taken of the transverse sections in oblique view (Fig. 4). On the other hand, IOR permitted evaluation of the bone structure in the surgical area, adequate implant height, and immediate post-operative assessment while the dogs were still under anesthesia (Fig. 5). In addition, CBCT provided accurate images of the entire bone structure for dental implant planning. These images allowed us to confirm measurements, simulate implant placement, and select implants with appropriate dimensions. This reduced the risk of bone trepanations or mandibular canal lesions.
Standard animal positioning under the scanner, which was established prior to this study, was crucial for evaluating feline and canine dental abnormalities in the present investigation. Similarly, the anesthesia protocol we used enabled safe and reliable image acquisition because the animals remained immobilized during the exam, which abolished the need for repeated scans. In addition to ensuring greater procedure effectiveness, the specifications used in the scanner for image acquisition reduced the occupational exposure of the medical professionals and animals to ionizing radiation; this has also been noted by other authors [2,18].
The average time taken to obtain a CBCT image after patient positioning was 40 sec. Although the average acquisition time for IOR was only 0.06 sec, patient and film positioning took up to 20 min, particularly when all dental elements required radiography. This technique also necessitated a change in the patient's recumbent position. The CBCT findings from our study concur with those of other studies [3,8] that evaluated this diagnostic procedure in humans. Faster image acquisition makes CBCT a safe procedure even for senile animals. On the other hand, longer duration of IOR procedures result in greater anesthesia consumption and increased risks for the patients.
Regarding criteria such as exam duration, use in senile animals, anesthesia consumption, radiation, and risks for the patient, CBCT is superior because it does not require image processing or an eventual exam repetition. This makes it a more reliable method. Furthermore, CBCT does not require the use of chemical substances, and produces images with superior quality that may be edited for visualization as a panoramic X-ray of the sagittal, frontal, and transverse sections. This technique also enables the creation of millimetric sections, application of specific image enhancement filters, 3D image reconstruction, and analysis from all view angles.
The non-use of chemical substances for CBCT image processing prevented the occupational exposure of medical professionals, which may be beneficial to the health of veterinary center workers. Although the absorbed radiation doses were not measured, other studies have shown that the radiation dose required for CBCT is significantly lower than that of conventional computed tomography [1,11,12,19,21] because the latter involves a series of rotations around the head (4, 8, 12, 16, 32, or 64-slice) for image acquisition [26]. Other studies have also shown that CBCT is associated with less emitted radiation than full-mouth periapical X-rays, and provides fast and accurate results [1,7].
For the assessment of teeth with three roots, CBCT enabled 3D reconstruction along with the evaluation of all roots and the tooth itself from all view angles and dimensions. IOR of the fourth premolar and upper first molar require special attention to positioning in order for the results to be reliable [15,16]. Besides accurately measuring the bisector of the angle between the tooth and film, the focus must be turned in a mesial-distal direction to acquire a clear image and avoid superposition of the mesial-buccal and mesial-palatine roots. In short, this type of radiography can be used to study the most significant differences in execution techniques between cats and dogs due to the position of the zygomatic arch in felines.
CBCT accurately diagnosed FDRLs, promoted visualization of all dental elements in a single acquisition, and did not require repeated scans. These factors are also associated with full-mouth periapical X-rays, the recommended technique for diagnosing FDRL [14,24,25]. The CBCT exam also enabled us to diagnose dental resorptions in one of the dogs, thus confirming a previous report involving a case of canine odontoclastic resorptive lesions [27]. By assessing the CBCT images produced for diagnosing of both of these diseases, we concluded that 3D reconstruction, tooth visualization from all angles, and minimum image distortion resulted in a more reliable diagnosis, advantages that have been previously attributed to CBCT [19].
In addition, CBCT was highly accurate in diagnosing head abnormalities such as trauma (even when compared to the extra-oral radiographs); hence it enabled joint assessment of the structures and dental elements involved. We were also able to surgically plan and correct the abnormalities diagnosed, thereby increasing treatment success. These results are in partial agreement with those of previous reports in humans [4] which recommended CBCT for diagnosing facial fractures and dental-alveolar injuries. However, such studies failed to point out the advantages of planning and procedure effectiveness associated with CBCT.
For dental implants, CBCT provided accurate images of the entire bone structure, thereby enabling us to confirm measurements and simulate implant placement. Such information helped us to select implants with dimensions suitable for the patients, thus reducing the risk of bone trepanations or mandibular canal lesions. In contrast, periapical X-rays failed to provide any data for these simulations. In human dentistry, some authors have identified CBCT as an effective method for this purpose and regard it as a reliable diagnosing method for guiding dental implantation procedures [6,9,23]. Therefore, by adding this technique to other diagnosing procedures, the use of CBCT in veterinary odontology services can serve as a viable option with an excellent cost-benefit relation. Given the effective application of CBCT for the diagnosis of animal bucco-dental abnormalities, this method seems to be perfectly viable for routine canine and feline dental examinations (especially in the specialized services).
In summary, our study showed that CBCT is an effective auxiliary method for diagnosing most canine and feline dental diseases. We verified the enhanced quality of the CBCT images after standardization, which allowed more accurate editing and analysis. Specific criteria must be kept in mind when selecting patients for CBCT. Alternatively, IOR can be rapidly executed, is cost-effective, and can be performed during surgical procedures. We believe that IOR remains the most suitable transoperative exam technique when assessing dental elements separately because this method may be performed during surgical procedures and it does not require additional anesthesia.
Figures and Tables
Fig. 1
Cat placed under cone beam computed tomography (CBCT) scanner via a polyvinyl chloride device.

Fig. 2
Cone beam CT of a cat's head after trauma. Panoramic view (bidimensional recontruction) showing mandibular (green arrows) and dental (yellow arrow) fractures.
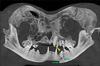
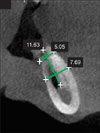
Fig. 4
Oblique view of a transverse CBCT section showing the mandibular area suitable for dental implantation. The software allowed measurement of the bone that helps determine the choice of implant.
References
1. Cohenca N, Simon JH, Roges R, Morag Y, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 1: traumatic injuries. Dent Traumatol. 2007. 23:95–104.

2. Costa MAF, Costa MFB, Roza MR, Gama Filho JB. Roza MR, editor. Biossegurança em odontologia veterinária. Odontologia em Pequenos Animais. 2004. Rio de Janeiro: LF Livros de Veterinária;19–38.
3. Farman AG, Scarfe WC. Development of imaging selection criteria and procedures should precede cephalometric assessment with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2006. 130:257–265.

4. Fullmer JM, Scarfe WC, Kushner GM, Albert B, Farman AG. Cone beam computed tomographic findings in refractory chronic suppurative osteomyelitis of the mandible. Br J Oral Maxillofac Surg. 2007. 45:364–371.

5. Garib DG, Raymundo R Jr, Raymundo MV, Raymundo DV, Ferreira SN. Tomografia computadorizada de feixe cônico (Cone Beam): Entendendo este novo método de diagnóstico por imagem com promissora aplicabilidade na ortodontia. Rev Dent Press Ortodon Ortop Facial. 2007. 12:139–156.

6. Guerrero ME, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D. State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Investig. 2006. 10:1–7.

7. Hatcher DC, Aboudara CL. Diagnosis goes digital. Am J Orthod Dentofacial Orthop. 2004. 125:512–515.

8. Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, Farman AG. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop. 2007. 132:429–438.

9. Iplikçioğlu H, Akça K, Çehreli MC. The use of computerized tomography for diagnosis and treatment planning in implant dentistry. J Oral Implantol. 2002. 28:29–36.

10. Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005. 32:282–293.
11. Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 96:508–513.

12. Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IAB. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998. 8:1558–1564.

13. Natalini CC. Teoria e Técnicas em Anestesiologia Veterinária. 2007. Porto Alegre: Artmed;83–88.
14. Negro VB, Hernández SZ, Saccomanno DM. Detección de lesiones odontoclásticas reabsortivas felinas (LORF) mediante examen clínico y radiológico. In Vet. 2005. 7:87–97.
15. Niemiec BA, Furman R. Canine dental radiography. J Vet Dent. 2004. 21:186–190.
16. Niemiec BA, Furman R. Feline dental radiography. J Vet Dent. 2004. 21:252–257.
17. Roza MR. Odontologia em Pequenos Animais. 2004. Rio de Janeiro: LF Livros de Veterinária;119–136.
18. Roza MR, Gama Filho JB, Costa MAF. Biossegurança em Ambientes Hospitalares Veterinários. 2003. Rio de Janeiro: Interciência;43–58.
19. Roza MR, Silva LAF, Januário AL, Barriviera M, Oliveira ACA, Fioravanti MCS. Tomografia computadorizada de feixe cônico na odontologia veterinária: descrição e padronização da técnica. Pesqui Vet Bras. 2009. 29:617–624.

20. Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006. 72:75–80.
21. Scarfe WC. Imaging of maxillofacial trauma: evolutions and emerging revolutions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:2 Suppl. S75–S96.

22. Tsugawa AJ, Verstraete FJM. How to Obtain and Interpret Periodontal Radiographs in Dogs. Clin Tech Small Anim Pract. 2000. 15:204–210.

23. Turkyilmaz I, Tözüm TF, Tumer C. Bone density assessments of oral implant sites using computerized tomography. J Oral Rehabil. 2007. 34:267–272.

24. van Wessum R, Harvey CE, Hennet P. Feline dental resorptive lesions. Prevalence patterns. Vet Clin North Am Small Anim Pract. 1992. 22:1405–1416.

25. Verstraete FJ, Kass PH, Terpak CH. Diagnostic value of full-mouth radiography in cats. Am J Vet Res. 1998. 59:692–695.
26. Winter AA, Pollack AS, Frommer HH, Koenig L. Cone Beam volumetric tomography vs. medical CT scanners: Expanding dental applications. NY State Dent J. 2005. 71:28–33.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download