Abstract
Purpose
Materials and Methods
Results
Conclusions
Figures and Tables
Table 1
Patient characteristics (n=1,899)

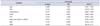
Table 2
Differences in men's general health score according to various parameters

Values are presented as mean±standard deviation or number (%).
PSA, prostate-specific antigen; TT, total testosterone; eGFR, estimated glomerular filtration rate; TPV, total prostate volume; MetS, metabolic syndrome; BMI, body mass index; WHR, waist-to-hip ratio; IPSS, International Prostate Symptom Score; CPSI, the National Institutes of Health Chronic Prostatitis Symptom Index; ADAM, androgen deficiency in aging males questionnaire; IIEF-5, International Index of Erectile Function-5; PEDT, premature ejaculation diagnostic tool.
Table 3
Logistic regression analyses predicting moderate to severe LUTS (IPSS≥8)

LUTS, lower urinary tract symptoms; IPSS, International Prostate Symptom Score; OR, odds ratio; CI, confidence interval; PSA, prostate-specific antigen; eGFR, estimated glomerular filtration rate; TPV, total prostate volume; MetS, metabolic syndrome; BMI, body mass index; WHR, waist-to-hip ratio.
a:Reference value.
Table 4
Logistic regression analyses predicting moderate to severe CP-like symptoms (CPSI≥15)
CP, chronic prostatitis; CPSI, National Institutes of Health Chronic Prostatitis Symptom Index; OR, odds ratio; CI, confidence interval; PSA, prostate-specific antigen; eGFR, estimated glomerular filtration rate; TPV, total prostate volume; MetS, metabolic syndrome; BMI, body mass index; WHR, waist-to-hip ratio.
a:Reference value.
Table 5
Logistic regression analyses predicting moderate to severe aging male's symptoms (ADAM≥37)

Table 6
Logistic regression analyses predicting moderate to severe erectile dysfunction (IIEF-5≤11)





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download