Abstract
Retrograde intrarenal surgery (RIRS) is being performed for the surgical management of upper urinary tract pathology. With the development of surgical instruments with improved deflection mechanisms, visuality, and durability, the role of RIRS has expanded to the treatment of urinary calculi located in the upper urinary tract, which compensates for the shortcomings of shock wave lithotripsy and percutaneous nephrolithotomy. RIRS can be considered a conservative treatment of upper urinary tract urothelial cancer (UTUC) or for postoperative surveillance after radical treatment of UTUC under an intensive surveillance program. RIRS has a steep learning curve and various surgical techniques can be used. The choice of instruments during RIRS should be based on increased surgical efficiency, decreased complications, and improved cost-benefit ratio.
Retrograde intrarenal surgery (RIRS) refers to the surgical management of upper urinary tract pathologies with a retrograde ureteroscopic approach. With the development of new surgical instruments, the deflection mechanism, visuality, and durability of RIRS have improved. Recently, the role of RIRS has expanded to the treatment of urinary calculi and urothelial malignancies in the upper urinary tract.
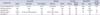
The first flexible ureteroscopic procedures were introduced in the 1960s [123]. However, these flexible ureteroscopes had no integrated deflecting systems or working channels. Flexible ureteroscopes were not widely utilized until the introduction of the new flexible ureteroscope and the holmium:yttrium aluminium garnet (YAG) laser system in the 1990s [45678]. Flexible ureteroscopes basically consist of the optical system of the fiberoptic image and light bundles, a deflection mechanism, and a working channel [9]. However, recently developed digital flexible ureteroscopes are expected to provide improved image quality and durability because they do not require a separate light cable or camera head [1011]. Narrow-band imaging digital flexible ureteroscopes are expected to increase the detection rate of upper urinary tract urothelial malignancy [12]. Deflecting mechanisms have been greatly developed as well. Deflection angles have recently been extended to 275 degrees, which enables ureteroscopic tips to access the entire renal collecting system, including the lower minor calices. Almost all flexible ureteroscopes currently available have working channels of at least 3.6 Fr in size, which permits adequate irrigation and insertion of stone retrieval devices. Dual-channel flexible ureteroscopes with smaller working channel diameters of 3.3 Fr have tried to overcome the limitation of a single channel to acquire better visual fields and surgical outcomes. However, the diameter of the outer sheaths was increased to 9.9 Fr [13]. With advances in the technical aspects of flexible ureteroscopes, laser lithotripsy systems, ureteral access sheaths, guidewires, highly flexible stone baskets, and flexible forceps, these instruments have become the requisites of RIRS. Table 1 lists the various flexible ureteroscopes that are currently widely used. Surgeons should know the advantages and disadvantages of the equipment to guarantee the best surgical outcomes.
Recently, the European Association of Urology guidelines for urolithiasis showed a broad spectrum of indicators for the active removal of kidney stones, such as stone growth, stones in patients at high risk of stone formation, obstruction caused by stones, infections, symptomatic stones with pain or hematuria, stones >15 mm, patient preference, comorbidity, and patients' social situation concerning profession or amount of travel [14]. In these cases, observation is not the option of choice. Rather, shock wave lithotripsy (SWL), percutaneous nephrolithotomy (PCNL), and RIRS are the available treatment options for active treatment of renal calculi [14].
Until now, SWL remained the first choice for the treatment of renal stones <20 mm in size [14]. However, many investigators have shown the disadvantages of SWL for treating renal stones. Previous investigations demonstrated inverse correlations between stone-free rates (SFRs) and stone sizes [15161718] and reported on the risk of ureteral obstruction with the need for additional procedures [15]. Unfavorable factors for success of SWL include SWL-resistant stones, steep infundibular-pelvic angles, a long lower pole calyx (>10 mm), and a narrow infundibulum (<5 mm) [1920212223]. Furthermore, SWL often requires multiple treatments and longer treatment periods than other surgical methods in patients with multiple stones. In these cases, surgeons should consider RIRS or PCNL to treat renal and upper ureter stones.
PCNL should be the first treatment choice for stones >20 mm [14]. RIRS cannot be recommended as the first treatment option for stones >20 mm. PCNL has generally been considered to be a safe surgical method with overall low postoperative complication rates and the highest SFR compared with other surgical methods [2425]. Although serious complications such as perioperative massive bleeding, urine leakage, bowel injury, hemothorax, and fistula are rare [26], increasing attention has been paid to the need for other minimally invasive surgical options to compensate for the shortcomings of PCNL.
Recently, technological advances in flexible ureteroscopy, coupled with the development of novel endoscopic baskets and flexible lithotrites, have allowed the role of RIRS to expand to the treatment of renal and upper tract calculi. Definite indications for RIRS have not yet been established. However, the possible indications for RIRS for renal stones are as follows:
· Midsized renal stones not appropriate for SWL or PCNL
· Failed SWL or SWL-resistant stones
· Radiolucent stones
· Anatomical abnormalities, e.g., steep infundibular-pelvic angle, long lower pole calyx, or narrow infundibulum
· Concomitant renal and ureter stones
· Complete removal of bilateral stones in a single session
· Multiple renal stones including nephrocalcinosis
· Bleeding disorders
· Need for complete stone removal, e.g., pilot
· Percutaneous antegrade approach for ureter stones in patients who underwent urinary diversion
· Combined or ancillary procedures following PCNL
· Patient habitus, e.g., obesity, unfit for anesthetic position
As mentioned above, SWL remains the first choice for renal stones <20 mm [14]. However, we should consider the inverse correlation between the SFR and stone size [15161718]. The European guidelines recommended a lower cutoff level of 15 mm [1427]. However, this is an arbitrary level and not a definite cutoff. The cutoff can be affected by many different factors, e.g., stone multiplicity, resistance to SWL, and patient need. The lower cutoff level for consideration of RIRS usually ranges from 10 to 15 mm. The upper cutoff level of stone size has been expanded to 30 to 35 mm in previous investigations [282930], which implies that RIRS can be a viable option for patients with renal stones >20 mm depending on the operator's skills.
Unfavorable factors for SWL include a steep infundibular-pelvic angle, a long lower pole calyx, or a narrow infundibulum in patients with a lower pole stone [1419202122]. PCNL is the first treatment option for lower pole stones along with a surgical procedure [333435]. However, RIRS has shown comparable surgical efficacy and safety as well in these investigations.
Because RIRS does not require a percutaneous procedure and has little probability of vessel injury during the surgical procedure, RIRS seems to be superior to PCNL or SWL for patients who take anticoagulant therapy. Until now, the ureteroscopic procedure including RIRS has shown its safety in patients with bleeding disorders with an acceptable level of increase in complications [363738].
The presence of a bleeding disorder is one of the contraindications to SWL and patients who are scheduled to undergo PCNL are usually recommended to discontinue anticoagulant therapy. However, some studies showed that continuing aspirin therapy is safe during PCNL [3940]. Further studies are needed to prove the safety of PCNL in patients with bleeding disorders.
When patients with ureteral strictures, urinary diversion of ileal conduits, or orthotopic neobladders have ureter stones, a retrograde approach is sometimes difficult. In these cases, a percutaneous antegrade approach using a flexible ureteroscope would be appropriate [4142]. The percutaneous procedure has proven efficacy and safety with a high SFR and minor complications [4142]. Furthermore, if migration of fragmented small stones into the ureter occurs during PCNL, a flexible ureteroscope would be helpful to remove the stones by use of laser lithotripsy or a stone basket. The percutaneous approach can be available by use of a ureteral access sheath or a small-sized balloon catheter.
More importantly, RIRS can be performed in all patients without any specific contraindications as shown in the European guidelines [14]. The first step is that each treatment should be considered with regard to the clinical situation, and clinicians should determine whether RIRS is the most appropriate surgical option.
Endoscopic surgery began with the treatment of upper urinary tract urothelial cancer (UTUC) in the 1980s [434445]. Currently, RIRS can be considered a conservative treatment of UTUC or for postoperative surveillance after radical treatment of UTUC [4647]. The smooth muscle of the ureter and the renal pelvis is thinner than the bladder wall, which implies that UTUC can penetrate the wall earlier than the bladder tumor [48]. Ureteroscopic treatment of UTUC is usually based on ablation and resection using holmium:YAG lasers [47]. However, undergrading and understaging of UTUC lesions can have severe consequences. In one study, up to 25% of patients had missed UTIC lesions, and nearly 50% had a missed carcinoma in situ lesion [49]. Therefore, endoscopic management should only be considered for patients with low-grade, low-stage UTUC under an intensive surveillance program. Recently, narrow-band imaging digital flexible ureteroscopy has been developed and is expected to increase the detection rate of UTUC [12]. Narrow-band imaging is a new diagnostic approach to visualize angiogenesis in the superficial malignancy. However, further studies of this diagnostic technique are needed.
To predict surgical success following RIRS, two wellvalidated tools have been introduced [5051]. Resorlu et al. [50] investigated the prognostic factors associated with RIRS and developed a scoring system called the Resorlu-Unsal Stone Score to predict the SFR. They reviewed 207 patients who underwent RIRS and showed that stone size, stone composition, stone number, renal malformations, and lower pole infundibulopelvic angle are significant predictors of RIRS outcome. The authors invented the scoring system based on the significant predictors. Similarly, Jung et al. [51] developed another scoring system for RIRS called the Modified S-ReSC or S-ReSC-R [52]. This scoring system is based on the number of sites of renal stones involved. The anatomical sites were classified into 9 subgroups, such as the renal pelvis (#1), superior and inferior major calyceal groups (#2-3), and anterior and posterior minor calyceal groups of the superior (#4-5), middle (#6-7), and inferior calyx (#8-9). If the stone is located in the inferior caliceal area (#3, #8-9), one additional point per site is added to the original score. The advantage of this scoring system is that it was externally validated for the first time [52] and its predictive accuracy was shown to be better than that of the Resorlu-Unsal Stone Score. Both scoring systems have been helpful for separating patients into outcome groups and for determining plans of treatment.
Previous studies showed that the SFR of RIRS ranges from 73.6% to 94.1% [53]. Compared with the SFR of PCNL, the SFR of RIRS was lower (odds ratio [OR], 2.19; 95% confidence interval [CI], 1.53-3.13; p<0.00001). The operative time of RIRS ranged from 43.1 to 67.5 minutes, which was longer than that of PCNL (OR, -4.81, 95% CI: -14.05 to 4.43, p=0.03). Complication rates ranged from 0% to 25%, which was lower than for PCNL (OR, 1.61; 95% CI, 1.11-2.35; p<0.01). Hospital stay was shorter for RIRS than for PCNL (OR, 1.28; 95% CI, 0.79-1.77; p<0.00001). Common complications of RIRS were fever (2%-28%), prolonged antibiotic use (4%-5%), and sepsis (3%-5%) and less common complications were bleeding (<5%), steinstrasse, and ureteral injuries.
Previous investigations addressed whether stone treatment results in renal functional change [5455]. Data on renal morphology and function are usually based on radiological examinations, combined with blood tests and urinalysis. Although Giusti et al. [55] showed that RIRS is safe in the treatment of renal stones without worsening renal function, these data did not provide information on separate renal function. Separate renal function can be estimated by diethylenetriamine pentaacetic acid (99mTc-DTPA) or technetium-99m dimercaptosuccinic acid (99mTc-DMSA). Recently, the author of the present review reported perioperative data for separate renal function [56]. In that study, separate renal function was deteriorated in one-third of patients (53 of 148, 35.8%) with renal stones >10 mm who underwent RIRS or miniaturized PCNL. The abnormal separate renal function showed postoperative recovery in 31 patients (58.5%). The study included 148 patients (117 RIRS and 31 miniaturized PCNL) and there were no statistically significant differences between the two patient groups in the deterioration of separate renal function or in postoperative recovery.
A variety of surgical techniques can be utilized to perform RIRS. Many investigators understand that RIRS has a steep learning curve if they do not have an assistant to help. There has been a single investigation to show the learning curve of RIRS [28]. Cho et al. [28] retrospectively investigated 100 patients who underwent single-session RIRS to treat mid-sized stones and analyzed the learning curve by using CUSUM (cumulative sum) analysis for monitoring change in fragmentation efficacy. The CUSUM curve showed that the 56th case was the change point at which a plateau was reached. The acceptable level of fragmentation efficacy was 25 mL/min. Stone multiplicity and sites involved were significant predictors of the SFR for RIRS.
Surgical technique will continue to change in the future with new developments in instruments. Essentially, the use of various instruments should be based on increased surgical efficiency, decreased complications, and improved cost-benefit ratio. The commonly used equipment and devices for RIRS are as follows:
· Flexible and (semi) rigid ureteroscopes
· Fluoroscopy (C-arm) with radiation protectors
· Guidewires
· 5-Fr ureteral catheter or dual-lumen catheter
· Contrast medium and balloon catheter if needed
· Ureteral access sheath (10/12, 12/14, 14/16 Fr, 28/35/45/55 cm)
· Holmium:YAG laser with laser fiber (200/365 µm)
· Stone basket (<2 Fr)
· Irrigation pump
The patient is positioned in a dorsal lithotomy position. The first step is securing access to the ureter. Either cystoscopic or ureteroscopic access to the ureter is appropriate. A hydrophilic guidewire is placed in the renal pelvis under fluoroscopy. This catheter is often changed into a stiff guidewire using an open-ended 5-Fr ureteral catheter. The ureteral lumen or ureterovesical junction can be dilated by use of a balloon dilatation catheter or by ureteroscopy.
When there is a narrowing or stricture in the ureter, a ureteral double J (DJ) stent can be inserted preoperatively. The stent is then retracted several weeks later and a stiff guidewire is inserted into the DJ stent. Previous investigations showed that preoperative ureteral stenting was associated with a high SFR and decreased operative time and cost for larger stones [575859]. However, this topic is still controversial, because patients may undergo an additional preoperative stenting procedure and may suffer from a longer duration of discomfort related to preoperative DJ stenting [60].
After ureteral cannulation, a ureteral access sheath is usually placed on the guidewire to the level of the ureteropelvic junction. There have been no absolute indications for the use of ureteral access sheaths. Ureteral access sheaths allow repeated ureteroscopic access to the renal pelvis and facilitate removal of multiple stone fragments. Although it is controversial whether the placement of ureteral access sheaths helps to increase the SFR [6162], the sheaths seem to be helpful for maintaining a continuous flow of irrigation fluid and an intra-renal low-pressure system [6364]. Ureteral access sheaths may induce ureter injury in certain situations [65]. However, there is little evidence for whether preoperative stenting reduces ureter injury [5759]. Ureteral access sheaths would not be necessary when a single passage of a stone is necessary after most of the stones are fully fragmented. However, bladder distention may induce narrowing of the ureterovesical junction, which may disturb drainage of irrigation fluid and a clear field of vision.
Several companies have developed a variety of new ureteral access sheaths [66]. The sizes of the most commonly used ureteral access sheaths range from 10/12 to 14/16 Fr in diameter and from 28 to 55 cm in length. Larger ureteral access sheaths are expected to be more beneficial for continuous irrigation of fluid but may be more hazardous to the ureter than smaller sheaths. However, little evidence has yet been reported [6367].
Almost all fiberoptic and digital ureteroscopes can fit through a 12/14 ureteral access sheath. The new standard 10/12 Fr sheaths and the minimization of flexible ureteroscope size will influence surgical trends in RIRS in the future.
A flexible ureteroscope is then inserted through the access sheath or on a guidewire. The holmium:YAG laser has become the gold standard lithotrite for RIRS [14]. The holmium laser consists of optical elements of fiber and plastic coating and has dual actions of producing stone dust or fragments mainly by the photothermal reaction [6869]. Acoustic shock waves by cavitation bubbles are less important. However, bubbles would improve photonic energy transmission into a renal stone. The fragmented stones can be removed by a stone basket and stone dust is small enough to pass through the urine. The author of the present review has performed about 500 cases of RIRS and favors the fragmentation technique over dust formation, especially for patients with large stones >10 mm, because the dust may hinder visualization of the clear operative field and it may be difficult to differentiate a small fragmented stone in the midst of dust. Stones from other calices can be repositioned into a single upper or middle calyx to increase the surgical efficiency and the durability of flexible ureteroscopy during the dust technique. The holmium laser power is usually set to 10 to 15 W with 0.5-1.2 J and 5-15 Hz. However, the setting may differ according to the method of lithotripsy [70] and surgeons usually increase the frequency (Hz) and maintain the power (W) when they perform the dust technique to increase the chance of laser lithotripsy.
Laser fibers sized 200 or 365 µm are usually used for treatment of stones. Small fibers (200-270 µm) are expected to be superior to larger ones (365 µm) because of similar fragmentation efficacy, increased efficiency of fluid irrigation, and increased flexibility [71]. However, the power (W) and energy (J) are important to maintain the fragmentation efficacy, and 365-µm laser fibers are more widely used than 200-µm fibers [72]. In flexible ureteroscopy, 200-µm laser fibers should be used to break lower pole stones.
Although the working channels of flexible ureteroscopy are >3 Fr, stone retrieval baskets <2 Fr are usually used to acquire maximal deflection of flexible ureteroscopy and constant irrigation of fluid [73]. The tipless design of stone retrieval baskets permits the capture of small stones even at the base of the renal pelvis and calices.
The combination of RIRS with other techniques is promising [747576]. Endoscopic combined intrarenal surgery using flexible ureteroscopy and miniature PCNL (endoscopic combined intrarenal surgery) or extracorporeal lithotripsy (lithotripsy endoscopically controlled by ureterorenoscopy) increase positive surgical outcomes, especially in complex renal stone cases. However, previous investigations have not yet shown increased SFRs [747576]. This approach would decrease the necessity of multiple percutaneous tracts, which would be helpful to decrease bleeding risk and radiation exposure. Furthermore, combined procedures deserve consideration for removal of stones associated with infundibular stenosis and caliceal diverticulum [77].
Some investigators have reported a newly developed robotic RIRS system [7879]. It is not clear whether this technique improves surgical outcomes or not. The potential advantages of robotic RIRS are improved ergonomics and instrument stability. An early clinical result showed data for 81 patients with renal calculi with a mean stone volume of 1,296 mm3 and a safe platform with significant improvement of ergonomics [79].
RIRS is an effective and safe treatment method for active removal of renal stones and detection of urothelial malignancy. RIRS will continue to evolve through technical improvements to the instrumentation. Urologists must make the best choice for their patients depending on surgical efficiency with this developing armamentarium, considering safety during the surgical procedure, the cost-benefit ratio, their area of expertise, and various patient characteristics.
Figures and Tables
Table 1
Characteristics of the widely used flexible ureteroscopes
ACKNOWLEDGMENTS
This work was supported by a clinical research grant-in-aid from the Seoul Metropolitan Government Seoul National University (SMG-SNU) Boramae Medical Center (16-2015-31).
References
1. Marshall VF. Fiber optics in urology. J Urol. 1964; 91:110–114.
2. Takagi T, Go T, Takayasu H, Aso Y. Fiberoptic pyeloureteroscope. Surgery. 1971; 70:661–663.
3. Bush IM, Goldberg E, Javadpour N, Chakrobortty H, Morelli F. Ureteroscopy and renoscopy: a preliminary report. Chic Med Sch Q. 1970; 30:46–49.
4. Abdel-Razzak OM, Bagley DH. Clinical experience with flexible ureteropyeloscopy. J Urol. 1992; 148:1788–1792.
5. Bagley DH. Intrarenal access with the flexible ureteropyeloscope: effects of active and passive tip deflection. J Endourol. 1993; 7:221–224.
6. Johnson DE, Cromeens DM, Price RE. Use of the holmium:YAG laser in urology. Lasers Surg Med. 1992; 12:353–363.
7. Albert P. The holmium:YAG laser: applications in urology. Clin Laser Mon. 1993; 11:39–41.
8. Bagley D, Erhard M. Use of the holmium laser in the upper urinary tract. Tech Urol. 1995; 1:25–30.
9. Conlin MJ, Marberger M, Bagley DH. Ureteroscopy: development and instrumentation. Urol Clin North Am. 1997; 24:25–42.
10. Shah K, Monga M, Knudsen B. Prospective randomized trial comparing 2 flexible digital ureteroscopes: ACMI/Olympus invisio DUR-D and Olympus URF-V. Urology. 2015; 85:1267–1271.
11. Multescu R, Geavlete B, Georgescu D, Geavlete P. Improved durability of flex-Xc digital flexible ureteroscope: how long can you expect it to last? Urology. 2014; 84:32–35.
12. Traxer O, Geavlete B, de Medina SG, Sibony M, Al-Qahtani SM. Narrow-band imaging digital flexible ureteroscopy in detection of upper urinary tract transitional-cell carcinoma: initial experience. J Endourol. 2011; 25:19–23.
13. Haberman K, Ortiz-Alvarado O, Chotikawanich E, Monga M. A dual-channel flexible ureteroscope: evaluation of deflection, flow, illumination, and optics. J Endourol. 2011; 25:1411–1414.
14. Türk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Guidelines on urolithiasis [Internet]. Anheim (NL): European Association of Urology;c2014. cited 2015 Jan 5. Available from: http://uroweb.org/wp-content/uploads/22-Urolithiasis_LR.pdf.
15. Argyropoulos AN, Tolley DA. Evaluation of outcome following lithotripsy. Curr Opin Urol. 2010; 20:154–158.
16. Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. 2009; (4):CD007044.
17. Sahinkanat T, Ekerbicer H, Onal B, Tansu N, Resim S, Citgez S, et al. Evaluation of the effects of relationships between main spatial lower pole calyceal anatomic factors on the success of shock-wave lithotripsy in patients with lower pole kidney stones. Urology. 2008; 71:801–805.
18. Danuser H, Muller R, Descoeudres B, Dobry E, Studer UE. Extracorporeal shock wave lithotripsy of lower calyx calculi: how much is treatment outcome influenced by the anatomy of the collecting system? Eur Urol. 2007; 52:539–546.
19. Pearle MS, Lingeman JE, Leveillee R, Kuo R, Preminger GM, Nadler RB, et al. Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol. 2005; 173:2005–2009.
20. Albanis S, Ather HM, Papatsoris AG, Masood J, Staios D, Sheikh T, et al. Inversion, hydration and diuresis during extracorporeal shock wave lithotripsy: does it improve the stone-free rate for lower pole stone clearance? Urol Int. 2009; 83:211–216.
21. Kosar A, Ozturk A, Serel TA, Akkus S, Unal OS. Effect of vibration massage therapy after extracorporeal shockwave lithotripsy in patients with lower caliceal stones. J Endourol. 1999; 13:705–707.
22. Aboumarzouk OM, Monga M, Kata SG, Traxer O, Somani BK. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol. 2012; 26:1257–1263.
23. Handa RK, Bailey MR, Paun M, Gao S, Connors BA, Willis LR, et al. Pretreatment with low-energy shock waves induces renal vasoconstriction during standard shock wave lithotripsy (SWL): a treatment protocol known to reduce SWL-induced renal injury. BJU Int. 2009; 103:1270–1274.
24. Olvera-Posada D, Tailly T, Alenezi H, Violette PD, Nott L, Denstedt JD, et al. Risk Factors for Postoperative Complications of Percutaneous Nephrolithotomy at a Tertiary Referral Center. J Urol. 2015; 07. 02. [Epub]. DOI: 10.1016/j.juro.2015.06.095.
25. Kyriazis I, Panagopoulos V, Kallidonis P, Ozsoy M, Vasilas M, Liatsikos E. Complications in percutaneous nephrolithotomy. World J Urol. 2015; 33:1069–1077.
26. Chubak B, Stern JM. An unusual presentation of colon perforation following percutaneous nephrolithotomy. Can Urol Assoc J. 2014; 8:E862–E866.
27. Keeley FX Jr, Tilling K, Elves A, Menezes P, Wills M, Rao N, et al. Preliminary results of a randomized controlled trial of prophylactic shock wave lithotripsy for small asymptomatic renal calyceal stones. BJU Int. 2001; 87:1–8.
28. Cho SY, Choo MS, Jung JH, Jeong CW, Oh S, Lee SB, et al. Cumulative sum analysis for experiences of a single-session retrograde intrarenal stone surgery and analysis of predictors for stone-free status. PLoS One. 2014; 9:e84878.
29. Jung GH, Jung JH, Ahn TS, Lee JS, Cho SY, Jeong CW, et al. Comparison of retrograde intrarenal surgery versus a single-session percutaneous nephrolithotomy for lower-pole stones with a diameter of 15 to 30 mm: A propensity score-matching study. Korean J Urol. 2015; 56:525–532.
30. Wilhelm K, Hein S, Adams F, Schlager D, Miernik A, Schoenthaler M. Ultra-mini PCNL versus flexible ureteroscopy: a matched analysis of analgesic consumption and treatment-related patient satisfaction in patients with renal stones 10-35 mm. World J Urol. 2015; 05. 14. DOI: 10.1007/s00345-015-1585-5. [Epub].
31. Alkan E, Avci E, Ozkanli AO, Acar O, Balbay MD. Same-session bilateral retrograde intrarenal surgery for upper urinary system stones: safety and efficacy. J Endourol. 2014; 28:757–762.
32. Goldberg H, Holland R, Tal R, Lask DM, Livne PM, Lifshitz DA. The impact of retrograde intrarenal surgery for asymptomatic renal stones in patients undergoing ureteroscopy for a symptomatic ureteral stone. J Endourol. 2013; 27:970–973.
33. Zhang W, Zhou T, Wu T, Gao X, Peng Y, Xu C, et al. Retrograde intrarenal surgery versus percutaneous nephrolithotomy versus extracorporeal shockwave lithotripsy for treatment of lower pole renal stones: a meta-analysis and systematic review. J Endourol. 2015; 29:745–759.
34. Ozturk U, Sener NC, Goktug HN, Nalbant I, Gucuk A, Imamoglu MA. Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10-20 mm. Urol Int. 2013; 91:345–349.
35. Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. 2011; 25:1131–1135.
36. Turna B, Stein RJ, Smaldone MC, Santos BR, Kefer JC, Jackman SV, et al. Safety and efficacy of flexible ureterorenoscopy and holmium:YAG lithotripsy for intrarenal stones in anticoagulated cases. J Urol. 2008; 179:1415–1419.
37. Watterson JD, Girvan AR, Cook AJ, Beiko DT, Nott L, Auge BK, et al. Safety and efficacy of holmium: YAG laser lithotripsy in patients with bleeding diatheses. J Urol. 2002; 168:442–445.
38. Aboumarzouk OM, Somani BK, Monga M. Flexible ureteroscopy and holmium:YAG laser lithotripsy for stone disease in patients with bleeding diathesis: a systematic review of the literature. Int Braz J Urol. 2012; 38:298–305.
39. Leavitt DA, Theckumparampil N, Moreira DM, Elsamra SE, Morganstern B, Hoenig DM, et al. Percutaneous nephrolithotomy during uninterrupted aspirin therapy in high-cardiovascular risk patients: preliminary report. Urology. 2014; 84:1034–1038.
40. Leavitt DA, Theckumparampil N, Moreira DM, Elsamra SE, Waingankar N, Hoenig DM, et al. Continuing aspirin therapy during percutaneous nephrolithotomy: unsafe or under-utilized? J Endourol. 2014; 28:1399–1403.
41. Zhong W, Yang B, He F, Wang L, Swami S, Zeng G. Surgical management of urolithiasis in patients after urinary diversion. PLoS One. 2014; 9:e111371.
42. Stuurman RE, Al-Qahtani SM, Cornu JN, Traxer O. Antegrade percutaneous flexible endoscopic approach for the management of urinary diversion-associated complications. J Endourol. 2013; 27:1330–1334.
43. Tasca A, Zattoni F. The case for a percutaneous approach to transitional cell carcinoma of the renal pelvis. J Urol. 1990; 143:902–904.
44. Woodhouse CR, Kellett MJ, Bloom HJ. Percutaneous renal surgery and local radiotherapy in the management of renal pelvic transitional cell carcinoma. Br J Urol. 1986; 58:245–249.
45. Orihuela E, Smith AD. Percutaneous treatment of transitional cell carcinoma of the upper urinary tract. Urol Clin North Am. 1988; 15:425–431.
46. Cornu JN, Roupret M, Carpentier X, Geavlete B, de Medina SG, Cussenot O, et al. Oncologic control obtained after exclusive flexible ureteroscopic management of upper urinary tract urothelial cell carcinoma. World J Urol. 2010; 28:151–156.
47. Bagley DH, Grasso M 3rd. Ureteroscopic laser treatment of upper urinary tract neoplasms. World J Urol. 2010; 28:143–149.
48. Stewart GD, Bariol SV, Grigor KM, Tolley DA, McNeill SA. A comparison of the pathology of transitional cell carcinoma of the bladder and upper urinary tract. BJU Int. 2005; 95:791–793.
49. Yamany T, van Batavia J, Ahn J, Shapiro E, Gupta M. Ureterorenoscopy for upper tract urothelial carcinoma: how often are we missing lesions? Urology. 2015; 85:311–315.
50. Resorlu B, Unsal A, Gulec H, Oztuna D. A new scoring system for predicting stone-free rate after retrograde intrarenal surgery: the "resorlu-unsal stone score". Urology. 2012; 80:512–518.
51. Jung JW, Lee BK, Park YH, Lee S, Jeong SJ, Lee SE, et al. Modified Seoul National University Renal Stone Complexity score for retrograde intrarenal surgery. Urolithiasis. 2014; 42:335–340.
52. Park J, Kang M, Jeong CW, Oh S, Lee JW, Lee SB, et al. External validation and evaluation of reliability and validity of the modified seoul national university renal stone complexity scoring system to predict stone-free status after retrograde intrarenal surgery. J Endourol. 2015; 29:888–893.
53. De S, Autorino R, Kim FJ, Zargar H, Laydner H, Balsamo R, et al. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol. 2015; 67:125–137.
54. Chou YH, Li CC, Hsu H, Chang WC, Liu CC, Li WM, et al. Renal function in patients with urinary stones of varying compositions. Kaohsiung J Med Sci. 2011; 27:264–267.
55. Giusti G, Proietti S, Cindolo L, Peschechera R, Sortino G, Berardinelli F, et al. Is retrograde intrarenal surgery a viable treatment option for renal stones in patients with solitary kidney? World J Urol. 2015; 33:309–314.
56. Piao S, Park J, Son H, Jeong H, Cho SY. Evaluation of renal function in patients with a main renal stone larger than 1 cm and perioperative renal functional change in minimally invasive renal stone surgery: a prospective, observational study. World J Urol. 2015; 07. 31. DOI: 10.1007/s00345-015-1653-x. [Epub].
57. Netsch C, Knipper S, Bach T, Herrmann TR, Gross AJ. Impact of preoperative ureteral stenting on stone-free rates of ureteroscopy for nephroureterolithiasis: a matched-paired analysis of 286 patients. Urology. 2012; 80:1214–1219.
58. Chu L, Farris CA, Corcoran AT, Averch TD. Preoperative stent placement decreases cost of ureteroscopy. Urology. 2011; 78:309–313.
59. Chu L, Sternberg KM, Averch TD. Preoperative stenting decreases operative time and reoperative rates of ureteroscopy. J Endourol. 2011; 25:751–754.
60. Lange D, Bidnur S, Hoag N, Chew BH. Ureteral stent-associated complications--where we are and where we are going. Nat Rev Urol. 2015; 12:17–25.
61. Traxer O, Wendt-Nordahl G, Sodha H, Rassweiler J, Meretyk S, Tefekli A, et al. Differences in renal stone treatment and outcomes for patients treated either with or without the support of a ureteral access sheath: The Clinical Research Office of the Endourological Society Ureteroscopy Global Study. World J Urol. 2015; 05. 14. [Epub]. DOI: 10.1007/s00345-015-1582-8.
62. Berquet G, Prunel P, Verhoest G, Mathieu R, Bensalah K. The use of a ureteral access sheath does not improve stone-free rate after ureteroscopy for upper urinary tract stones. World J Urol. 2014; 32:229–232.
63. Ng YH, Somani BK, Dennison A, Kata SG, Nabi G, Brown S. Irrigant flow and intrarenal pressure during flexible ureteroscopy: the effect of different access sheaths, working channel instruments, and hydrostatic pressure. J Endourol. 2010; 24:1915–1920.
64. Auge BK, Pietrow PK, Lallas CD, Raj GV, Santa-Cruz RW, Preminger GM. Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol. 2004; 18:33–36.
65. Traxer O, Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol. 2013; 189:580–584.
66. Sarkissian C, Noble M, Li J, Monga M. Patient decision making for asymptomatic renal calculi: balancing benefit and risk. Urology. 2013; 81:236–240.
67. Mogilevkin Y, Sofer M, Margel D, Greenstein A, Lifshitz D. Predicting an effective ureteral access sheath insertion: a bicenter prospective study. J Endourol. 2014; 28:1414–1417.
68. Vassar GJ, Chan KF, Teichman JM, Glickman RD, Weintraub ST, Pfefer TJ, et al. Holmium: YAG lithotripsy: photothermal mechanism. J Endourol. 1999; 13:181–190.
69. Chan KF, Vassar GJ, Pfefer TJ, Teichman JM, Glickman RD, Weintraub ST, et al. Holmium:YAG laser lithotripsy: a dominant photothermal ablative mechanism with chemical decomposition of urinary calculi. Lasers Surg Med. 1999; 25:22–37.
70. Prabhakar M. Retrograde ureteroscopic intrarenal surgery for large (1.6-3.5 cm) upper ureteric/renal calculus. Indian J Urol. 2010; 26:46–49.
71. Kuo RL, Aslan P, Zhong P, Preminger GM. Impact of holmium laser settings and fiber diameter on stone fragmentation and endoscope deflection. J Endourol. 1998; 12:523–527.
72. Knudsen BE, Pedro R, Hinck B, Monga M. Durability of reusable holmium:YAG laser fibers: a multicenter study. J Urol. 2011; 185:160–163.
73. Korman E, Hendlin K, Monga M. Small-diameter nitinol stone baskets: radial dilation force and dynamics of opening. J Endourol. 2011; 25:1537–1540.
74. Hamamoto S, Yasui T, Okada A, Koiwa S, Taguchi K, Itoh Y, et al. Efficacy of endoscopic combined intrarenal surgery in the prone split-leg position for staghorn calculi. J Endourol. 2015; 29:19–24.
75. Cracco CM, Scoffone CM. ECIRS (Endoscopic Combined Intrarenal Surgery) in the Galdakao-modified supine Valdivia position: a new life for percutaneous surgery? World J Urol. 2011; 29:821–827.
76. Traxer O, Letendre J. Extracorporeal lithotripsy endoscopically controlled by ureterorenoscopy (LECURS): a new concept for the treatment of kidney stones-first clinical experience using digital ureterorenoscopes. World J Urol. 2014; 32:715–721.
77. Palmero JL, Miralles J, Garau C, Nuno de, Amoros A, Benedicto A. Retrograde intrarenal surgery (RIRS) in the treatment of calyceal diverticulum with lithiasis. Arch Esp Urol. 2014; 67:331–336.
78. Desai MM, Aron M, Gill IS, Pascal-Haber G, Ukimura O, Kaouk JH, et al. Flexible robotic retrograde renoscopy: description of novel robotic device and preliminary laboratory experience. Urology. 2008; 72:42–46.
79. Saglam R, Muslumanoglu AY, Tokatlı Z, Caskurlu T, Sarica K, Tasci Aİ, et al. A new robot for flexible ureteroscopy: development and early clinical results (IDEAL stage 1-2b). Eur Urol. 2014; 66:1092–1100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download