Abstract
Purpose
To document the experiences of a single institution in evaluating the clinical courses and treatment outcomes of patients with cystine stones.
Materials and Methods
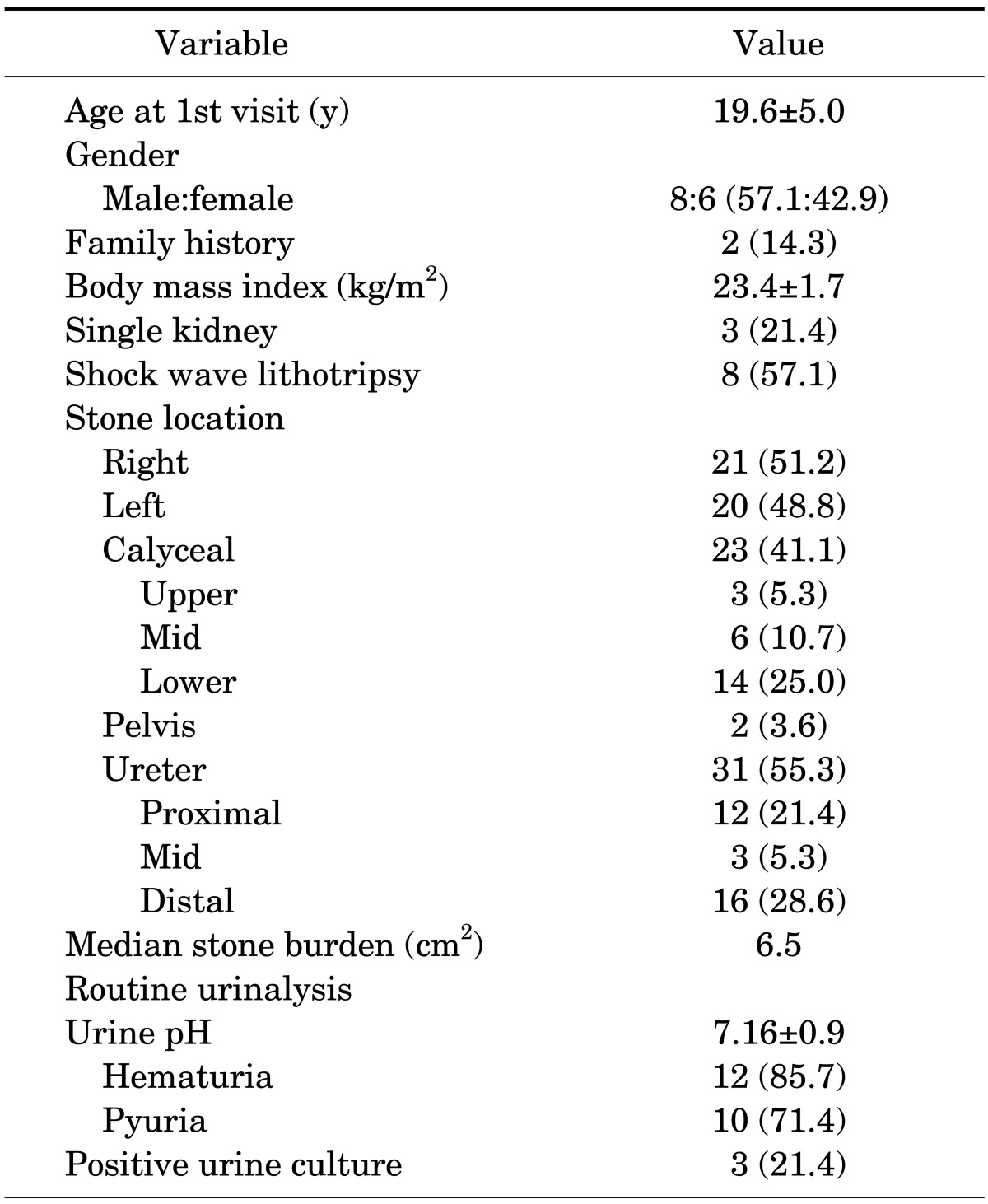
The clinical data of 14 patients with cystine stones who were treated at our institution from March 1994 to July 2012 were reviewed. These data included age at first visit, gender, family history, body mass index, presence of a single kidney, stone locations, stone burden, routine urinalysis, and culture. In addition, we also analyzed data on surgery, shock wave lithotripsy, medical treatment, stone recurrence or regrowth, and overall treatment success rates.
Results
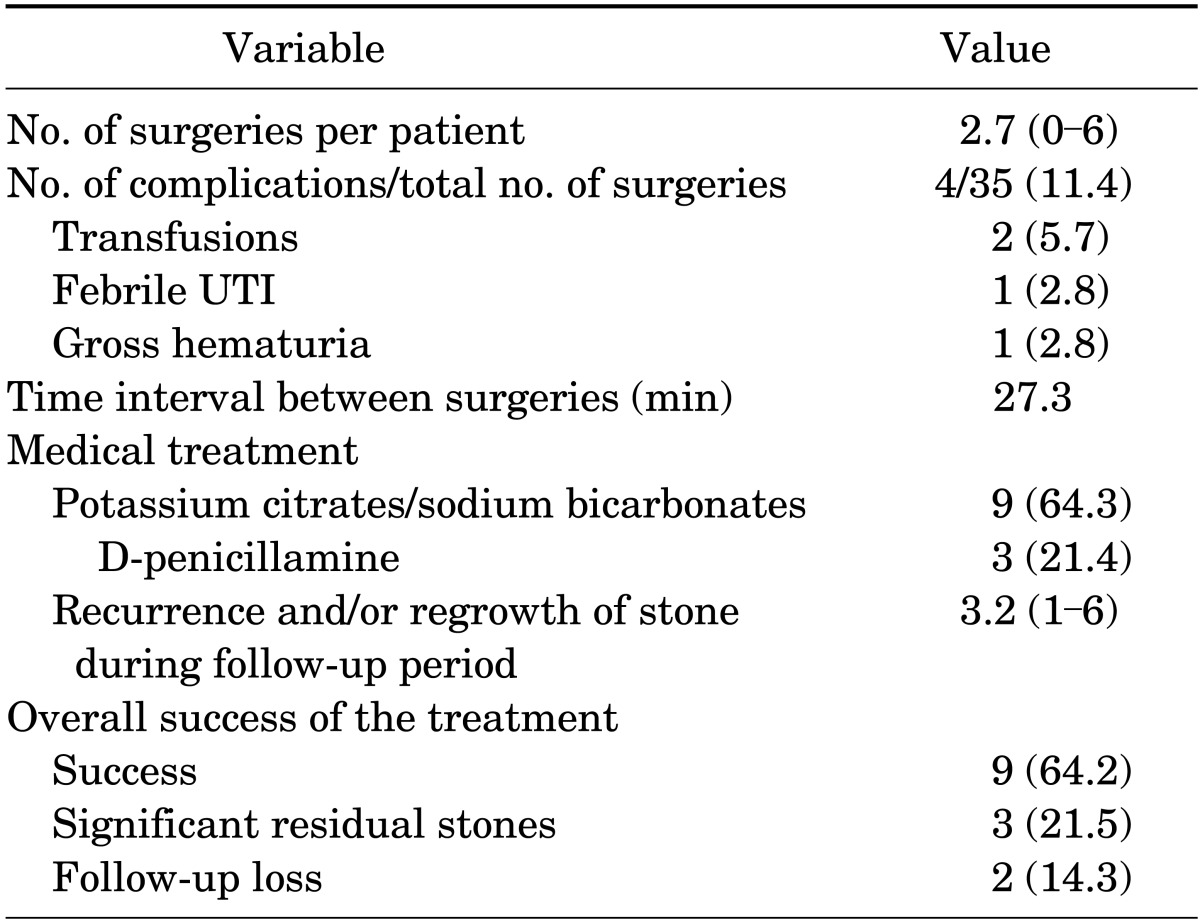
The mean age of our patients at their first visit was 19.6±5.0 years, and eight patients were males. The median stone burden and mean urine pH before each surgery were 6.5 cm2 and 6.5±0.9, respectively. Two patients had a family history of cystine stones. Patients underwent surgery an average of 2.7 times. The median interval between surgeries was 27.3 months, and 1 open surgery, 12 percutaneous nephrolithotomies, and 25 ureterorenoscopies were performed. Potassium citrate or sodium bicarbonate was used in nine cases. D-Penicillamine was continuously used in three patients. Patients had an average incidence of 3.2 recurrences or regrowth of stones during the median follow-up period of 60.5 months.
Cystinuria is an autosomal recessive genetic disorder that leads to defects in the transepithelial transporters for the dibasic amino acids, including cystine, ornithine, lysine, and arginine [1]. The urine concentrations of those amino acids in cystinuric patients become elevated as a result of impaired reabsorption from the renal proximal tubule [2]. However, of these dibasic amino acids, only cystine is relatively insoluble at physiological pH, which leads to crystal formation and, ultimately, stone disease [3]. More than 50% of patients with cystinuria show stone formation throughout their lifetime, as well as a high rate of recurrence of up to 60% [2]. Furthermore, more than three-quarters of cystinuric patients show a likelihood of bilateral stone formation [3]. Hence, these patients are at high risk of renal function impairment and consequent poor quality of life.
Cystine stones are relatively uncommon compared with other stone compositions, constituting just 1% to 2% of adult urinary tract stone diseases [4,5], and accounting for up to 10% of pediatric stone diseases [3]. Patients typically present with their first symptoms of cystine stones between 2 and 40 years of age with the peak age of onset in the third decade of life [6]. Incidence is equal between the genders, but male patients tend to present with symptoms earlier and also with more aggressive disease [7]. The prevalence of cystinuria is regionally variable, ranging from 1:1800 persons on the east coast of the Mediterranean to 1:100,000 persons in Sweden [3]. The estimated prevalence in the United States is 1:15,000 [6]. However, although there is a report by Turkish investigators that the prevalence of cystinuria in Asia is estimated as 1:1000 [8,9], there are very few reports on this issue among populations in Northeast Asia. Research from Japan reported a prevalence of cystine crystalluria of 1:16,000 [10], but it is still difficult to find recent reports on patient series from this region.
Because patients with cystinuria may develop serious problems with renal function and hence life quality owing to its high recurrence rate, appropriate principles for treatment plans and follow-up schedules should be established for these cases. Therefore, we report here our single-center experience of 14 cases of cystine stones to contribute to the development of such principles.
This study was performed with the approval and oversight of the Institutional Review Board at Asan Medical Center. We retrospectively reviewed the data for 14 patients diagnosed with cystine stones who visited our outpatient clinic between March 1994 and July 2012. Patient age at first visit, gender, family history, body mass index (BMI), presence of a single kidney, stone locations, stone burden, routine urinalysis, and urine culture results were the variables reviewed. In addition, the average number of repeated surgeries, complications, types of surgeries, intervals between repeated surgeries, shock wave lithotripsy (SWL), medical treatment, recurrences or regrowth of stones, and overall treatment success rates were also analyzed.
Stones were generally examined by computed tomography (CT) scans combined with abdominal plain films (kidney-ureter-bladder, KUB), and the diameters of the stones were estimated before surgery. Most patients underwent surgery, SWL, or both to treat this condition, and the type of operation was determined by the stone location and burden. Either percutaneous nephrolithotomy (PCNL) or ureterorenoscopic lithotomy (URS) was performed, although there was one case of open surgery in our series.
PCNL was performed with a 26-Fr adult nephroscope and stones were fragmented by use of an ultrasonic lithotriptor, ballistic lithotripter, or holmium: yttrium-aluminium-garnet (YAG) laser. A 14-Fr Malecot nephrostomy tube was then placed at the end of the procedure. For URS, 6-Fr or 7.5-Fr semirigid scopes (Richard Wolf Medical Instruments Co., Vernon Hills, IL, USA) with a 3.5-Fr operative working channel, or two-way actively deflectable (270°/270°) flexible ureteroscopes (Richard Wolf Medical Instruments Co.; and Storz, Flex-X2, Tuttlingen, Germany) with 3-Fr dual working channels were used. Fragmentation of stones during URS was performed with 365- and 200-µm diameter holmium:YAG laser fibers for semirigid and flexible instruments, respectively.
Stone analyses were performed in all patients with a Fourier-Transform Infrared spectrometer (Perkin-Elmer, Überlingen, Germany) after surgery or if spontaneous stone passage occurred. If cystine stones were found, we recommended genetic testing and that the patients' siblings accompany them to the clinic. The patients' clinical outcomes were usually assessed by CT scans and KUB. Intravenous pyelographies were seldom used and were mostly performed during the early part of our current study period. The definition of recurrence or regrowth of stones was a newly appeared stone or stones that became larger than a previous finding as seen in the image during the follow-up period. The overall success of treatment was defined as either no visible residual stones or the presence of remnant stones smaller than 2 mm in diameter on a postoperative KUB image or CT scan performed on the last day of follow-up.
Potassium citrate (1,000 mg three times a day) or sodium bicarbonate (500 mg four times a day) was recommended for all patients after diagnosis. D-Penicillamine (250 mg twice a day) was recommended for recurrent cases despite urine alkalization therapy.
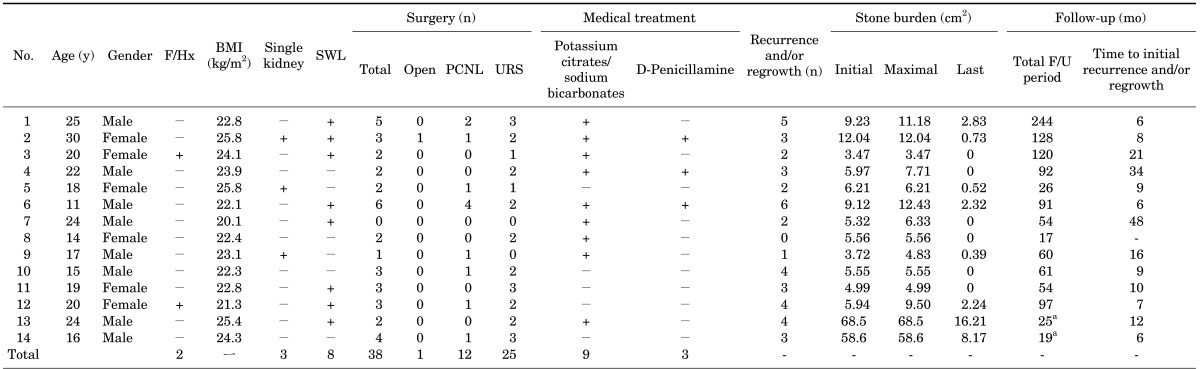
The mean age of our study patients at the first visit was 19.6 years and 8 patients (57.1%) were male. We identified 23 calyceal stones (41.1%), 2 pelvic stones (3.6%), and 31 ureteral stones (55.3%) in our cohort of 14 patients. The median stone burden was 6.7 cm2. Two patients (14.3%) had a family history of cystinuria and 3 patients (21.4%) had a single kidney at the first visit. Among the patients with a single kidney, all patients had a unilateral non-functioning kidney before the visit to our clinic. One patient with a single kidney had undergone a simple nephrectomy because the patient's right kidney was found to have no function following a Tc-99m diethylene triamine penta-acetic acid renal scan and the patient had a complete staghorn stone causing right flank pain. Eight patients underwent SWL regardless of surgery or as an adjunctive treatment method. A list of the patients, their demographic characteristics, and stone locations are detailed in Tables 1 and 2.
A total of 38 surgeries were performed among our 14 patient series. Among these were 12 PCNL, 25 URS, and 1 open surgery procedures. PCNL was repeated up to four times in one patient and three times in three URS cases. Only one cystinuric patient in our series did not undergo surgery at our institution. However, this patient had undergone several URS sessions at other hospitals before visiting our outpatient clinic and is currently receiving only potassium citrate treatment.
The mean number of repeat surgeries per patient was 2.7 during the median follow-up period of 60.3 months. One patient underwent six repeated surgeries including four PCNL and two URS procedures (Table 2). A total of 4 complications were observed over 35 procedures: 2 cases of transfusion, 1 case of febrile urinary tract infection (UTI), and 1 case of gross hematuria. Transfusions were required after PCNL. Both febrile UTI and gross hematuria occurred in patients who underwent URS. No additional treatments were necessary to manage the patients who developed complications.
The median interval between repeat surgeries was 27.3 months (interquartile range, 10.1-42.9 months). Medications were recommended for all patients after the diagnosis had been made by stone analysis, but only 9 patients (64.3%) continuously followed the medication regimen with good compliance. Of these, six patients took potassium citrate and three took sodium bicarbonate for urine alkalization. Furthermore, three patients were prescribed a thiol medication, D-penicillamine, in addition to urine alkalizers. Patients with cystine stones suffered from multiple recurrences or regrowth of stones (mean number, 3.2) during the follow-up period. Nine patients (64.2%) had either no visible stones or no significant residual stones and two patients were lost to follow-up. Overall treatment outcomes are summarized in Table 3.
Patients with cystinuria are reported to present their first typical symptomatic stone between 2 and 40 years of age, with a median age of onset of 12 and 15 years in female and male patients, respectively [6]. In addition, the incidence of cystinuria has been found to be comparable in both genders in most previous studies [2,7]. Although the age at first visit did not reflect the exact timing of symptom onset, the mean age of our patients at their first outpatient visit was 19.6 years, which is slightly higher than that of previous reports.
Previous studies have reported that male patients tend to have a more aggressive cystinuric disease course with a significantly higher number of stones and an earlier onset of symptoms [1,2,7]. In our current analysis, male patients were slightly younger (19.2 years vs. 20.2 years), had undergone more repeat surgeries (2.9 vs. 2.5), and showed more frequent recurrences or regrowth of stones (3.5 vs. 2.3). There was almost no difference between the stone burdens of our male and female patients (23.0 cm2 vs. 23.7 cm2). However, none of these comparisons showed statistical significance, likely because of the small number of cases (data not shown).
Because cystinuria is a genetic disorder, family histories are very important in the management of affected patients. Cystinuria is an autosomal recessive disease, but some heterozygote carriers have an autosomal dominant, incomplete penetrance appearance with increased, but typically normal, urinary cystine excretion [1]. Therefore, the first classification of cystinuria by Rosenberg et al. [11] was based on phenotypic characteristics. They classified cystinuric patients into three subgroups: type I, type II, and type III (the latter two are referred to as non-type I). Type I is characterized by its autosomal recessive, normal urinary cystine excretion pattern (0-100 mmol of cystine/g creatinine), whereas non-type I is considered to be an autosomal dominant disorder with incomplete penetrance and a slightly higher risk of stone formation [2,11,12]. However, a new classification of the disease has been proposed by Dello Strologo et al. [7] on the basis of the type of the mutation. These authors reported that the SLC3A1 gene in chromosome 2 and the SLC7A9 gene on chromosome 19 are mutated in type A and type B cystinuric patients, respectively. In our current data, the family history was identified in only two patients, probably because of autosomal recessive inheritance or incomplete penetrance.
The main treatment aims for patients with cystine stones are complete stone clearance, prevention of stone recurrence, and preservation of renal function. Therefore, establishing appropriate treatment plans that combine medical or surgical treatment with a regular follow-up schedule is paramount. In this regard, multimodal approaches that include SWL, URS, and PCNL have been suggested as primary therapies for treating patients with cystine stones [2].
Ahmed et al. [13] have suggested SWL, URS, and PCNL as an initial approach for stones smaller than 12 mm, 12-20 mm, and larger than 20 mm, respectively. In our present study, the surgical approaches were determined in accordance with the size and location of the stones. Stones larger than 20 mm were usually managed by PCNL as an initial approach, whereas stones between 15 mm and 20 mm were treated by using either PCNL or multiple URS sessions, depending on stone location and size.
Because many patients with cystinuria usually undergo repeat surgeries, surgical complications can be an important issue. One previous study reported a complication rate associated with PCNL in patients with cystine stones of 15.4% [14]. Another study reported an overall complication rate of 23.8% for URS [15]. The complication rate we observed in the present series was 11.4%, but none of these complications were major and thus no additional procedures were needed to manage them.
The aims of medical treatment for cystinuric patients are to prevent recurrences and to dissolve existing stones, thereby supplementing surgery or SWL. Hydration, a low-sodium diet, urine alkalization, and thiol drugs comprise the main aspects of treatment for cystinuria. However, thiol medications that are used to treat cystinuric patients, such as D-penicillamine and tiopronin, have several adverse effects, including alteration of taste perception, muco-cutaneous lesions, proteinuria due to nephrotic syndrome, and various other immune-mediated diseases [2]. Poor compliance is an issue for these therapies, probably because of these adverse effects as well as the different socioeconomic situations of the patients [16]. Treatment with potassium citrate or sodium bicarbonate is recommended for all cystinuric patients, and D-penicillamine is recommended in cases refractory to other therapies. However, only 9 of 14 patients were compliant for such treatment regimens in our current study cohort.
The number of recurrences or regrowth of stones during follow-up in each of our patients varied widely, from none to six. Patients with no recurrence underwent two sessions of URS and consistently followed our treatment regimen, including potassium citrate medications and the follow-up schedule. In contrast, patients with six incidences of recurrence or regrowth of stones were noncompliant with their treatment regimens for both medication and the follow-up schedule.
A previous study reported an overall success rate of PCNL in children with cystine stones of 63.1% [14]. Another previous study reported a success rate of 71% in patients with cystine stones who underwent URS [15]. Although there are some differences in the definition of treatment success, the success rate among our current patient series (64.3%) is comparable with previous results. The definition of treatment success in previous studies was the absence of any residual stones regardless of size, whereas a residual stone smaller than 2 mm in diameter was included in our category of treatment success herein. However, because previous reports have routinely evaluated treatment results by KUB or ultrasonography of the abdomen instead of CT scanning, complete stone clearance might have been overestimated. In contrast, we routinely performed CT scans as part of our follow-up protocol. Furthermore, we have shown here the results of a multimodal treatment approach in patients with cystine stones rather than reporting the results of only one treatment modality.
Our study had some limitations of note. Our analyses were retrospective and we did not perform genetic studies on all patients to determine the type of cystinuria or to evaluate the different responses to treatments, especially medications. Despite these limitations, our current report is the first study to report the characteristics as well as the relatively successful treatment outcomes in a cohort of patients with rare cystinuria from Northeast Asia. Further prospective, multicenter studies of a larger number of patients, including studies assessing the efficacy of different medications, are needed to evaluate these treatment outcomes more accurately.
Patients with cysteine stones have high recurrence or regrowth rates and relatively large stone burdens with an earlier age of onset. Successful management of cystinuria thus requires a strict and regular follow-up schedule, appropriate multimodal approaches, and high patient compliance, especially in relation to medications, to prevent recurrent stone formation. Additional research is needed to determine adequate treatment strategies for this condition, including surgical and medical therapies, to eventually prevent deterioration of renal function in affected patients.
References
1. Saravakos P, Kokkinou V, Giannatos E. Cystinuria: current diagnosis and management. Urology. 2014; 83:693–699. PMID: 24246330.

2. Claes DJ, Jackson E. Cystinuria: mechanisms and management. Pediatr Nephrol. 2012; 27:2031–2038. PMID: 22281707.

3. Knoll T, Zollner A, Wendt-Nordahl G, Michel MS, Alken P. Cystinuria in childhood and adolescence: recommendations for diagnosis, treatment, and follow-up. Pediatr Nephrol. 2005; 20:19–24. PMID: 15602663.

4. Leusmann DB, Blaschke R, Schmandt W. Results of 5,035 stone analyses: a contribution to epidemiology of urinary stone disease. Scand J Urol Nephrol. 1990; 24:205–210. PMID: 2237297.

5. Pahira JJ. Management of the patient with cystinuria. Urol Clin North Am. 1987; 14:339–346. PMID: 3576855.

6. Rogers A, Kalakish S, Desai RA, Assimos DG. Management of cystinuria. Urol Clin North Am. 2007; 34:347–362. PMID: 17678985.

7. Dello Strologo L, Pras E, Pontesilli C, Beccia E, Ricci-Barbini V, de Sanctis L, et al. Comparison between SLC3A1 and SLC7A9 cystinuria patients and carriers: a need for a new classification. J Am Soc Nephrol. 2002; 13:2547–2553. PMID: 12239244.
8. Ozalp I, Coskun T, Tokol S, Demircin G, Monch E. Inherited metabolic disorders in Turkey. J Inherit Metab Dis. 1990; 13:732–738. PMID: 2246857.

9. Tanzer F, Ozgur A, Bardakci F. Type I cystinuria and its genetic basis in a population of Turkish school children. Int J Urol. 2007; 14:914–917. PMID: 17880288.

10. Ito H, Murakami M, Miyauchi T, Mori I, Yamaguchi K, Usui T, et al. The incidence of cystinuria in Japan. J Urol. 1983; 129:1012–1014. PMID: 6406687.

11. Rosenberg LE, Downing S, Durant JL, Segal S. Cystinuria: biochemical evidence for three genetically distinct diseases. J Clin Invest. 1966; 45:365–371. PMID: 5904553.

13. Ahmed K, Khan MS, Thomas K, Challacombe B, Bultitude M, Glass J, et al. Management of cystinuric patients: an observational, retrospective, single-centre analysis. Urol Int. 2008; 80:141–144. PMID: 18362482.

14. Onal B, Dogan C, Citgez S, Argun B, Onder AU, Sever L, et al. Percutaneous nephrolithotomy in children with cystine stone: long-term outcomes from a single institution. J Urol. 2013; 190:234–237. PMID: 23313363.

15. Ruggera L, Zanin M, Beltrami P, Zattoni F. Retrograde transureteral approach: a safe and efficient treatment for recurrent cystine renal stones. Urol Res. 2011; 39:411–415. PMID: 21193905.

16. Ahmed K, Dasgupta P, Khan MS. Cystine calculi: challenging group of stones. Postgrad Med J. 2006; 82:799–801. PMID: 17148700.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download