Abstract
Brain and skin metastasis from urothelial carcinoma of the bladder is rare. There have been few case reports of the clinical course of patients with metastatic urothelial carcinoma of the brain and skin. In the present case, a 60-year-old man had undergone radical cystectomy with an ileal conduit owing to urothelial carcinoma (T1N0M0). The patient developed dizziness 9 years later and a solitary brain tumor was discovered in his left cerebellar hemisphere. The tumor was totally resected and the mass was verified to be metastatic urothelial carcinoma. One year after the metastasectomy of the brain lesion, multiple erythematous nodular lesions developed on his abdominal skin. The skin lesions were excised and verified to be metastatic urothelial carcinoma. This report describes this case of urothelial carcinoma of the bladder that metastasized to the brain and abdominal skin.
Bladder cancer is the second most common malignancy of the genitourinary tract in Korea. Bladder cancer has variable metastatic potential and almost any organ can be involved by metastasis. Lymph nodes, liver, lung, and bone are the most common metastatic sites of urothelial carcinoma of the bladder, with skin, brain, heart, and kidney being rare sites of metastasis [1-3]. We report a case of urothelial carcinoma of the bladder with brain and abdominal skin metastasis.
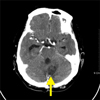
A 60-year-old man presented to the emergency room with severe dyspnea that had developed 20 hours earlier. He had undergone a radical cystectomy with an ileal conduit 10 years previously. Postoperative pathological results revealed urothelial carcinoma of stage T1N0M0 (Fig. 1A). After discharge, the patient had failed to attend routine follow-up visits for 8 years. After 8 years, he presented to the outpatient clinic with complaints of urethral bleeding. A urethroscopic biopsy revealed recurred urothelial carcinoma. After a radiologic work-up, he received three cycles of systemic combination chemotherapy with gemcitabine and cisplatin for urothelial carcinoma metastasized to the lungs, both inguinal lymph nodes, and both iliac chain lymph nodes. However, the lymphadenopathy was so aggravated that the response to systemic chemotherapy seemed to be ineffective. One year later, computed tomography (CT) was performed to evaluate dizziness. Brain CT revealed a 3×4 cm sized mass in the left cerebellar hemisphere (Fig. 2). A metastasectomy was performed and the mass proved to be metastatic urothelial carcinoma (Fig. 1B).
The patient was admitted for palliative treatment. Physical examination revealed multiple, 1-cm, erythematic nodular abdominal skin lesions (Fig. 3). Other findings from the physical examination were unremarkable. Laboratory findings were inconclusive. He underwent excisional biopsy of the skin lesions and the final histopathologic report was consistent with metastatic urothelial carcinoma (Fig. 1C). He died from acute respiratory distress syndrome the day after the excisional biopsy.
Bladder cancer is commonly a disease of older age and is a common malignant disease of the urinary tract [1-4]. The Korea National Statistical Office reported that an estimated 3,230 new cases of bladder cancer occurred in 2008 in Korea with 1,007 deaths. Bladder cancer has variable metastatic potential and almost any organ can be involved by metastasis [4]. Babaian et al. [5] reported that evidence of metastatic disease was found in a postmortem examination in approximately two thirds of patients with bladder cancer. The incidence of clinically detected distant metastases from urothelial carcinoma of the bladder reportedly ranges from 9.5% to 29% [1,6]. Lymph nodes, liver, lung, bone, and peritoneum are the most common metastatic sites of urothelial carcinoma of bladder, whereas skin, brain, heart, and kidney are rarely involved [1-3]. Only 7 cases of skin metastasis from bladder cancer have been reported in Korea [7].
The first step in the metastasis of urothelial carcinoma of the bladder is local lymphatic spread into the obturator, superior gluteal, inferior gluteal, external iliac, and common iliac nodes. Then, tumor cells disseminate through the para-aortic lymphatic chain to the thoracic duct and enter the general circulation. When the local nodes become obstructed, lymphohematogenous spread occurs by tumor cells shunted into the vascular compartment. Hematogenous metastases spread either via the pelvic plexus into the inferior vena cava and general circulation or via the perivertebral vein into the azygos, hemiazygos, intercostals, and other systemic veins [6].
Skin and brain metastases from urothelial carcinoma of the bladder are relatively rare [3]. According to the Brain Tumor Registry of Japan, only 0.6% of metastatic brain tumors were from bladder cancers [8]. In another study, central nervous system metastases were found in fewer than 1% of cases [1]. Urothelial carcinoma metastasizes to the brain hematogenously, and cancer cells are filtered by the lungs. Therefore, brain metastasis may be secondary to pulmonary metastasis. Many patients with brain metastases die before the brain lesion becomes manifest. Mueller et al. [9] found that among 10,417 cases of cutaneous metastases, only 1.1% represented a primary urologic lesion. Like brain metastasis, Spector et al. [10] suggested that skin metastasis in urothelial carcinoma of the bladder is a result of increased longevity in successfully treated patients. There are four mechanisms of metastatic dissemination by which the skin may be involved: 1) direct invasion from an underlying neoplasm, 2) iatrogenic implantation from an operation, 3) lymphatic spread, or 4) hematogenous spread [2,9]. In this case, similar to a patient reported by Ku et al. [8], skin metastasis was likely by hematogenous spread rather than other mechanisms. However, brain and skin metastasis is regarded as a late manifestation of systemic spread. The mean survival period of most patients with bladder cancer is relatively too short for manifestations of brain or skin metastatic lesions to develop. Thus, our case suggests that brain or skin may be rare sites for metastatic lesions.
Major advances have occurred in the diagnosis of bladder cancer and metastatic disease since the early 1990s [4]. New, effective, aggressive, multi-therapeutic approaches to bladder cancer involving radical operation and systemic combination chemotherapy are prolonging the survival period [1]. These developments are likely to make encountering patients who have uncommon metastatic lesions from urothelial carcinoma of the bladder, such as brain or skin metastasis, a more frequent occurrence. Therefore, clinicians should recognize the importance of a thorough physical examination including neurologic function and a general exam in patients with urothelial carcinoma.
Figures and Tables
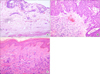
FIG. 1
(A) A representative section of the urinary bladder shows high-grade urothelial carcinoma. The tumor cells are arranged in small nests or cords and discontinuously invade into deep portions of the lamina propria (H&E, ×100). (B) The brain mass of the cerebellum shows metastatic carcinoma with tumor cells in a broad cord or sheet arrangement, identical to a urinary bladder tumor (H&E, ×200). (C) The excisional biopsied skin the abdomen shows individually scattered and nested pleomorphic tumor cells in the dermis, which is consistent with metastatic urothelial carcinoma (H&E, ×200).
References
1. Wakisaka S, Miyahara S, Nonaka A, Asami N, Kinoshita K, Kohriyama K. Brain metastasis from transitional cell carcinoma of the bladder: case report. Neurol Med Chir (Tokyo). 1990. 30:188–190.
2. Swick BL, Gordon JR. Superficially invasive transitional cell carcinoma of the bladder associated with distant cutaneous metastases. J Cutan Pathol. 2010. 37:1245–1250.
3. Atmaca AF, Akbulut Z, Demirci A, Belenli O, Alici S, Balbay DM. Multiple subcutaneous nodular metastases from transitional cell carcinoma of the bladder. Pathol Oncol Res. 2007. 13:70–72.
4. Shinagare AB, Ramaiya NH, Jagannathan JP, Fennessy FM, Taplin ME, Van den Abbeele AD. Metastatic pattern of bladder cancer: correlation with the characteristics of the primary tumor. AJR Am J Roentgenol. 2011. 196:117–122.
5. Babaian RJ, Johnson DE, Llamas L, Ayala AG. Metastases from transitional cell carcinoma of urinary bladder. Urology. 1980. 16:142–144.
6. Goldman SM, Fajardo AA, Naraval RC, Madewell JE. Metastatic transitional cell carcinoma from the bladder: radiographic manifestions. AJR Am J Roentgenol. 1979. 132:419–425.
7. Oh SH, Lee WJ, Rhee DY, Chang SE, Lee MW, Choi JH, et al. A case of cutaneous metastasis from urothelial carcinoma of the urinary bladder. Korean J Dermatol. 2007. 45:401–403.
8. Ku JH, Yeo WG, Park MY, Lee ES, Kim HH. Metastasis of transitional cell carcinoma to the lower abdominal wall 20 years after cystectomy. Yonsei Med J. 2005. 46:181–183.
9. Mueller TJ, Wu H, Greenberg RE, Hudes G, Topham N, Lessin SR, et al. Cutaneous metastases from genitourinary malignancies. Urology. 2004. 63:1021–1026.
10. Spector JI, Zimbler H, DeLeo M, Ross JS. Skin metastases from transitional cell bladder cancer. Urology. 1987. 29:215–217.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download