Abstract
Purpose
The primary objective was to assess whether transrectal ultrasound (TRUS)-guided prostate biopsy in the left lateral decubitus (LLD) position differed from the procedure in the lithotomy position regarding patients' pain perception. The secondary objective was to assess the analgesic effect of intrarectal 2% lidocaine gel in this setting.
Materials and Methods
This single-center, open-label trial enrolled 148 men undergoing prostate biopsy. Then men were randomly assigned to group 1 (LLD position, no lidocaine, n=50, "test"), group 2 (lithotomy position+lidocaine, n=50, "positive control"), and group 3 (lithotomy position, no lidocaine, n=48, "negative control"). Twelve-core samples were taken in each biopsy set. Pain was assessed by using a 10-point visual analogue scale (VAS).
Results
Across the groups, patients were comparable regarding age, prostate-specific antigen levels, prostate volume, digital rectal examination findings, and pathohistological diagnosis. VAS scores were lower in group 1 (median, 2.95) than in group 2 (median, 4.95; p<0.001) or group 3 (median, 4.60; p<0.001). The difference between group 2 and group 3 was insignificant (p=0.268). The adjusted mean differences (with adjustment for the above covariates) were as follows: group 1 vs. group 2, -1.43 (95% confidence interval [CI]: -2.25 to -0.60; p<0.001); group 1 vs. group 3, -1.22 (95% CI: -2.04 to -0.41; p=0.001); group 2 vs. group 3, 0.20 (95% CI, -0.63 to 1.04; p=0.836); and group 1 vs. groups 2 and 3, -1.33 (95% CI, -1.92 to -0.73; p<0.001). The procedure was comparably well tolerated across the groups.
Prostate carcinoma is one of the most common malignant diseases in men. In Croatia, the annual incidence rate has been estimated at 79.2/100,000 [1]. Introduction of prostate-specific antigen (PSA) testing and, particularly, transrectal ultrasound (TRUS)-guided prostate biopsy have greatly improved the detection of prostate cancer [2]. Biopsy can be performed in different patient positions, i.e., the lithotomy position, the lateral decubitus position, or the knee-chest position [3], and typically, 10, 12, or even more core samples are taken [4]. Sampling of a greater number of biopsy cores causes some degree of discomfort or pain in most patients [5,6].
One randomized trial indicated that intrarectal application of 2% lidocaine gel prior to biopsy was a simple, safe, and effective analgesic method for this purpose [7]. However, a recent meta-analysis of 5 other randomized trials comparing intrarectal lidocaine gel with a placebo gel or no treatment [8] and two subsequent trials comparing lidocaine gel with no treatment [9,10] failed to detect a pain-relieving effect of this intervention. Also, a recent randomized trial suggested that pain perception in patients undergoing prostate biopsy might be less profound in the left lateral decubitus (LLD) position than in the lithotomy position [11], whereas another one did not [12].
Our standard procedure has been systematic 12-core prostate biopsy in the lithotomy position with the intrarectal placement of 10 ml of 2% lidocaine gel 5 minutes prior to the procedure. Considering the conflicting reports on pain perception in the lateral decubitus vs. lithotomy position [11,12] and the analgesic effects of intrarectal anesthetic gel [7-10], the primary objective of the present study was to evaluate pain perception in patients undergoing prostate biopsy in the LLD position compared with the lithotomy position, and the secondary objective was to evaluate the analgesic effect of intrarectal 2% lidocaine gel.
This prospective, randomized, single-center, open-label trial (with blinded data analysis) was performed between February 2008 and July 2010 in General Hospital Varazdin, Croatia. Consecutive eligible patients were randomly assigned to one of three groups: group 1, biopsy performed in the LLD position without topical lidocaine ("test" treatment); group 2, biopsy performed in the lithotomy position with intrarectal application of 10 ml of 2% lidocaine gel 5 minutes before the procedure (our standard procedure, "positive control" treatment); and group 3, biopsy performed in the lithotomy position without topical lidocaine ("negative control" treatment).
In the five trials embraced by the recent meta-analysis [8] and two subsequent trials [9,10], pain scores on a 10-point visual analogue scale (VAS) in patients undergoing prostate biopsy with or without intrarectal anesthetic gel averaged between 3 and 5.6 with standard deviations (SDs) between 1.5 and 2.7. In an analysis of variance with 3 treatment groups, assuming a mean VAS score of 5 under the null hypothesis and an SD of 2.5, a total of 126 patients (42 per group) would provide 81% power at the overall 0.05 alpha level to detect a mean difference of 1.5 VAS score points between any two treatments. The targeted detectable difference (1.5 points) was set arbitrarily but accounted for the fact that the effect of the periprostatic nerve block vs. placebo has been estimated at around 2.1 score points and at around 1.5 score points as compared with intrarectal lidocaine [8]. Considering a possible imprecision of the variability estimate, we decided to enroll a total of 150 patients (50 per group) to ascertain at least 80% power for detection of the targeted difference.
The randomization list was generated by using the permutated block method (block size 6) and was concealed from the patient-enrolling investigators (confined with a registered nurse assisting in the procedure but not participating in the study). When a patient met the inclusion and exclusion criteria, the assigned treatment was disclosed.
Inclusion criteria were as follows: 1) indication for a prostate biopsy (elevated PSA or PSA velocity ≥0.75 ng/ml) or an abnormal digital rectal finding, 2) no previous prostate biopsy, and 3) informed consent. Exclusion criteria were: 1) concomitant anorectal disease, 2) current treatment with analgesics, 3) impaired intellectual ability (inability to understand the informed consent), and 4) contraindications for the lithotomy position (e.g., hip joint disease or a contracture).
All biopsies were performed by the same investigator (a qualified urologist) on a Siemens Sonoline SL-1 ultrasound device with Siemens Endo-P Sonde Biplane, US Biopsy 18G Biopsyneedle, and Promag 2.2 Automatic Biopsy System and were systematic 12-core biopsies (all cores were obtained from the lateral areas of the prostate, 2 from the base, 2 from the mid-lobe, and 2 from the apex on each side).
Antibiotic prophylaxis (2×500 mg oral ciprofloxacin/day) was started the night before the procedure and was extended for 4 days.
Immediately after the procedure, patients' pain perception was assessed by using a 10-point VAS (0, no pain; 10, excruciating pain). All patients were outpatients and were discharged after a 2-hour post-biopsy observation. They were scheduled for a regular visit with urinalysis 7 days after biopsy. All other visits or procedures were performed on an "as-needed" basis.
Blinded data analysis was performed by an investigator not included in the clinical part of the trial. Considering the trial objectives, the comparisons of interest were between group 1 (LLD position, "test") and groups 2 and 3 (lithotomy position with or without lidocaine gel, i.e., "positive control" and "negative control" control, respectively) and between group 2 and group 3. Univariate comparisons were performed by using Kruskal-Wallis nonparametric analysis of variance with adjustment for three pair-wise comparisons (Dunn's test). Because in a multivariate analysis (adjustment for age, PSA value, prostate volume, pathohistological diagnosis, and digital rectal finding), residuals of the VAS scores showed a normal distribution, a general linear model was fitted to the data to obtain adjusted (least-square, LS) means and LS-mean differences between the groups with Tukey-Kramer adjustment for multiple comparisons. Because the LS-means for group 2 and group 3 were practically identical, an additional analysis was done in which group 1 (LLD position) was compared with groups 2 and 3 cumulatively (lithotomy position). We used STATA ver. 9.0 (StataCorp LP, College Station, TX, USA) software.
Two patients randomly assigned to group 3 (lithotomy position, no lidocaine) decided not to participate in the trial; hence, a total of 148 patients were included. Patients in the three groups were generally comparable regarding age, PSA levels, prostate volume, digital rectal findings, and pathohistological diagnosis (Table 1).
In the univariate analysis, VAS pain scores in group 1 (LLD position, no lidocaine; median, 2.95) were significantly lower than in either group 2 (lithotomy position+lidocaine; median, 4.95) or group 3 (lithotomy, no lidocaine; median, 4.60), whereas the difference between groups 2 and 3 was insignificant (Table 2).
After adjustment for the factors depicted in Table 1, VAS pain scores in group 1 remained significantly lower than in group 2 or group 3, whereas there was practically no difference between group 2 and group 3 (Table 3).
The biopsy was comparably well tolerated across the groups. Two patients in group 3 experienced minor rectal bleeding during the post-biopsy observational period. One patient in group 1 and one in group 3 developed a febrile uroinfection, which responded well to antibiotics and subsided within 2 weeks after the procedure. Hematuria was observed in 17/50 patients (34%) in group 1, 20/50 patients (40%) in group 2, and 15/48 patients (31%) in group 3, all resolving within 2 weeks after biopsy. Minor complications such as hematospermia were not noted.
TRUS-guided prostate biopsy has greatly improved the diagnosis of prostate cancer because it is a highly sensitive and specific method that is generally (regardless of the performance modalities) safe and well tolerated [13]. The major disadvantages of the procedure are anal discomfort, largely due to the insertion of the ultrasound probe; pain, predominantly induced by the needle penetration through the prostate capsule; and a certain level of psychological stress [14], largely related to the nature of the procedure (e.g., patient's position, anal insertion of the probe, the possibility of a malignant disease). Regarding pain management, the guidelines of the European Association of Urology suggest periprostatic block as a state of the art method [13]. Periprostatic block is more effective and apparently at least equally as safe and well tolerated as application of topical anesthetic gel or no local analgesic treatment [8]. Nevertheless, it may have complications, such as repeated injections during the biopsy, systemic lidocaine toxicity, urinary incontinence, and, occasionally, degradation of the image resolution due to anesthetic injection [15,16]. Therefore, other methods may still be considered legitimate, particularly because the level of pain induced by the biopsy is, at worst, moderate in most patients.
Topical intrarectal application of anesthetic gels (e.g., 2% lidocaine) has been traditionally considered to relieve anal discomfort, but a recent meta-analysis of randomized trials [8] and two subsequent trials [9,10] indicated a lack of an analgesic effect. The present data are in line with these observations. The evaluation of lidocaine gel in the present trial would have attained a higher level of evidence had we used a placebo gel and a full 2×2 factorial design (i.e., combination of patient positions and gel), but this was not the primary objective of this study. From the methodological standpoint (randomization, accounting for potential confounders), the present observations should be viewed as a fair contribution to the body of evidence [8-10] indicating a lack of efficacy of topical lidocaine in this setting.
The main finding of the present trial is a lower intensity of pain in patients undergoing prostate biopsy in the LLD position than in the lithotomy position (with or without intrarectal lidocaine gel) as assessed on a 10-point VAS immediately after the procedure. By size, the observed adjusted differences (around 1.4 score points vs. the lithotomy position with 2% lidocaine gel, around 1.2 score points vs. the lithotomy position without lidocaine, and around 1.3 score points vs. cumulative lithotomy position) are similar to those between periprostatic nerve block and intrarectal anesthetic gel (around 1.5 score points) [8] and should therefore be considered practically relevant. Similar observations were reported from a recent trial in which 340 patients were randomly assigned to undergo prostate biopsy either in the LLD or lithotomy position without further topical analgesic treatment [11], but another smaller trial (total n=70) [12] reported less pain in the lithotomy position than in the LLD position. There appears to be no plausible explanation for the discrepancy between the current and some of the published [11] vs. other published data [12], except for the fact that all three trials were single-center trials and that under such conditions, observations in smaller trials could be by chance (due to sampling variability). It should be noted, however, that in the present trial the "effect of patient position" was consistently significant in statistical terms and practically relevant by size in both univariate comparisons and after adjustment for potentially relevant covariates. Taken together, the present and the published data [11,12] strongly suggest that patients' pain perception during TRUS-guided prostate biopsy in the LLD position might be relevantly lower than in the lithotomy position, and this topic thus deserves further well-designed multicentric evaluations. The present data do not allow for a straightforward explanation of the beneficial "effect" of the LLD position. Perception of pain is a highly subjective psychological phenomenon and the methods commonly used in this setting (e.g., VAS scoring systems) evaluate exactly that-the subjective interpretation of painful stimuli that may be affected by a number of other psychological phenomena, particularly anxiety and depression, which are highly prevalent among patients undergoing prostate biopsy [14]. The lithotomy position could be more unpleasant or embarrassing than the LLD position, and therefore, the pain perception could be intensified; it is considered "gynecological" and "exposing" as compared to the LLD position, which is a more relaxed, physiological position typically used for sleep and rest. Therefore, it could be viewed as a stress-relieving position that could be beneficial during this relatively unpleasant procedure. Unfortunately, neither the present nor the published studies evaluated the levels of depression or anxiety concomitantly with the pain evaluation. We suggest that such evaluations in future studies could help us to understand the underlying mechanisms of the observed phenomena.
Figures and Tables
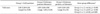
TABLE 3
Adjusted mean differences (with 95% confidence intervals, CI) between groups regarding visual analogue scale pain scores (multivariate analysisa)

Mean differences, confidence intervals, and p-values were determined with Tukey-Kramer adjustment for multiple comparisons.
LLD, left lateral decubitus.
a: General linear modelwas fitted to visual analogue scale scores (adjustments: age, prostate-specific antigen, prostate volume, pathohistological diagnosis, and digital rectal finding, all p>0.100).
ACKNOWLEDGEMENTS
We are thankful to Slaven Pikija, MD, Sinisa Car, MD and professor Vladimir Trkulja, MD, PhD, for their writing assistance.
References
1. Croatian National Institute of Public Health. accessed December 16, 2010. http://www.hzjz.hr/rak/novo.htm.
2. Stamey TA, Yang N, Hay AR, McNeal JE, Freiha FS, Redwine E. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med. 1987. 317:909–916.
3. Spirnak JP, Resnick MI. Gillenwater JY, Grayhack JT, Howards SS, Mitchell ME, editors. Ultrasound. Adult & pediatric urology. 2002. Philadelphia: Lippincott Williams & Wilkins;140.
4. Presti JC. Prostate biopsy: current status and limitations. Rev Urol. 2007. 9:93–98.
5. Clements R, Aideyan OU, Griffiths GJ, Peeling WB. Side effects and patient acceptability of transrectal biopsy of the prostate. Clin Radiol. 1993. 47:125–126.
6. Collins GN, Lloyd SN, Hehir M, McKelvie GB. Multiple transrectal ultrasound-guided prostatic biopsies-true morbidity and patient acceptance. Br J Urol. 1993. 71:460–463.
7. Issa MM, Bux S, Chun T, Petros JA, Labadia AJ, Anastasia K, et al. A randomized prospective trial of intrarectal lidocaine for pain control during transrectal prostate biopsy: the Emory University experience. J Urol. 2000. 164:397–399.
8. Tiong HY, Liew LC, Samuel M, Consigliere D, Esuvaranathan K. A meta-analysis of local anesthesia for transrectal ultrasound-guided biopsy of the prostate. Prostate Cancer Prostatic Dis. 2007. 10:127–136.
9. Díaz Pérez GA, Meza Montoya L, Morante Deza C, Pow-Sang Godoy M, Destefano Urrutia V. Pain during transrectal ultrasound guided needle biopsy of the prostate: comparison of the use or not of lidocaine gel. Actas Urol Esp. 2009. 33:134–137.
10. Song SH, Kim JK, Song K, Ahn H, Kim CS. Effectiveness of local anaesthesia techniques in patients undergoing transrectal ultrasound-guided prostate biopsy: a prospective randomized study. Int J Urol. 2006. 13:707–710.
11. Kilciler M, Demir E, Bedir S, Erten K, Kilic C, Peker AF. Pain scores and early complications of transrectal ultrasonography-guided prostate biopsy: effect of patient position. Urol Int. 2007. 79:361–363.
12. Bruyère F, Faivre d'Arcier B, Haringanji DC, Boutin JM, Haillot O, Lanson Y. Effect of patient position on pain experienced during prostate biopsy. Urol Int. 2007. 78:351–355.
13. Heidenreich A, Bolla M, Joniau S, Mason MD, Matveev V, Mottet N, et al. Guidelines on prostate cancer. EAU Guidelines. 2011. Arnhem: European Association of Urology.
14. Jadhav SA, Sukumar S, Kumar G, Bhat SH. Prospective analysis of psychological distress in men being investigated for prostate cancer. Indian J Urol. 2010. 26:490–493.
15. Von Knobloch R, Weber J, Varga Z, Feiber H, Heidenreich A, Hofmann R. Bilateral fine-needle administered local anaesthetic nerve block for pain control during TRUS-guided multi-core prostate biopsy: a prospective randomised trial. Eur Urol. 2002. 41:508–514.
16. Turgut AT, Olçücüoğlu E, Koşar P, Geyik PO, Koşar U. Complications and limitations related to periprostatic local anesthesia before TRUS-guided prostate biopsy. J Clin Ultrasound. 2008. 36:67–71.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download