Abstract
Purpose
With the recent changes in eating habits and the westernization of peoples' lifestyle, the occurrence of coronary artery disease is on the rise. In 1998, the World Health Organization (WHO) defined "metabolic syndrome" as a condition in which all the risk factors of coronary artery disease exist in an elderly individual. We investigated the relationship between metabolic syndrome and voiding difficulty.
Materials and Methods
In 2004, we investigated 123 male out-patients who visited the endocrinology department and the health care center between the months of March and October. We divided the patients into two groups: one group met the criteria for metabolic syndrome (n=90, 58.7±8.9 years old) and one group didn't met the criteria (n=33, 57.8±9.5 years old), and we compared factors of voiding difficulty between the these two groups.
Results
When comparing the components of metabolic syndrome in the patient study group to the control study group, the metabolic syndrome patients scored poorly for all the metabolic syndrome components in comparison to the control group (p<0.05). When comparing the voiding factors of the metabolic syndrome patients to the control group, the metabolic syndrome patient group scored substantially lower than the control group for all the voiding factors (p<0.05).
Conclusions
The results of this study proved that metabolic syndrome and voiding difficulty are related. Therefore, the earlier diagnosis of metabolic syndrome should be possible by performing a more active investigation for metabolic syndrome in the patients who are admitted with voiding difficulty.
Figures and Tables
Table 1
Comparison of factors of metabolic syndrome between the metabolic syndrome group and the control group
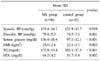
Table 3
Comparison of voiding dysfunction between the MS group and the control group, according to ICS standardization

References
1. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silvershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998. 97:1837–1847.
2. Fuster V, Pearson TA. 27th Bethesda Conference. Matching the intensity of risk factor management with the hazard for coronary disease events. J Am Coll Cardiol. 1996. 27:957–1047.
3. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.
4. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991. 14:173–194.
5. Rett K, Wicklmayr M, Mehnert H. New aspects of insulin resistance in hypertension. Eur Heart J. 1994. 15:Suppl C. 78–81.
6. Boon TA, Van Venrooij GE, Eckhardt MD. Effect of diabetes mellitus on lower urinary tract symptoms and dysfunction in patients with benign prostatic hyperplasia. Curr Urol Rep. 2001. 2:297–301.
7. Michel MC, Heemann U, Schumacher H, Mehlburger L, Goepel M. Association of hypertension with symptoms of benign prostatic hyperplasia. J Urol. 2004. 172:1390–1393.
8. Hammarsten J, Hogstedt B, Holthuis N, Mellstrom D. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998. 1:157–162.
9. Hammarsten J, Hogstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001. 39:151–158.
10. Matsuda T, Abe H, Suda K. Relation between benign prostatic hyperplasia and obesity and estrogen. Rinsho Byori. 2004. 52:291–294.
11. Hoepelman AI, Meiland R, Geerlings SE. Pathogenesis and management of bacterial urinary tract infections in adult patients with diabetes mellitus. Int J Antimicrob Agents. 2003. 22:Suppl 2. 35–43.
12. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.
13. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Excutive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
14. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998. 15:539–553.
15. The Asia-Pacific perspective: redefining obesity and its treatment. Western Pacific Regional Office of the World Health Organization, The International Obesity Task Force. 2000. Sydney: Health Communications Australia;http://www.obesityasiapacific.com.
16. Nugent AP. The metabolic syndrome. BNF Nutr Bull. 2004. 29:36–43.
17. Lym YL, Hwang SW, Shim HJ, Oh EH, Chang YS, Cho BL. Prevalence and risk factors of the metabolic syndrome as defined by NCEP-ATP III. J Korean Acad Fam Med. 2003. 24:135–143.
18. Landsberg L. Diet, obesity and hypertension: an hypothesis involving insulin, the sympathetic nervous system, and adaptive thermogenesis. Q J Med. 1986. 61:1081–1090.
19. Berne C, Pollare T, Fagius J. The sympathetic outflow in vasoconstrictor nerve fascicles to muscle is increased during euglycacemic hyperinsulinemia. Diabetologia. 1989. 32:Suppl. 465A.
20. Michel MC, Mehlburger L, Schumacher H, Bressel HU, Goepel M. Effect of diabetes on lower urinary tract symptoms in patients with benign prostatic hyperplasia. J Urol. 2000. 163:1725–1729.
21. Fonseca V, Seftel A, Denne J, Fredlund P. Impact of diabetes mellitus on the severity of erectile dysfunction and response to treatment: analysis of data from tadalafil clinical trials. Diabetologia. 2004. 47:1914–1923.
22. Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW. Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol. 2002. 168:599–604.
23. Giugliano F, Esposito K, Di Palo C, Ciotola M, Giugliano G, Marfella R, et al. Erectile dysfunction associates with endothelial dysfunction and raised proinflammatory cytokine levels in obese men. J Endocrinol Invest. 2004. 27:665–669.
24. Sugaya K, Kadekawa K, Ikehara A, Nakayama T, Gakiya M, Nashiro F, et al. Influence of hypertension on lower urinary tract symptoms in benign prostatic hyperplasia. Int J Urol. 2003. 10:569–574.
25. Saito M, Ohmura M, Kondo A. Effect of ageing on blood flow to the bladder and bladder function. Urol Int. 1999. 62:93–98.
26. Lau DH, Kommu S, Mikhailidis DP, Morgan RJ, Mumtaz FH. Re: the prevalence of hypertension, hyperlipidemia, diabetes mellitus and depression in men with erectile dysfunction. J Urol. 2005. 173:1050.
27. McNeal J. Pathology of benign prostatic hyperplasia. Insight into etiology. Urol Clin North Am. 1990. 17:477–486.
28. Shieh SM, Sheu WH, Shen DC, Fuh MM, Chen YD, Reaven GM. Glucose, insulin, and lipid metabolism in doxazosintreated patients with hypertension. Am J Hypertens. 1992. 5:827–831.
29. Pollare T, Lithell H, Selinus I, Berne C. Application of prazosin is associated with an increase of insulin sensitivity in obese patients with hypertension. Diabetologia. 1988. 31:415–420.
30. Swislocki AL, Hoffman BB, Sheu WH, Chen YD, Reaven GM. Effect of prazosin treatment on carbohydrate and lipoprotein metabolism in patients with hypertension. Am J Med. 1989. 86:14–18.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download