1. Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011; 186:540–544. PMID:
21683389.

2. Hanno PM, Burks DA, Clemens JQ, Dmochowski RR, Erickson D, Fitzgerald MP, et al. Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011; 185:2162–2170. PMID:
21497847.

3. Vasudevan V, Moldwin R. Addressing quality of life in the patient with interstitial cystitis/bladder pain syndrome. Asian J Urol. 2017; 4:50–54. PMID:
29264207.

4. Boucher M, Meen M, Codron JP, Coudore F, Kemeny JL, Eschalier A. Cyclophosphamide-induced cystitis in freely-moving conscious rats: behavioral approach to a new model of visceral pain. J Urol. 2000; 164:203–208. PMID:
10840460.

5. Edrees G, Luts A, Stewart F. Bladder damage in mice after combined treatment with cyclophosphamide and X-rays. The influence of timing and sequence. Radiother Oncol. 1988; 11:349–360. PMID:
3375461.

6. Stewart FA. Mechanism of bladder damage and repair after treatment with radiation and cytostatic drugs. Br J Cancer Suppl. 1986; 7:280–291. PMID:
3521706.
7. Arnold H, Bourseaux F, Brock N. Chemotherapeutic action of a cyclic nitrogen mustard phosphamide ester (B 518-ASTA) in experimental tumours of the rat. Nature. 1958; 181:931. PMID:
13526741.

8. Rubin JS, Rubin RT. Cyclophosphamide hemorrhagic cystitis. J Urol. 1966; 96:313–316. PMID:
5953127.

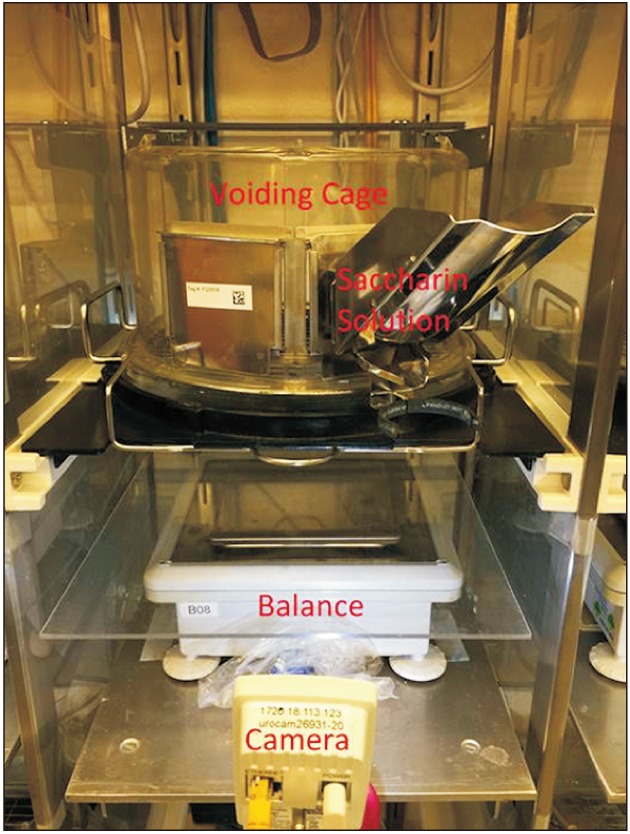
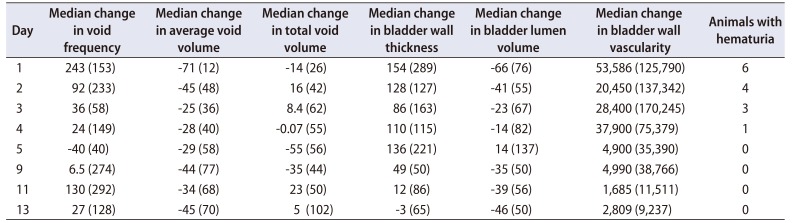
9. Wood R, Eichel L, Messing EM, Schwarz E. Automated noninvasive measurement of cyclophosphamide-induced changes in murine voiding frequency and volume. J Urol. 2001; 165:653–659. PMID:
11176453.

10. Wood RW, Baggs RB, Schwarz EM, Messing EM. Initial observations of reduced uroflow in transgenic adenocarcinoma of murine prostate. Urology. 2006; 67:1324–1328. PMID:
16765198.

11. Nicholson TM, Ricke EA, Marker PC, Miano JM, Mayer RD, Timms BG, et al. Testosterone and 17β-estradiol induce glandular prostatic growth, bladder outlet obstruction, and voiding dysfunction in male mice. Endocrinology. 2012; 153:5556–5565. PMID:
22948219.

12. Nicholson TM, Nguyen JL, Leverson GE, Taylor JA, Vom Saal FS, Wood RW, et al. Endocrine disruptor bisphenol A is implicated in urinary voiding dysfunction in male mice. Am J Physiol Renal Physiol. 2018; 315:F1208–F1216. PMID:
30019933.

13. Nicholson TM, Moses MA, Uchtmann KS, Keil KP, Bjorling DE, Vezina CM, et al. Estrogen receptor-α is a key mediator and therapeutic target for bladder complications of benign prostatic hyperplasia. J Urol. 2015; 193:722–729. PMID:
25167991.

14. Valenstein ES, Cox VC, Kakolewski JW. Polydipsia elicited by the synergistic action of a saccharin and glucose solution. Science. 1967; 157:552–554. PMID:
6028919.

15. Datta K, Chin A, Ahmed T, Qing WG, Powell KL, Simhambhatla P, et al. Mixed effects of 2,6-dithiopurine against cyclophosphamide mediated bladder and lung toxicity in mice. Toxicology. 1998; 125:1–11. PMID:
9585095.

16. Bjorling DE, Elkahwaji JE, Bushman W, Janda LM, Boldon K, Hopkins WJ, et al. Acute acrolein-induced cystitis in mice. BJU Int. 2007; 99:1523–1529. PMID:
17346276.

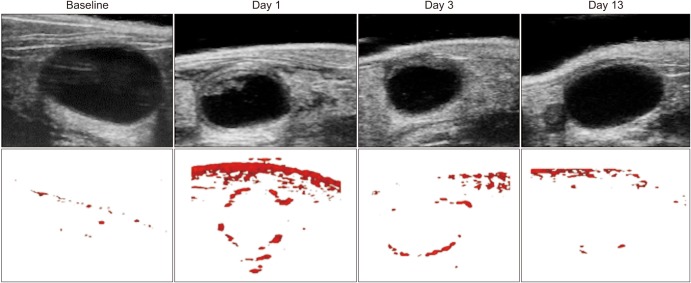
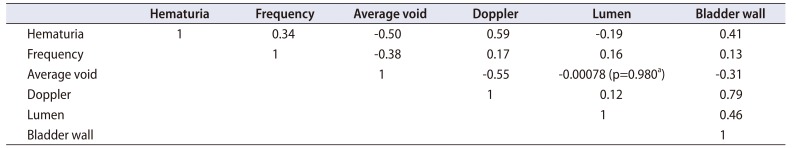
17. Wu SY, Jhang JF, Jiang YH, Kuo HC. Increased bladder wall thickness is associated with severe symptoms and reduced bladder capacity in patients with bladder pain syndrome. Urol Sci. 2016; 27:263–268.

18. Pontari MA, Hanno PM, Ruggieri MR. Comparison of bladder blood flow in patients with and without interstitial cystitis. J Urol. 1999; 162:330–334. PMID:
10411032.

19. Golubeva AV, Zhdanov AV, Mallel G, Dinan TG, Cryan JF. The mouse cyclophosphamide model of bladder pain syndrome: tissue characterization, immune profiling, and relationship to metabotropic glutamate receptors. Physiol Rep. 2014; 2:e00260. PMID:
24760514.

20. Ali MM, Ahmed AF, Khaled SM, Abozeid H, AbdelMagid ME. Accuracy of ultrasound-measured bladder wall thickness for the diagnosis of detrusor overactivity. Afr J Urol. 2015; 21:25–29.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download