Abstract
Purpose
Few studies have explored the treatment of isolated communicating hydroceles via scrotal incision. We prospectively evaluated the surgical outcomes of such treatment in boys with hydroceles compared with that using traditional, inguinal incision hydrocelectomy.
Materials and Methods
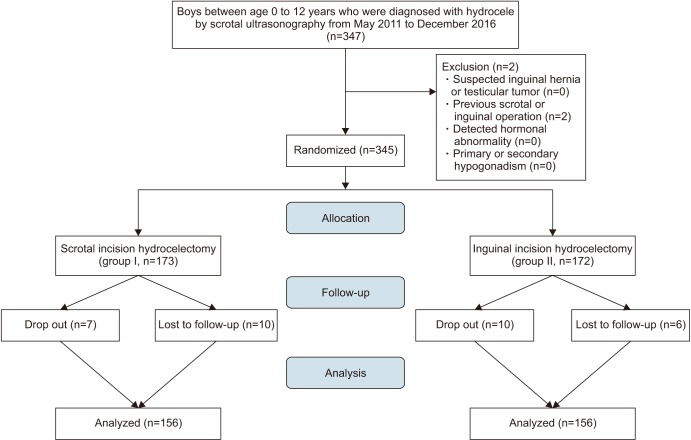
Of 347 boys aged 0–12 years who were diagnosed as hydrocele on ultrasonography, 173 boys were assigned to the scrotal incision hydrocelectomy group (group I, n=173) and 172 boys were assigned to the traditional inguinal incision hydrocelectomy group (group II, n=172), and finally 156 boys in group I and 156 boys in group II were included in this study. Surgical outcomes, including postoperative complications and hydrocele relapse rates, were compared between groups.
Results
The overall success rates were similar in both groups (group I, 96.8%; group II, 89.1%; p=0.740). The operation time and hospital stay were significantly shorter in group I (30.94±3.95 minutes and 3.94±0.30 days) than in group II (38.02±7.12 minutes and 4.24±0.99 days; p<0.001 and p=0.009, respectively). The postoperative complication rate was lower in group I than in group II (3.2% vs. 10.9%, p=0.740).
Conclusions
Scrotal incision hydrocelectomy in boys was associated with shorter operative time and hospital stay, and a lower postoperative complication rate, than was the inguinal incision approach. The scrotal incision technique might be an easy and effective alternative treatment when used to treat hydroceles in boys as well as inguinal incision approach.
A hydrocele is a pathological accumulation of fluid in the visceral and parietal layers of the tunica vaginalis of the scrotum or along the spermatic cord when fluid production by the tunica vaginalis is increased or fluid reabsorption is impaired. A congenital hydrocele, caused by communication between the tunical and peritoneal cavities via a patent processus vaginalis (PPV), usually improves spontaneously within the first year of life [12]. The standard approach to treatment is inguinal; it involves freeing the spermatic cord from attached tissue, separating the tissues, and high-ligating the PPV [34]. Recently, good success rates with minimal complications were reported when hydrocelectomy was performed via a scrotal approach [2]. Other studies also demonstrated that the scrotal approach is an alternative for the correction of inguinoscrotal pathologies [5]. The advantages of this approach include minimal postoperative scarring because the incision is small, a short operative time, and elimination of any risk of ilioinguinal nerve damage because the spermatic cord is not dissected [2]. However, the postoperative risk of persistent hernia or hydrocele when PPV high-ligation is inadequate remains of concern. Testicular ascent may also develop postoperatively when the proximal attachments are not adequately separated [67].
To date, no report has compared outcomes of surgery using the traditional inguinal and scrotal approaches in randomized patients; we address this issue here. To our knowledge, this study is the first randomized clinical trial to analyze the outcomes of the two hydrocelectomy methods in boys.
Institutional Review Board of Chonnam National University (approval number: CNUH-2017-254) approval was obtained and all procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its comparable ethical standards. Informed consent was obtained f rom all individual participants included in the study.
In total, 347 boys aged 0–12 years with hydroceles confirmed by ultrasonography were enrolled in this prospective study from May 2011 to December 2016. All parents gave written informed consent. Before operation, we recorded scrotal anomalies, testicular volumes, and cryptorchidism revealed by scrotal ultrasonography. We performed physical examination and transillumination test to exclude inguinal hernia, and boys with suspected testicular tumors, as indicated clinically or ultrasonographically, and boys with prior operative histories (ipsilateral scrotal or inguinal surgery), primary or secondary hypogonadism, and/or hormonal abnormalities were excluded (n=2). We divided the boys into two groups in a 1:1 ratio through a simple randomization procedure: group I (n=173; scrotal incision hydrocelectomy) and group II (n=172; conventional inguinal hydrocelectomy). Boys who developed fever prior to operation, and those whose parents withdrew consent or could not be contacted before operation were dropped out (group I/group II=7/10). Ten and six boys in both groups, respectively, were lost to follow-up after surgery (Fig. 1). Finally, 156 boys who underwent scrotal incision hydrocelectomy (group I) and 156 boys who underwent hydrocelectomy via the traditional inguinal incision approach (group II) were included in data analysis.
We recorded the postoperative rates of wound infection, epididymitis, reduced testicular volume, hydrocele relapse, wound dehiscence, and scrotal hematoma. All boys underwent follow-up physical examinations at postoperative 1 week and routine scrotal ultrasonography (until maximum 3 months) to assess the status of operation-related complications and the recurrence of hydrocele. All boys were admitted one day before the operation to prepare the surgery. The hospitalization day was defined as 1 day before the operation day to discharge from the hospital. If postoperative complications were occurred, discharge from the hospital was postponed. Surgical success was defined as the absence of any postoperative complication and no need for surgical conversion.
All operations were performed by one surgeon who is experienced to pediatric urological surgery (Professor Sun-Ouck Kim) and all patients were under general anesthesia. The operation time was defined as that from the beginning to end of anesthesia. We encountered no intraoperative complication.
After induction of general anesthesia, a transverse skin incision was created along a high scrotal skin fold. The skin, dartos fascia, and thin cremasteric fascia were incised as usual. The surgeon approached the testis via blunt and sharp dissection of subcutaneous tissues. The scrotal wound was retracted upward to facilitate dissection, and the cord cover and adhesive tissues were dissected at the most cephalad site possible to ensure sufficient cord length and to possibly allow entry into the lower half of the inguinal canal from below. The gubernacular attachments were released to enable identification of the testes (within the cremasteric fibers), the PPV, and the cord structures. The fibers and hernia sac were carefully separated from the cord, and the cranial sac was mobilized under traction into the canal and ligated with sutures, as in traditional inguinal incision hydrocelectomy. The testis was then relocated into the dartos pouch, and two (medial and lateral) fixation sutures were placed between the testicular tunica albuginea and inner scrotal wall to prevent testicular ascent. Subcutaneous tissue was sutured using Vicryl 3/0 and the skin was sutured subcuticularly with 4/0 polypropylene, without drain insertion [12345].
The first step of inguinal incision hydrocelectomy was creation of a skin-crease inguinal incision over the external inguinal ring. Dissection proceeded down to the external ring and the external oblique aponeurosis. The external ring was opened by splitting the aponeurosis. The ilioinguinal nerve lying under the aponeurosis was preserved to minimize the risk of postoperative numbness and pain. The spermatic cord was mobilized and dislocated laterally and upwardly. The cord and testis were gently removed through the inguinal incision and then dissected to an extent permitting mobilization. After re-insertion of the testis via the incision site, the hydrocele sac was opened and irrigation was performed to avoid wound contamination by hydrocele fluid. After examining the testis and other structures for tumors and other lesions, PPV high-ligation was performed and the testis was repositioned in the hemiscrotum. The inguinal wound was closed; the external oblique aponeurosis and subcutaneous tissue layers were sutured with Vicryl 3/0, and the skin was closed with subcuticular 4/0 polypropylene sutures; no drainage tube was placed [12345].
Statistical analysis was performed using IBM SPSS Statistics ver. 24.0 software (IBM Co., Armonk, NY, USA). Categorical data were compared using Fisher's exact test and Chi-square test and continuous data were compared using independent t-test and Mann-Whitney U-test. A p-value of <0.05 was considered to reflect statistical significance.
Patient age did not differ between groups (p=0.130). Unilateral hydroceles predominated in both groups and there was no significant difference between groups (p=0.305). Table 1 shows the baseline characteristics and type of hydrocele of all patients. We divided hydroceles into three types: group I included 127 cases (81.4%) of communicating hydroceles, 21 cases (13.5%) of non-communicating hydroceles, and 8 cases (5.1%) of hydrocele of cord, and group II included 117 cases (75.0%) of communicating, 25 cases (16.0%) of non-communicating hydroceles, and 14 cases (9.0%) of hydrocele of cord (Table 1).
The overall success rates of the two groups were similar (group I, 96.8%; group II, 89.1%; p=0.740). The operative time (mean±standard deviation [SD]) was 30.94±3.95 minutes in group I and 38.02±7.12 minutes in group II. The hospital stay was 3.94±0.30 days (mean±SD) in group I and 4.24±0.99 days in group II (Table 2). The operation time and hospital stay were significantly shorter in group I than in group II (p<0.001 and p=0.009, respectively).
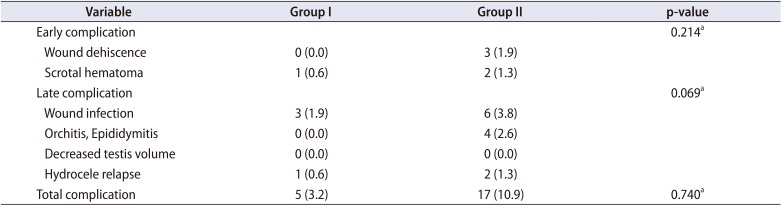
In terms of early postoperative complications (within 1 week), three cases (1.9%) wound dehiscence were found in groups II. Scrotal hematoma was developed in one cases (0.6%) and two cases (1.3%) in group I and group II. In terms of late complications (within 3 months postoperatively), three cases (1.9%) and six cases (3.8%) of wound infection, and one cases (0.6%) and two cases (1.3%) hydrocele relapses were recorded in group I and group II, respectively. Four cases (2.6%) of epididymitis were found in group II. There was no case of postoperative testicular atrophy. The overall postoperative complication rate showed no significant difference between the two groups (3.2% vs. 10.9%, p=0.740; Table 3).
We found that scrotal incision hydrocelectomy to treat isolated hydroceles in boys was well tolerated, and was associated with a shorter operation time and hospital stay than was the traditional approach. Also, the success rate of the scrotal approach was 96.8%, with only five (3.2%) instances of postoperative complications. The results thus suggest that scrotal incision hydrocelectomy may be safely substituted for traditional inguinal hydrocelectomy.
PPVs are classified as closed, partially closed, or open, depending on the extent of communication or obliteration from the internal ring to the testis. The primary goal of surgical hydrocele treatment is to ligate the PPV as cranially as possible without iatrogenic injury or any postoperative complication. Two principal surgical concerns have been raised: does PPV dissection from the spermatic cord improve as surgical skill increases, and how can dissection be rendered adequately proximal? Scrotal incision usually does not permit adequate PPV separation and ligation, associated with the risk of postoperative hernia or hydrocele relapse. The traditional inguinal incision allows easy access to the PPV, and high-ligation. Thus, inguinal incision hydrocelectomy has previously been accepted as the gold standard treatment [28].
In boys, the scrotal skin can be readily mobilized via surgical incision, and the distance from the external to the internal inguinal ring is relatively short, aiding scrotoinguinal surgery. Thus, some surgeons believe that scrotal incision hydrocelectomy would allow adequate high-ligation of the PPV. Here, we successfully dissected the PPV from cord structures through the inguinal canal by applying traction to the scrotal incision. After the PPV was separated from the spermatic cord, the proximal PPV could always be retracted to the level of the internal inguinal ring and ligated at the most proximal level.
The advantages of the scrotal approach are as follows. The approach is easy, given the anatomical structures involved in scrotal and groin pathology in boys. Wound edge traction is seldom required, reducing trauma to the inguinal region; dissection is minimal, associated with little postoperative pain or swelling. The conventional incision for hydrocele repair in the groin usually leaves a scar. Nonetheless, this remains easily visible and few cases, the scar, especially if placed close to the pubic tubercle, tends to become hypertrophic. The single incision in the scrotal skin fold is associated with less pain than is the customary inguinal skin-crease incision, improves cosmetic outcomes, and is associated with a shorter operative time because only one, not two, incisions must be closed.
Several studies have obtained successful results with use of the scrotal approach in boys with hernias and hydroceles [29]. Alp et al. [2] reported that the clinical outcomes of the inguinal and scrotal approaches were comparable in the treatment of communicating hydroceles in boys using sacdissection without opening.
Koyle et al. [10] emphasized the benefits of the scrotal approach: easy access to scrotal structures and removal of the distal tunica vaginalis without significant morbidity, and excellent cosmetic outcomes. Others have suggested that the inspection of scrotal structures would reduce the risk of subsequent non-communicating hydrocele, eliminate the risk of acute scrotal hematoma, and permit the excision of vestigial appendages [71112]. Furthermore, several reports have shown that the scrotal approach to orchiopexy for correction of cryptorchidism in boys is also simple and effective [13141516].
Our study has several limitations. First, selection bias in terms of communicating and non-communicating hydroceles may have been in play, although we randomized the operation method regardless of preoperative ultrasonographic findings in terms of the PPV or hydrocele type. Second, our subject numbers were small and the work was performed in a single tertiary-care center. Because of the mean follow-up period was relatively short, the real hydrocele relapse incidence would probably underestimated. A prospective trial with a large cohort and long-term follow-up is needed.
Notes
CONFLICTS OF INTEREST: The corresponding author of this manuscript, Sun-Ouck Kim, declares relationship with the Chonnam National University Hospital Institutional Research Fund (no. CNUH-2017-254), but this has made no influence on this work in relation with the company or its products. Other authors have no potential conflicts of interest to disclose.
References
1. Lasheen A. Hydrocelectomy through the inguinal approach versus scrotal approach for idiopathic hydrocele in adults. J Arab Soc Med Res. 2012; 7:68–72.
2. Alp BF, Irkilata HC, Kibar Y, Zorba U, Sancaktutar AA, Kaya E, et al. Comparison of the inguinal and scrotal approaches for the treatment of communicating hydrocele in children. Kaohsiung J Med Sci. 2014; 30:200–205. PMID: 24656161.

3. Bevan AD. Operation for undescended testicle and congenital inguinal hernia. J Am Med Assoc. 1899; 13:773–777.

4. Hutcheson JC, Cooper CS, Snyder HM 3rd. The anatomical approach to inguinal orchiopexy. J Urol. 2000; 164:1702–1704. PMID: 11025753.

5. Soualili Z, Achouri D, Haif A, Touabti S, Yahia SA, Benmahmoud M, et al. The interscrotal approach to inguinoscrotal pathologies. Arab J Urol. 2015; 13:176–178. PMID: 26413342.

6. Dayanc M, Kibar Y, Irkilata HC, Demir E, Tahmaz L, Peker AF. Long-term outcome of scrotal incision orchiopexy for undescended testis. Urology. 2007; 70:786–788. discussion 788-9. PMID: 17991558.

7. Bassel YS, Scherz HC, Kirsch AJ. Scrotal incision orchiopexy for undescended testes with or without a patent processus vaginalis. J Urol. 2007; 177:1516–1518. PMID: 17382769.

8. Wilson JM, Aaronson DS, Schrader R, Baskin LS. Hydrocele in the pediatric patient: inguinal or scrotal approach? J Urol. 2008; 180(4 Suppl):1724–1727. discussion 1727-8. PMID: 18721980.

9. Bianchi A, Squire BR. Transscrotal orchidopexy: orchidopexy revised. Pediatric Surg Int. 1989; 4:189–192.

10. Koyle MA, Walsh R, Caruso A, Wilson E. Scrotal (Bianchi) approach to patent processus vaginalis in children. Tech Urol. 1999; 5:95–99. PMID: 10458663.
11. Fearne Ch, Abela M, Aquilina D. Scrotal approach for inguinal hernia and hydrocele repair in boys. Eur J Pediatr Surg. 2002; 12:116–117. PMID: 12015656.

12. Feng S, Yang H, Li X, Yang J, Zhang J, Wang A, et al. Single scrotal incision orchiopexy versus the inguinal approach in children with palpable undescended testis: a systematic review and meta-analysis. Pediatr Surg Int. 2016; 32:989–985. PMID: 27510940.

13. Iyer KR, Kumar V, Huddart SN, Bianchi A. The scrotal approach. Pediatr Surg Int. 1995; 10:58–60.

14. Caruso AP, Walsh RA, Wolach JW, Koyle MA. Single scrotal incision orchiopexy for the palpable undescended testicle. J Urol. 2000; 164:156–158. discussion 158-9. PMID: 10840452.

15. Gökçora IH, Yagmurlu A. A longitudinal follow-up using the high trans-scrotal approach for inguinal and scrotal abnormalities in boys. Hernia. 2003; 7:181–184. PMID: 12802619.

16. Parsons JK, Ferrer F, Docimo SG. The low scrotal approach to the ectopic or ascended testicle: prevalence of a patent processus vaginalis. J Urol. 2003; 169:1832–1833. discussion 1833. PMID: 12686856.

Table 1
Comparison of baseline characteristics and hydrocele type of two groups
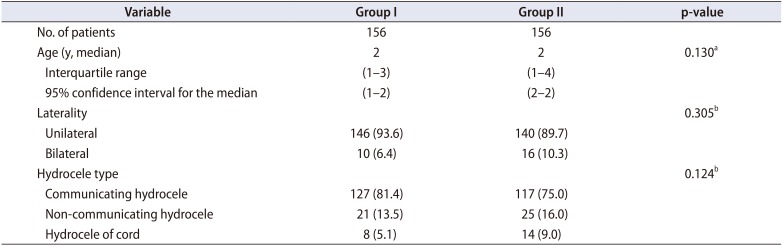
Table 2
Comparison of surgical outcomes between the two groups
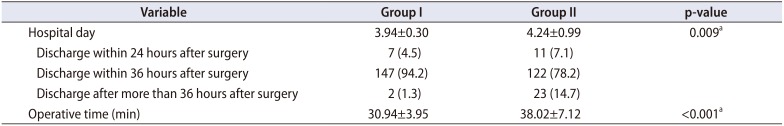
Table 3
Comparison of postoperative complications between the two groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download