Abstract
Purpose
To compare patients with sepsis due to obstructive urolithiasis (Sep-OU) and underwent drainage by percutaneous nephrostomy (PCN) or a double-J (DJ)-ureteral stent and to identify predictive risk factors of DJ stent failure in these patients.
Materials and Methods
We reviewed our records from January 2013 to July 2018 and identified 286 adult patients with Sep-OU out of which 36 had bilateral involvement, thus total 322 renal units were studied. Urologic residents in training carried out both ureteral stenting and PCN tube placement. Demographic data and stone characteristics were recorded along with Charlson comorbidity index. For predicting risk factors of DJ stent failure, those variables that had a p-value <0.1 in univariate analysis were combined in a multinomial regression analysis model.
Results
The patients with PCN placement were significantly older than those with DJ stent placement (p=0.001) and also had significant number of units with multiple calculi (p=0.018). PCN was also placed more frequently in those patients with a upper ureteric calculi (p<0.05). On multinomial regression analysis multiple calculi (p=0.014; odds ratio [OR], 4.878; 95% confidence interval [CI], 1.377–17.276) and larger calculi size (p=0.040; OR, 0.974; 95% CI, 0.950–0.999) were the significant predictors of DJ stent failure.
Urgent decompression of the urinary collecting system is required in patients with obstructive urolithiasis in two main scenarios: in presence of urinary tract infections and when patient is in anuria. There are two popular methods for doing this, which are either placing a double-J (DJ) ureteral stent or a percutaneous nephrostomy (PCN) tube [1]. It is still a matter of debate that, which out of the two is superior in draining an infected system. Does one method has more complications or is there a difference in success rates between the two are all questions that do not have a definitive answer [23]. The choice of method to drain an obstructed infected system thus usually depends upon the urologist's personal preference, institutional practice, familiarity with procedure and person doing the procedure (junior/senior resident, radiologist or urologist himself). It has been our experience that in certain cases of sepsis due to obstructive urolithiasis (Sep-OU) despite the placement of a DJ stent, there is inadequate system drainage and persistent features of sepsis and a PCN has to be placed. We thus conducted this study to study the pattern of drainage of collecting system in patients with Sep-OU and to study predictive risk factors of DJ stent failure in such cases. The persistence of sepsis due to inadequate system drainage was considered as failure of a DJ stent.
We retrospectively reviewed our prospectively maintained database for adult patients (>18 years age) with Sep-OU who underwent either DJ stent placement or PCN placement from January 2013 to July 2018. The Institutional Ethical Committee approved the study protocol (approval number: 3204/Ethics/R-cell-18). Informed consent was taken from the patient.
The definition of sepsis was based on the third international consensus definitions for sepsis. This defines sepsis as a ‘life-threatening dysfunction of organs caused by a dysregulated response of the host to infection’. The parameters used to assess organ dysfunction include Glasgow coma scale, total leucocyte counts, platelet counts, serum creatinine and bilirubin [4]. These parameters were recorded within 24 hours of admission.
Urology senior residents in training usually place both DJ stent and PCN at our institute; only in rare cases do the consultants carry out these procedures. We thus included only those cases that were performed by urology residents. As both procedures are regularly done at our department familiarity with procedures is not an issue. Although urology residents carry out the procedure, the choice of procedure is the discretion of the consultant urologist in charge. If it is decided to place a DJ stent and attempts to place it fail, then PCN is placed. In patients who cannot be placed in a lithotomy position PCN is placed. Also in patients in whom there are persistent signs of sepsis and the system is not drained despite placement of a DJ stent, a PCN is placed.
A DJ stent is placed under local anesthesia with a 20F sheath and 30 degree telescope. The patient is laid in lithotomy position. We place a 5F or 6F DJ stent. A 0.035-inch guide-wire is first introduced into the collecting system and then the DJ stent is introduced over it. This is done under fluoroscopic guidance. We routinely place a Foley catheter in these patients.
PCN is also placed under local anesthesia with the patient in prone position. The puncture is done using Accuson X-300 (SIEMENS Healthineers, Erlangen, Germany) ultrasound scanner and a guide-wire is introduced into the collecting system. A 12F or 14F PCN is then placed over the guide-wire under fluoroscopic guidance. Contrast is instilled into the system via PCN to confirm its position if there is any uncertainty regarding it.
We recorded the patient age, sex, stone location, size, laterality and Charlson comorbidity index (CCI). We also identified 20 patients in whom a PCN had to be placed after failure of DJ stent.
The continuous data was presented as median and interquartile range and categorical data with percentage. Chi-square test was used for categorical data and independent sample t-test for continuous data. For the purpose of analyzing risk factors for DJ stent failure we combined those variables with p-value <0.1 in a multinomial risk adjusted regression analysis to identify significant variables. All statistical analysis was done using IBM SPSS Statistics ver. 21.0 software (IBM Co., Armonk, NY, USA).
A total of 286 patients were included in the study and 36 patients (12.6%) had bilateral involvement. The total renal units studied were thus 322. The patient and stone characteristics are described in Table 1. The most common stone location was upper ureteric (36.0%). When compared to patients with DJ stent placement the patients with a PCN were older (p=0.001) and had a greater stone size (p=0.018). PCN was placed more often in patients with a upper ureteric calculi. Both groups of patients were comparable in terms of sex, multiple calculi, CCI and lower ureteric stone location (Table 2).
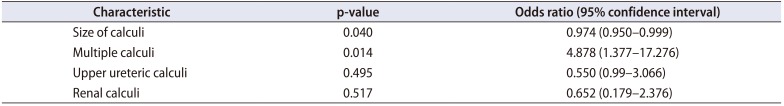
Out of the 144 patients who had a DJ stent placed for Sep-OU, 20 had failure i.e., a PCN had to be placed due to non-resolution of sepsis and persistent obstruction. On univariate analysis it was found that in patients with DJ stent failure the stones were larger (p=0.015) in size and multiple (p=0.002). These were the only two significant factors. DJ stent failure was more in patients with a renal calculus (20%) with an odds ratio (OR) and 95% confidence interval (CI) of 2.375 and 0.905–6.233 respectively, but it was not statistically significant (p=0.073). On combining factors in a multinomial regression model the two significant factors for DJ stent failure were size of calculi (p=0.040; OR, 0.974; 95% CI, 0.950–0.999) and multiple calculi (p=0.014; OR, 4.878; 95% CI, 1.377–17.276). Table 3 and 4 summarize the results of univariate analysis and multinomial regression analysis respectively.
Decompression of urinary tract in presence of Sep-OU is an emergency procedure. Usually it has to be done with a DJ stent or PCN placement before any definitive management for relief of obstruction can be carried out. The choice of procedure among the two usually has to be individualized in absence of any clear guidelines demonstrating the superiority of one procedure over the other [567].
While DJ stenting is usually done by a urologist, PCN placement may be done by a urologist or an intervention radiologist [8]. In King George's Medical University urologists do both procedures. Usually in teaching institutes these procedures are done by urologic residents. In our study also we included only those patients who had the DJ stent or PCN placed by residents.
There are few studies comparing DJ stent with PCN placement in the setting of Sep-OU. Most of these studies are observational and retrospective [91011]. The two prospective studies comparing DJ stent with PCN have conflicting results. While one study demonstrated clear superiority of PCN, the other could not demonstrate the benefits of one procedure over the other [312].
The choice of procedure thus remains at the clinician's discretion. The perceived advantage of DJ stenting is its lesser rate of infection, better patient comfort and its shorter procedural time. The disadvantages of DJ stent placement include more dysuria, hematuria, urgency, analgesic requirement and delay in definitive management. Also usually it has to be placed without anesthesia, which may be discomforting for the patient [101213].
On the other hand PCN placement presumably provides better drainage and may be suitable for patients in whom eventual percutaneous management of the calculi is contemplated, but has poorer patient acceptance, requires more care (dressings) and has longer hospital stay [3910].
We feel that there is no doubt that PCN provides better drainage of an infected system. The question remains that whether it is superior to DJ stent in Sep-OU? We found that 20 out of 144 patients (13.9%) who had a DJ stent placed initially had failure, and a PCN had to be placed. To identify the subset of patients that could benefit from PCN insertion straightaway we carried statistical analysis of factors associated with DJ stent failure and found that PCN would be a suitable initial procedure of choice in patients with multiple stones and larger stones. Although renal stones were not significant predictor of DJ stent failure we feel that a PCN would be better if percutaneous management of the calculi is planned. Obviously, in patients with a bleeding disorder a DJ stent placement would be apt.
The greatest limitation of our study is its retrospective nature. Also there is heterogeneity in patient selection as individual preferences of a urologist play a role in selection of method to drain the obstructed system. On comparing patients with PCN and DJ stent there was clearly a trend in our patients for PCN to be placed in those with greater stone size and older age. Thirdly, the data of this study may not apply to the western population as the patients present late to us and usually have frank pyonephrosis with thick pus in the collecting system that may contribute to DJ stent failure.
The strength of our study lies in its simplicity and the fact that both procedures were carried out by a same cohort (urologic residents). We focused our analysis on three major stone characteristics viz. number, location and size.
To conclude our study demonstrates that in patients with Sep-OU if there are multiple calculi and larger stones then probably PCN placement rather than a DJ stent is a better alternative. Obviously, a prospective randomized study with better power would be required to substantiate our results.
References
1. Türk C, Knoll T, Seitz C, Skolarikos A, Chapple C, McClinton S, et al. Medical expulsive therapy for ureterolithiasis: the EAU recommendations in 2016. Eur Urol. 2017; 71:504–507. PMID: 27506951.

2. Ramsey S, Robertson A, Ablett MJ, Meddings RN, Hollins GW, Little B. Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol. 2010; 24:185–189. PMID: 20063999.

3. Pearle MS, Pierce HL, Miller GL, Summa JA, Mutz JM, Petty BA, et al. Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol. 1998; 160:1260–1264. PMID: 9751331.

4. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for Sepsis and Septic shock (Sepsis-3). JAMA. 2016; 315:801–810. PMID: 26903338.

5. Chang HC, Tang SH, Chuang FP, Wu ST, Sun GH, Yu DS, et al. Comparison between the use of percutaneous nephrostomy and internal ureteral stenting in the management of long-term ureteral obstructions. Urol Sci. 2012; 23:82–84.

6. Hsu L, Li H, Pucheril D, Hansen M, Littleton R, Peabody J, et al. Use of percutaneous nephrostomy and ureteral stenting in management of ureteral obstruction. World J Nephrol. 2016; 5:172–181. PMID: 26981442.

7. Ku JH, Lee SW, Jeon HG, Kim HH, Oh SJ. Percutaneous nephrostomy versus indwelling ureteral stents in the management of extrinsic ureteral obstruction in advanced malignancies: are there differences? Urology. 2004; 64:895–899. PMID: 15533473.

8. Lynch MF, Anson KM, Patel U. Current opinion amongst radiologists and urologists in the UK on percutaneous nephrostomy and ureteric stent insertion for acute renal unobstruction: results of a postal survey. BJU Int. 2006; 98:1143–1144. PMID: 17125470.

9. Ahmad I, Saeed Pansota M, Tariq M, Shahzad Saleem M, Ali Tabassum S, Hussain A. Comparison between Double J (DJ) ureteral stenting and Percutaneous Nephrostomy (PCN) in obstructive uropathy. Pak J Med Sci. 2013; 29:725–729. PMID: 24353616.

10. Goldsmith ZG, Oredein-McCoy O, Gerber L, Bañez LL, Sopko DR, Miller MJ, et al. Emergent ureteric stent vs percutaneous nephrostomy for obstructive urolithiasis with sepsis: patterns of use and outcomes from a 15-year experience. BJU Int. 2013; 112:E122–E128. PMID: 23795789.

11. Yoshimura K, Utsunomiya N, Ichioka K, Ueda N, Matsui Y, Terai A. Emergency drainage for urosepsis associated with upper urinary tract calculi. J Urol. 2005; 173:458–462. PMID: 15643207.

12. Mokhmalji H, Braun PM, Martinez Portillo FJ, Siegsmund M, Alken P, Köhrmann KU. Percutaneous nephrostomy versus ureteral stents for diversion of hydronephrosis caused by stones: a prospective, randomized clinical trial. J Urol. 2001; 165:1088–1092. PMID: 11257644.

13. Joshi HB, Adams S, Obadeyi OO, Rao PN. Nephrostomy tube or 'JJ' ureteric stent in ureteric obstruction: assessment of patient perspectives using quality-of-life survey and utility analysis. Eur Urol. 2001; 39:695–701. PMID: 11464060.
Table 1
Characteristics of patients in the study
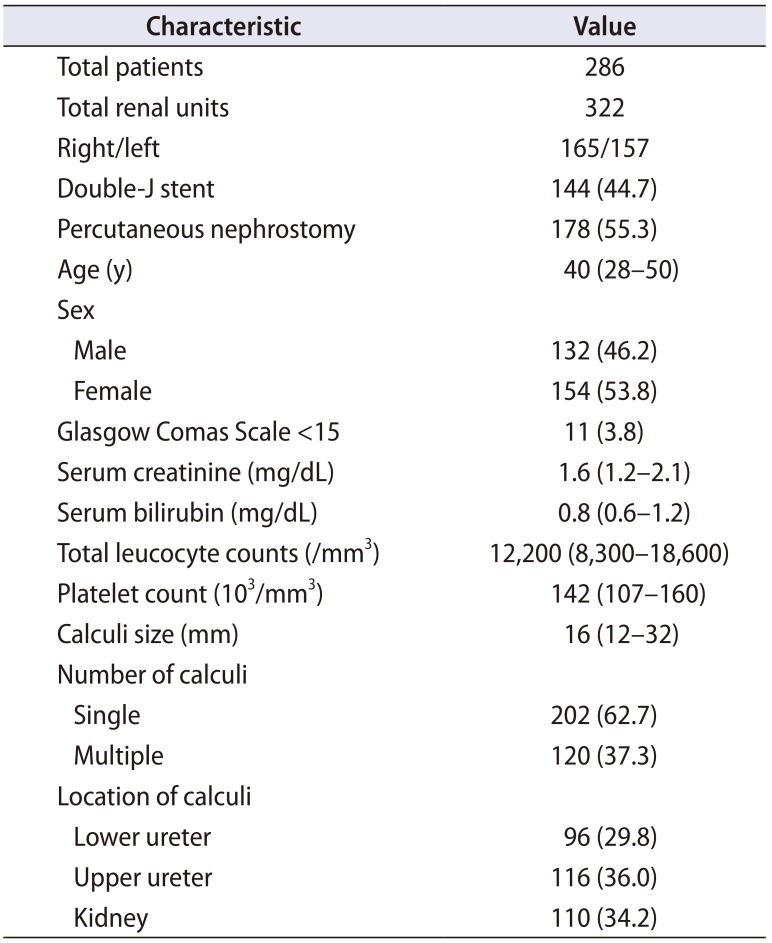
Table 2
Comparison of patients with DJ stent versus PCN
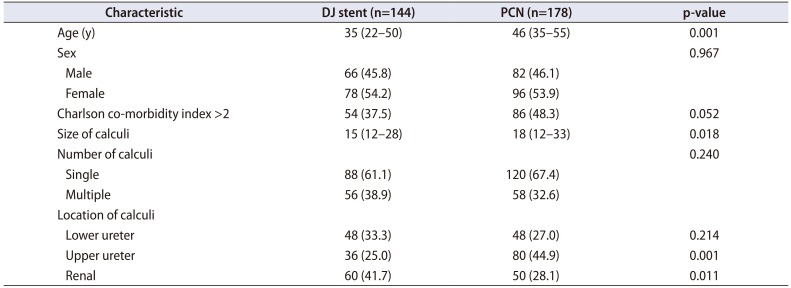
Table 3
Univariate analysis of factors for DJ stent failure
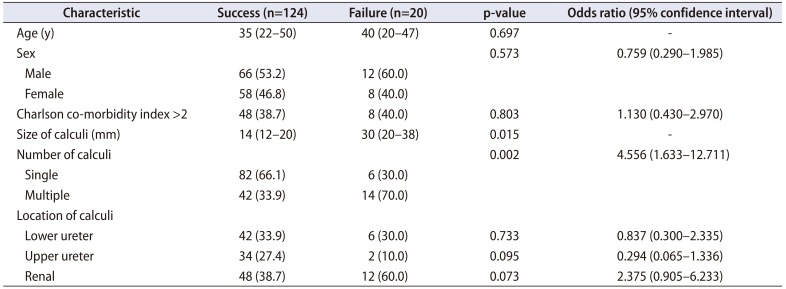
Table 4
Multinomial regression analysis of risk factors for DJ stent failure




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download