Case Report
A 45-year-old woman diagnosed with end-stage heart failure and cardiac cirrhosis was referred for CHLT. She was 158 cm tall and weighed 45.6 kg, and she had valvular heart disease with a functional status of class IV based on the New York Heart Association criteria. Initially, no substantial hepatic dysfunction was apparent but she did exhibit signs of mild jaundice. She had undergone mitral valve replacement and tricuspid annuloplasty, 1 month before being transferred to our hospital. Ischemic kidney injury was suspected on postoperative day (POD) 1, requiring continuous renal replacement therapy (CRRT). Two days later, the patient suffered cardiac arrest caused by ventricular fibrillation, and venoarterial extracorporeal membrane oxygenation (ECMO) was applied to the right femoral vessels.
After admission to our institution, transthoracic echocardiogram demonstrated severe biventricular dysfunction with a left ventricular ejection fraction of less than 5%. As the patient was waitlisted for CHLT, the peripheral ECMO was converted to a central ECMO with direct cannulation into the ascending aorta and right atrium. The ECMO flow rate ranged from 3.6–4.1 L/min, and heparinization was conducted to maintain activating clotting time (ACT) within 160–180 s. The patient remained on CRRT, and infusion of norepinephrine (0.03 µg/kg/min) was set to obtain a mean arterial pressure ranging from 50–60 mmHg. Progressive hyperbilirubinemia developed, and abdominal computed tomographic images revealed hepatic fissure widening, irregularity of hepatic contours, and heterogeneous enhancement of parenchyma, which were all considered features suggestive of chronic liver disease. In addition to those findings, splenomegaly, a moderate amount of ascites, and dilated inferior vena cava indicated congestive hepatopathy secondary to heart failure. A tracheostomy was performed to facilitate long-term ventilator care, and the patient was sedated with remifentanil (0.03 µg/kg/min). Electrocardiography revealed the onset of new atrial fibrillation with a ventricular response of 76 bpm. Plain chest X-ray revealed cardiomegaly with total atelectasis of the left lung, and bronchoscopic examination revealed compression of the left main bronchus by the enlarged left atrium. Preoperative blood test results were as follows: total bilirubin 47.3 mg/dl, direct bilirubin 36.2 mg/dl, aspartate transaminase 92 units/L, alanine transaminase 51 units/L, creatinine 0.91 mg/dl, platelet count 34,000 /µl, and prothrombin time international normalized ratio (PT INR) 1.49. Child-Pugh class C and a model for end-stage liver disease score of 26 were established, and an emergent CHLT was scheduled.
General anesthesia was induced with midazolam (2 mg), etomidate (8 mg), and atracurium (50 mg), and maintained with oxygen, room air, and desflurane. Mechanical ventilation was set to pressure controlled mode with a peak airway pressure of 20 cmH2O, targeting normocarbia. Hemodynamic monitoring was comprised of intra-arterial (both right radial and femoral artery), central venous, inferior vena cava (femoral vein), and pulmonary arterial pressures with cardiac output measurements (Vigilance™ monitoring, Edwards Lifesciences, Irvine, CA, USA) using a Swan-Ganz catheter (CCombo V; 7.5 French, Edwards Lifesciences, Irvine, CA, USA). Because the right inguinal area had been anatomically disturbed during prior ECMO insertion, the right femoral vessels were each punctured with an arterial catheter (Leader Cath©, 20 G 0.5 × 80 mm, Vygon©, Ecouen, France) under the guidance of ultrasound imaging. Leaving aside the previously inserted 7 Fr central line in the right internal jugular vein, a 9-Fr Advanced Venous Access catheter (Edwards Lifesciences, Irvine, CA, USA) was also placed approximately 5 cm distal to the original insertion point under ultrasonographic guidance. After unremarkable induction, a transesophageal echocardiography probe was inserted to assess function and confirm de-airing of the heart graft at the end of the cardiopulmonary bypass (CPB).
A sequential heart and liver transplant was planned without interrupting extracorporeal circulatory support. The heart and liver graft were both immersed in histidine-tryptophan-ketoglutarate solution and maintained at approximately 0℃. After re-sternotomy, the left femoral vessels and superior vena cava were cannulated and CPB was established by the administration of 100 mg heparin. Heart transplantation was performed using a modified bicaval technique, and at the end of anastomosis a temporary pacemaker was inserted to maintain the heart rate at 90 bpm (
Table 1). During the total bypass time of 148 min, 11 units of leukocyte-depleted red blood cells (LDRBC) and 2 units of fresh frozen plasma (FFP) were transfused. CPB was rapidly converted to peripheral ECMO via the left femoral vessels. Protamine sulfate (100 mg) was used to reverse heparinization and achieve an ACT of 163 s.
With the chest left open, liver transplantation was initiated. A separate incision below the subcostal area was made and full mobilization of the recipient's liver was achieved by performing careful dissection. During hepatectomy, substantial hemorrhage was observed from not only the surgical field in progress but also the thorax, which necessitated massive volume resuscitation using a rapid infusion system (Level 1, Smiths Medical Products, MN, USA). The cardiac surgeon was called upon for additional bleeding control. The piggyback technique was applied during the anhepatic stage.
While referring to the hourly results of complete blood cell counts and coagulation profiles, transfusion was conducted as follows: LDRBC targeting hemoglobin of 10 g/dl, two units of FFP when PT INR was above 3, and one unit of single-donor platelets when the platelet count was below 50,000 /µl. A potassium level exceeding 4.5 mEq/L during the anhepatic stage was managed by using a bolus dose of 10 international units (IU) of regular insulin, followed by 200 ml of 5% dextrose solution infusion. Correction of metabolic acidosis with a base deficit below −10 mmol/L was attempted via the infusion of 1 L of half saline mixed with 80 mEq/L sodium bicarbonate, and 300 mg calcium chloride was administered when ionized calcium was less than 0.8 mmol/L. After reperfusion, glucose control was performed using regular insulin in accordance with the Portland protocol, targeting 80–120 mg/dl. Perioperative coagulation and arterial blood gas profiles are shown in
Tables 2 and
3, respectively. Furthermore, thromboelastography was utilized (
Table 4), as platelet count alone does not accurately correlate with actual coagulation function in patients with ECMO [
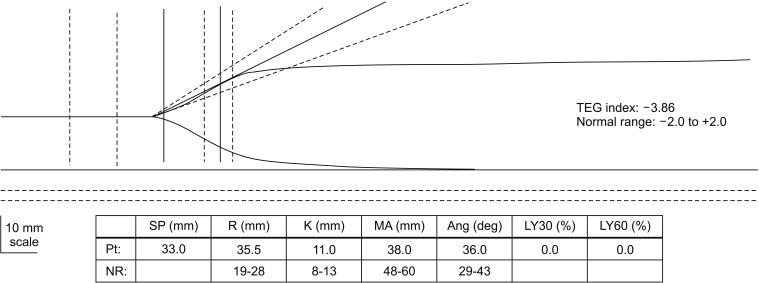
4]. Perioperative thromboelastography analyses resulted in flat traces for all, except the protamine-added blood sample, which showed mostly normal curve characteristics, slightly decreased maximum amplitude and slightly increased R time (
Fig. 1). This indicated that the effect of heparin was the dominant cause of the coagulation disorder. Despite pre-administration of 1 mg atropine, 600 mg calcium chloride, and 20 mEq bicarbonate, post-reperfusion syndrome lasting approximately 3 min developed (
Table 1) and small doses of epinephrine (total of 100 µg) were required for recovery. Tranexamic acid (500 mg) was administered 10 min after reperfusion, and an additional bolus of protamine (50 mg) was given due to the prolonged ACT (215 s). After completing the closure of the abdominal incision, the cardiac transplant team returned to control residual bleeding and close the sternum.
Overall, 13,600 ml crystalloid, 1,250 ml 5% albumin, 3,800 ml of half saline, 32 units of LDRBC, 5,500 ml of cell saver (Haemonetics, MA, USA) blood, 11 units of FFP, 4 units of single-donor platelets, and 5 units of cryoprecipitate were infused. There was no measurable urine output, and lost red cell mass was calculated to be approximately 7,500 ml [
5]. Removal of body waste through substantial surgical bleeding and replacement by fluids and blood products mimicked the effects of plasmapheresis [
6], which led to a decline in postoperative creatinine level (0.7 mg/dl) without implementing intraoperative renal replacement therapy. Upon completion of surgery, dobutamine (5 µg/kg/min), norepinephrine (0.05 µg/kg/min), vasopressin (0.05 units/min), and epinephrine (0.05 µg/kg/min) were administered and the patient was transferred to the cardiothoracic intensive care unit on ECMO support. The total anesthesia time was 13 h and 15 min.
On POD 1, the patient exhibited ischemic signs in the right hand which appeared to be associated with prolonged arterial cannulation, and these were alleviated after an emergent thromboembolectomy of the right radial and brachial artery. Because the arterial line had been inserted prior to arrival at our institution, whether the Allen's test had been performed was uncertain. Moreover, a significant dose of vasopressor may have impeded perfusion of the right hand contributing to the ischemic event. ECMO was removed on POD 4, but norepinephrine (0.1 µg/kg/min) infusion was needed, and it was slowly tapered over the course of 1 month postoperatively. Transaminase levels, prothrombin time, and bilirubin levels were normalized within 3 weeks. However, the patient's recovery was hindered by type II respiratory failure requiring mechanical ventilation for over 1 month, and oliguric acute kidney injury necessitating CRRT. Improving renal function was evident, and the transition from CRRT to hemodialysis (3 times a week) took place on POD 45, at which point hemodialysis was no longer needed. In addition, the patient exhibited defective wound healing at multiple locations on the sternum, abdomen, and left inguinal area, which were treated using antibiotics and surgical revision. Two months after CHLT, transudative ascites and right pleural effusion developed transiently, but improved after daily drainage. To investigate the underlying cause, abdominal computed tomography was undertaken and revealed signs of chronic liver disease and mild periportal edema implying volume overload status. The patient survived a recent episode of septic shock due to catheterrelated infection. The most recent echocardiogram revealed normal left ventricular function and slightly reduced right ventricular systolic function with a small amount of pericardial effusion. At 5 months postoperatively, she was discharged in a stable condition without evidence of rejection of either allograft.
Discussion
Since its introduction in 1984 by Starzl et al. [
7], the number of CHLTs performed has accumulated to over 200 in the United States, the majority of which were performed within the last decade [
8]. Despite limited global experience, medical and surgical advances have improved the outcome of CHLT, which is becoming a promising therapy for those who suffer dual organ failure. A single-center study of 26 CHLT recipients demonstrated acceptable results, with 1 year and 5-year survival rates of 87% and 83%, respectively [
3]. According to the medical literature, the most common indications for CHLT are familial amyloidosis and heart failure with concomitant cardiac cirrhosis [
910].
As the majority of CHLT candidates with severe cardiac insufficiency are unable to tolerate the hemodynamic changes that occur during liver transplantation, it is suggested that heart transplantation be performed prior to liver transplantation [
11]. A number of operative strategies have been published, including (1) a separate staged operation involving heart transplantation followed by liver transplantation, (2) heart transplantation on CPB then liver transplantation after discontinuing CPB during the same operation, and (3) heart and liver transplantation both performed on CPB [
3]. The most widely applied technique is performing the heart transplant on CPB, separating from the bypass, and continuing the liver transplant with selective use of venovenous bypass [
1011].
The patient was receiving ECMO support in the current case, indicating the relative urgency of a heart transplant over that of a liver transplant. The authors decided to begin the cardiac transplantation on CPB and proceed with liver transplantation on ECMO in order to mitigate the hemodynamic stress on the transplanted heart and minimize the cold ischemia time of the liver by omitting the CPB weaning process. Considering the inherent volume-overload condition of cirrhotic patients, cardiac graft function may decline after cessation of CPB [
12]. Moreover, the left bronchus remained collapsed, so achieving adequate gas exchange would have been difficult without an extracorporeal circulatory device.
The underlying pathophysiology of liver cirrhosis poses a challenge to the management of heart transplantation. Cirrhotic patients are characterized by a hyperdynamic state with high cardiac output and low systemic vascular resistance, mandating increased vasopressor support during anesthesia [
13]. Balanced anesthesia via a combination of intravenous drugs with minimal suppression on hemodynamics (
e.g., etomidate, opioids) and low-dose inhalation agents to avoid excessive vasopressor use is essential [
14]. In addition, hepatic dysfunction causes acid/base disorders, thrombocytopenia, and imbalance between procoagulant and anticoagulant factors, which is complicated by the use of hemodynamic support devices (
e.g., ECMO, CPB) [
15]. The authors conducted prudent transfusion of blood products intraoperatively, referring to consecutive coagulation profiles and clinical estimation of blood loss.
The newly grafted heart is also subject to specific obstacles during liver transplantation. The heart allograft possesses a normal Starling relationship between end-diastolic volume and cardiac output, and is therefore vulnerable to a sudden decrease in preload—which is frequently encountered during inferior vena cava clamping [
13]. Conversely, excessive volume overload as a result of massive fluid infusion during liver transplantation may compromise the graft's right ventricular function, leading to right heart failure [
12]. Continuous monitoring of central venous pressure and transesophageal echocardiography are pivotal in determining the recipient's volume status, which can be managed via resuscitation, diuresis, or vasoactive agents [
12]. The authors integrated various hemodynamic parameters with the information provided by transesophageal echocardiography to aid fluid therapy and inotropic use. Also, cirrhosis-induced electrolyte disorder, volume redistribution, and metabolic acidosis from reperfusion of the liver graft should be promptly managed because such conditions may jeopardize cardiac function and increase the risk of arrhythmias [
13].
In conclusion, many factors should be taken into account for a successful CHLT, due to the burden of two surgical procedures and the reduced physiologic reserve of the recipient associated with concurrent cardiac and hepatic dysfunction. Evidence is accumulating that CHLT is a safe procedure with a favorable outcome for selected patients with dual organ failure who would be precluded from either heart or liver transplantation alone. With individualized anesthetic and surgical methods focusing on adequate organ perfusion, optimal graft function, and minimizing perioperative complications, CHLT may ultimately become the standard of care.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download