Abstract
It is well known that diabetic patients have a high risk of cardiovascular events, and although there has been a tremendous effort to reduce these cardiovascular risks, the incidence of cardiovascular morbidity and mortality in diabetic patients remains high. Therefore, the early detection of coronary artery disease (CAD) is necessary in those diabetic patients who are at risk of cardiovascular events. Significant medical and radiological advancements, including coronary computed tomography angiography (CCTA), mean that it is now possible to investigate the characteristics of plaques, instead of solely evaluating the calcium level of the coronary artery. Recently, several studies reported that the prevalence of subclinical coronary atherosclerosis (SCA) is higher than expected, and this could impact on CAD progression in asymptomatic diabetic patients. In addition, several reports suggest the potential benefit of using CCTA for screening for SCA in asymptomatic diabetic patients, which might dramatically decrease the incidence of cardiovascular events. For these reasons, the medical interest in SCA in diabetic patients is increasing. In this article, we sought to review the results of studies on CAD in asymptomatic diabetic patients and discuss the clinical significance and possibility of using CCTA to screen for SCA.
Cardiovascular (CV) disease is the main cause of death in diabetic patients [1], with diabetic patients having a 2- to 4-fold higher risk of a CV event than nondiabetic patients. Furthermore, diabetic patients can sometimes be asymptomatic, even after progression of CV disease. Therefore, it is necessary to identify those patients with diabetes who are at risk of CV events before the onset of their symptoms. The American Diabetes Association reviewed the issue of coronary artery disease (CAD) screening in patients with diabetes to identify high-risk subgroups and improve their CV outcome with intensive modification of risk factors, medical surveillance, and revascularization [2]. However, the risk assessment may be limited, because nuclear and echocardiography stress tests have a poor prognostic value in diabetic patients compared with the general population with suspected CAD [234].
The emergence of high-resolution multi-detector coronary computed tomography angiography (CCTA) has provided an opportunity to evaluate coronary anatomy noninvasively, and to determine the presence and extent of coronary atherosclerosis [5]. Several CCTA studies showed that diabetic patients have a higher prevalence of CAD and fewer normal coronary arteries than nondiabetic patients [67]. Nevertheless, the recent European Society of Cardiology guidelines do not recommend CCTA for risk assessment and advise the use of other noninvasive image testing methods in high-risk diabetic patients [8]. By contrast, the American College of Cardiology Foundation/American Heart Association guidelines for detection and risk assessment of CAD suggest that CCTA may be appropriate in high-risk diabetic patients [9]. In this article, we sought to review the impact of subclinical coronary atherosclerosis (SCA) on asymptomatic diabetic patients, and to determine the relevance of SCA as an important risk factor in the screening of asymptomatic diabetic patients before they present with symptoms of CAD.
The actual prevalence of SCA in a truly representative population of diabetic patients has not been ascertained. Previous studies exploring the association between CV risk factors and CCTA-determined coronary atherosclerotic burden in type 2 diabetes mellitus (T2DM) patients have shown various prevalence rates for SCA. A large cohort study (the Multi-Ethnic Study of Atherosclerosis) reported that 63% of diabetic patients had a coronary artery calcium (CAC) score >0, compared with 48% of those subjects without diabetes [7]. In a similar manner, a Korean single-center registry study indicated that plaque of any type was more frequently observed in patients with diabetes than in patients without diabetes (58.4% vs. 51.2%, P=0.001) [6]. In an article focusing on Southern Asians, asymptomatic T2DM patients had a higher rate of CAC score >0 (69% vs. 55%, P<0.05) and more obstructive CAD (39% vs. 27%, P<0.05) than Caucasian patients selected according to matched criteria [10]. The differences in prevalence could be explained by the diversity in race. Another study reported that the differences in CAC score associated with diabetes varied with race, with values of 1.37 (95% confidence interval [CI], 1.03 to 1.81) in Caucasians, 1.38 (95% CI, 1.02 to 1.87) in Hispanics, 1.58 (95% CI, 1.20 to 2.09) in African Americans, and 2.37 (95% CI, 1.59 to 3.53) in Chinese [11]. However, the relationships between risk factors and CAC showed no significant differences between races. Thus, the racial differences in CAC prevalence among diabetic patients are likely due to unmeasured risk factors and genetic susceptibility [12]. As many previous studies were confined to Western populations and the prevalence of SCA in diabetic patients differs between countries, there is a need to investigate the actual prevalence of SCA in diabetic patients in each individual country.
The technology behind CCTA has advanced dramatically, with the result that physicians can now investigate the characteristics of plaque, instead of only evaluating the calcium level of the coronary artery. Published studies assessing plaque characteristics have shown a relatively high proportion of nonobstructive plaques in diabetes, ranging from 70% to 80% [1314]. In terms of plaque constitution, previous studies reported that 34% and 41% of plaques were classified as noncalcified plaque, proportions that are higher than those of 21% and 24% in nondiabetic patients [61314]. These noncalcified plaques were associated with a family history of diabetes, and newly diagnosed patients tended to have a large volume of noncalcified plaque, especially patients with asymptomatic diabetes [1516]. Asymptomatic diabetic patients therefore appear to have a relatively high prevalence of noncalcified plaques, with these being mainly nonobstructive. Although such nonobstructive lesions are not associated with induced ischemia, plaque rupture may occur frequently in nonobstructive plaques (Fig. 1) [17]. Therefore, the detection of an increased nonobstructive plaque burden using CCTA may be clinically important in asymptomatic diabetes patients with a familial history of CAD and those patients who have been recently diagnosed with asymptomatic diabetes.
An analysis of the locations of CAD lesions revealed that 30.5% of patients had significant CAD, and that 16.5% of patients showed a significant stenosis in the left main or proximal left anterior descending artery on CCTA [13]. Although asymptomatic diabetes patients showed a higher CAC score and more significant CAD than nondiabetic subjects, there were no significant differences in high-risk CAD, which was defined as at least 2-vessel CAD with proximal left anterior descending artery involvement, 3-vessel CAD, or left main disease [6]. These characteristics of coronary atherosclerotic plaque in asymptomatic CAD in diabetic patients were summarized in Table 1. According to the studies published so far, high-risk CAD involvement is not related to the presence of diabetes, although the volume of atherosclerosis or plaque invading the coronary arteries, and unstable features of plaque, are associated with diabetes [6131819].
Diabetic patients are characterized by the presence of an accelerated progressive atheroma burden with a significantly increased incidence of CV events [20]. A recent study reported that asymptomatic patients with newly diagnosed diabetes had plaque features associated with increased vulnerability [16], a finding that indicates that early-stage diabetic patients constitute an important therapeutic target for the prevention of future CV events. Several studies have investigated the predictors of atherosclerosis progression and the impact of atherosclerosis progression on CV events in diabetic patients. These have reported rates of atherosclerosis progression ranging from 8.8% to 29.6% during follow-up periods (about 2 years) [212223]. The determinants of progression of CAC in diabetic patients were established as age, male gender, blood pressure, smoking, hyperlipidemia, waist-hip ratio, duration of diabetes, presence of retinopathy, statin use, white race, and Framingham risk score [21].
There are conflicting opinions over reducing CAC or coronary atherosclerosis in diabetic patients by strict glycemic control. While one study did not find a decrease in the progression of CAC by intensive glycemic control [24], other studies reported that patients with suboptimal glycemic control had more progression of CAC, and that a poor prognosis was observed in those patients where coronary atherosclerosis had already occurred [2325]. A recent study revealed that, in well-controlled diabetic patients, blood pressure, statin use, and the length of coronary artery lesions were independent factors predicting progression of CAC and atherosclerosis [25]. Therefore, good glycemic control could be important in the progression of CAC or atherosclerosis, and many clinical risk factors could aggravate plaque in asymptomatic diabetic patients.
Although it is an invasive and complicated technique, fractional flow reserve (FFR) is nowadays considered the most accurate method for detecting coronary ischemia. The Fractional Flow Reserve vs. Angiography for Multivessel Evaluation (FAME) trial demonstrated FFR to be a clinical and prognostic standard method, because its ability to guide decisions on revascularization resulted in better clinical outcomes than angiographic-guided revascularization [26]. In the FAME study, 47% of lesions were considered intermediate in stenosis severity, with only one-third of these lesions resulting in coronary ischemia [27]. A prospective clinical head-to-head comparative study in suspected CAD patients compared the diagnostic accuracy of CCTA, single-photon emission computed tomography (SPECT), and positron emission tomography with examination of all coronary arteries by FFR [28]. CCTA exhibited a high sensitivity (90%) and negative predictive value (89%), even in comparison with FFR [28]. SPECT was limited by a high rate of false negatives in cases of balanced ischemia, such as 3-vessel disease or left main disease. This limitation was also identified in a recently published meta-analysis suggesting a low sensitivity for SPECT in comparison with the FFR reference standard [29]. Therefore, despite a lack of information on the coronary functional state, CCTA is a powerful noninvasive method for ruling out hemodynamically significant CAD.
Nevertheless, the most recent American Diabetic Association guidelines recommend against screening for CV disease in asymptomatic diabetic patients, because there is a paucity of data suggesting any specific benefits of invasive interventions over medical therapy alone [30]. However, many potential reasons for appropriate screening of obstructive CAD may still remain. First, the identification of asymptomatic CAD by appropriate screening could result in the provision of precise and appropriate treatment strategies for patients, such as suggesting more aggressive lifestyle modification and better medical or invasive interventions, efforts that may dramatically decrease the CV death rate. In addition, effective screening of obstructive CAD could help prevent the various complications associated with CAD, including heart failure and arrhythmias, and eventually the overall cost of managing diabetic patients may be significantly reduced. In patient trials, traditional individual risk factors for predicting CAD are subject to limitations such as overestimation and heterogeneity, and it takes a long time for diseases to present, and hence to evaluate risk factors. For these reasons, the detection of subclinical atherosclerosis or the screening of CAD in asymptomatic diabetic patients is valuable, and options has been suggested for overcoming several limitations of the traditional risk factors.
In the Detection of Ischemia in Asymptomatic Diabetics (DIAD) trial, no significant differences in cardiac death or nonfatal myocardial infarction were found between the screened and not-screened subjects, because the screening group showed a low rate of CV events that was below the expectation, as well as less coronary revascularizations [31]. One randomized trial has evaluated the use of CCTA in asymptomatic patients. The Effect of Screening for Coronary Artery Disease Using CT Angiography on Mortality and Cardiac Events in High-Risk Patients with Diabetes (FACTOR-64 study) showed that patients with diabetes and large amounts of coronary atherosclerosis did not show reduced rates of CV events after changes in medical care, because the overall CV event rate was lower than expected [32]. Another recent study, the Does Coronary Atherosclerosis Deserve to be Diagnosed Early in Diabetic Patients (DADDY-D) study, enrolled diabetic patients without CAD, who were then randomly assigned to screening for silent myocardial ischemia followed by revascularization or to continuing follow-up [33]. Again, only a small portion (4.6%) of the screened patients received revascularization, and therefore this study failed to demonstrate a significant reduction in CV events, a finding similar to those of previous studies (Table 2). To date, there are no data demonstrating improvement in clinical outcomes with the use of CCTA screening in asymptomatic diabetic patients. Possible reasons for failure of previous studies include a lower manifestation of CV events after optimal management during follow-up and coronary revascularization, which is not able to reduce future CV events in asymptomatic patients. Because of the low CV risk of asymptomatic diabetes, previous studies could not provide evidence demonstrating the effectiveness of screening using CCTA.
To overcome this, a risk-score model for the assessment of CAD was suggested for use in asymptomatic diabetes. Several studies show that CCTA is an effective method for risk assessment and re-stratification in high-risk asymptomatic patients with diabetes [343536]. After formulating a risk-score model with variables for significant CAD, the low- (≤3), intermediate- (4 to 6), and high-risk (≥7) groups showed significant differences in 5-year cardiac event-free survival rate (96.6%±1.5% vs. 88.9%±1.8% vs. 73.8%±4.1%, respectively; log-rank P for trend <0.001) and the probability of CAD (12.6% vs. 29.4% vs. 57.7%, respectively; P for all <0.001) [36]. On the basis of this CAD risk-score model, the authors proposed that further evaluations for CAD are not recommended for low-risk patients, that CAC scoring may be appropriate as a screening test for intermediate-risk patients, and that CCTA might be considered as a first-line test for high-risk patients (Fig. 2) [36]. Another method suggested for overcoming the limitations shown by the screening studies is to use a noninvasive technique for the determination of FFR for selected coronary segments; this can be accomplished through analysis of CCTA [37]. CCTA-derived FFR enables noninvasive assessment of the hemodynamic significance of coronary artery lesions coupled with determination of the anatomical severity of a coronary stenosis. Prior multicenter trials showed CCTA-derived FFR to have a generally high diagnostic performance [3839]. Although no study has reported on the diagnostic accuracy of CCTA-derived FFR in asymptomatic diabetic patients, we expect that it will be a good method for risk assessment in high-risk asymptomatic diabetic patients.
In summary, the prevalence of SCA in diabetic patients is high, and the progression of coronary atherosclerosis leads to the onset of future CV events and is associated with a poor prognosis. Although CCTA screening has not yet been demonstrated as improving the outcomes of asymptomatic diabetic patients, it has been shown to be beneficial in predicting future risk, and is promising for screening with an additional technique.
References
1. Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med. 2007; 147:149–155. PMID: 17576993.

2. Bax JJ, Inzucchi SE, Bonow RO, Schuijf JD, Freeman MR, Barrett EJ. Global Dialogue Group for the Evaluation of Cardiovascular Risk in Patients with Diabetes. Cardiac imaging for risk stratification in diabetes. Diabetes Care. 2007; 30:1295–1304. PMID: 17259467.

3. Kamalesh M, Feigenbaum H, Sawada S. Assessing prognosis in patients with diabetes mellitus: the Achilles' heel of cardiac stress imaging tests? Am J Cardiol. 2007; 99:1016–1019. PMID: 17398204.
4. Elhendy A, Arruda AM, Mahoney DW, Pellikka PA. Prognostic stratification of diabetic patients by exercise echocardiography. J Am Coll Cardiol. 2001; 37:1551–1557. PMID: 11345364.

5. American College of Cardiology Foundation Task Force on Expert Consensus Documents. Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, Hlatky MA, Hodgson JM, Lauer MS, Miller JM, Morin RL, Mukherjee D, Poon M, Rubin GD, Schwartz RS. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol. 2010; 55:2663–2699. PMID: 20513611.
6. Park GM, Lee JH, Lee SW, Yun SC, Kim YH, Cho YR, Gil EH, Kim TS, Kim CJ, Cho JS, Park MW, Her SH, Yang DH, Kang JW, Lim TH, Koh EH, Lee WJ, Kim MS, Lee KU, Kim HK, Choe J, Park JY. Comparison of coronary computed tomographic angiographic findings in asymptomatic subjects with versus without diabetes mellitus. Am J Cardiol. 2015; 116:372–378. PMID: 26037293.

7. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002; 156:871–881. PMID: 12397006.
8. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F. European Association for Cardiovascular Prevention & Rehabilitation (EACPR). ESC Committee for Practice Guidelines (CPG). European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The fifth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012; 33:1635–1701. PMID: 22555213.
9. Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, Kramer CM, Min JK, Patel MR, Rosenbaum L, Shaw LJ, Stainback RF, Allen JM. American College of Cardiology Foundation Appropriate Use Criteria Task Force. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology foundation appropriate use criteria task force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014; 63:380–406. PMID: 24355759.
10. Gobardhan SN, Dimitriu-Leen AC, van Rosendael AR, van Zwet EW, Roos CJ, Oemrawsingh PV, Kharagjitsingh AV, Jukema JW, Delgado V, Schalij MJ, Bax JJ, Scholte AJ. Prevalence by computed tomographic angiography of coronary plaques in South Asian and white patients with type 2 diabetes mellitus at low and high risk using four cardiovascular risk scores (UKPDS, FRS, ASCVD, and JBS3). Am J Cardiol. 2017; 119:705–711. PMID: 28024655.

11. Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2005; 111:1313–1320. PMID: 15769774.

12. Wagenknecht LE, Divers J, Bertoni AG, Langefeld CD, Carr JJ, Bowden DW, Elbein SC, Shea S, Lewis CE, Freedman BI. Correlates of coronary artery calcified plaque in blacks and whites with type 2 diabetes. Ann Epidemiol. 2011; 21:34–41. PMID: 21130367.

13. Park GM, Lee SW, Cho YR, Kim CJ, Cho JS, Park MW, Her SH, Ahn JM, Lee JY, Park DW, Kang SJ, Kim YH, Lee CW, Koh EH, Lee WJ, Kim MS, Lee KU, Kang JW, Lim TH, Park SW, Park SJ, Park JY. Coronary computed tomographic angiographic findings in asymptomatic patients with type 2 diabetes mellitus. Am J Cardiol. 2014; 113:765–771. PMID: 24528613.

14. Scholte AJ, Schuijf JD, Kharagjitsingh AV, Jukema JW, Pundziute G, van der Wall EE, Bax JJ. Prevalence of coronary artery disease and plaque morphology assessed by multi-slice computed tomography coronary angiography and calcium scoring in asymptomatic patients with type 2 diabetes. Heart. 2008; 94:290–295. PMID: 17646190.

15. Park GM, Cho YR, Lee SW, Yun SC, Gil EH, Kim DW, Kim TS, Kim CJ, Cho JS, Park MW, Her SH, Kim YH, Yang DH, Kang JW, Lim TH, Jung CH, Koh EH, Lee WJ, Kim MS, Lee KU, Kim HK, Choe J, Park JY. Family history of diabetes and the risk of subclinical atherosclerosis. Diabetes Metab. 2016; 42:170–177. PMID: 26455871.

16. Mrgan M, Funck KL, Gaur S, Ovrehus KA, Dey D, Kusk MW, Nørgaard BL, Gram JB, Olsen MH, Gram J, Sand NPR. High burden of coronary atherosclerosis in patients with a new diagnosis of type 2 diabetes. Diab Vasc Dis Res. 2017; 14:468–476. PMID: 28866908.

17. Wackers FJ. Asymptomatic patients with diabetes mellitus should be screened for coronary artery disease. J Nucl Cardiol. 2006; 13:609–615. PMID: 16945739.

18. Pundziute G, Schuijf JD, Jukema JW, Boersma E, de Roos A, van der Wall EE, Bax JJ. Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol. 2007; 49:62–70. PMID: 17207724.

19. Min JK, Berman DS, Dunning A, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan K, Chow BJ, Cury R, Delago A, Feuchtner G, Hadamitzky M, Hausleiter J, Kaufmann P, Karlsberg RP, Kim YJ, Leipsic J, Lin FY, Maffei E, Plank F, Raff G, Villines T, Labounty TM, Shaw LJ. All-cause mortality benefit of coronary revascularization vs. medical therapy in patients without known coronary artery disease undergoing coronary computed tomographic angiography: results from CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter Registry). Eur Heart J. 2012; 33:3088–3097. PMID: 23048194.

20. Nicholls SJ, Tuzcu EM, Kalidindi S, Wolski K, Moon KW, Sipahi I, Schoenhagen P, Nissen SE. Effect of diabetes on progression of coronary atherosclerosis and arterial remodeling: a pooled analysis of 5 intravascular ultrasound trials. J Am Coll Cardiol. 2008; 52:255–262. PMID: 18634979.
21. Anand DV, Lim E, Darko D, Bassett P, Hopkins D, Lipkin D, Corder R, Lahiri A. Determinants of progression of coronary artery calcification in type 2 diabetes role of glycemic control and inflammatory/vascular calcification markers. J Am Coll Cardiol. 2007; 50:2218–2225. PMID: 18061069.
22. Kiramijyan S, Ahmadi N, Isma'eel H, Flores F, Shaw LJ, Raggi P, Budoff MJ. Impact of coronary artery calcium progression and statin therapy on clinical outcome in subjects with and without diabetes mellitus. Am J Cardiol. 2013; 111:356–361. PMID: 23206921.

23. Ndrepepa G, Iijima R, Kufner S, Braun S, Cassese S, Byrne RA, Sorges J, Schulz-Schupke S, Hoppmann P, Fussaro M, Laugwitz KL, Schunkert H, Kastrati A. Association of progression or regression of coronary artery atherosclerosis with long-term prognosis. Am Heart J. 2016; 177:9–16. PMID: 27297844.

24. Saremi A, Moritz TE, Anderson RJ, Abraira C, Duckworth WC, Reaven PD. Veterans Affairs Diabetes Trial (VADT). Rates and determinants of coronary and abdominal aortic artery calcium progression in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care. 2010; 33:2642–2647. PMID: 20807873.

25. Kataoka Y, Yasuda S, Miyamoto Y, Sase K, Kosuge M, Kimura K, Yoshimasa Y, Miyazaki S. DIANA study investigators. Clinical predictors of atheroma progression despite optimal glycemic control in early-stage diabetic patients with coronary artery disease: insight from the DIANA study. J Atheroscler Thromb. 2014; 21:509–518. PMID: 24430787.

26. De Bruyne B, Fearon WF, Pijls NH, Barbato E, Tonino P, Piroth Z, Jagic N, Mobius-Winckler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engstrom T, Oldroyd K, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Limacher A, Nuesch E, Juni P. FAME 2 Trial Investigators. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014; 371:1208–1217. PMID: 25176289.

27. Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, Maccarthy PA, Van't Veer M, Pijls NH. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010; 55:2816–2821. PMID: 20579537.
28. Danad I, Raijmakers PG, Driessen RS, Leipsic J, Raju R, Naoum C, Knuuti J, Maki M, Underwood RS, Min JK, Elmore K, Stuijfzand WJ, van Royen N, Tulevski II, Somsen AG, Huisman MC, van Lingen AA, Heymans MW, van de Ven PM, van Kuijk C, Lammertsma AA, van Rossum AC, Knaapen P. Comparison of coronary CT angiography, SPECT, PET, and hybrid imaging for diagnosis of ischemic heart disease determined by fractional flow reserve. JAMA Cardiol. 2017; 2:1100–1107. PMID: 28813561.

29. Danad I, Szymonifka J, Twisk JWR, Norgaard BL, Zarins CK, Knaapen P, Min JK. Diagnostic performance of cardiac imaging methods to diagnose ischaemia-causing coronary artery disease when directly compared with fractional flow reserve as a reference standard: a meta-analysis. Eur Heart J. 2017; 38:991–998. PMID: 27141095.

30. Fox CS, Golden SH, Anderson C, Bray GA, Burke LE, de Boer IH, Deedwania P, Eckel RH, Ershow AG, Fradkin J, Inzucchi SE, Kosiborod M, Nelson RG, Patel MJ, Pignone M, Quinn L, Schauer PR, Selvin E, Vafiadis DK. American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health. Council on Clinical Cardiology, Council on Cardiovascular and Stroke Nursing, Council on Cardiovascular Surgery and Anesthesia, Council on Quality of Care and Outcomes Research. American Diabetes Association. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2015; 38:1777–1803. PMID: 26246459.

31. Bansal S, Wackers FJ, Inzucchi SE, Chyun DA, Davey JA, Staib LH, Young LH. DIAD Study Investigators. Five-year outcomes in high-risk participants in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study: a post hoc analysis. Diabetes Care. 2011; 34:204–209. PMID: 20929989.
32. Muhlestein JB, Lappe DL, Lima JA, Rosen BD, May HT, Knight S, Bluemke DA, Towner SR, Le V, Bair TL, Vavere AL, Anderson JL. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA. 2014; 312:2234–2243. PMID: 25402757.
33. Turrini F, Scarlini S, Mannucci C, Messora R, Giovanardi P, Magnavacchi P, Cappelli C, Evandri V, Zanasi A, Romano S, Cavani R, Ghidoni I, Tondi S, Bondi M. Does coronary Atherosclerosis Deserve to be Diagnosed earlY in Diabetic patients? The DADDY-D trial. Screening diabetic patients for unknown coronary disease. Eur J Intern Med. 2015; 26:407–413. PMID: 26058988.

34. Min JK, Labounty TM, Gomez MJ, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan KM, Chow B, Cury R, Delago A, Dunning A, Feuchtner G, Hadamitzky M, Hausleiter J, Kaufmann P, Kim YJ, Leipsic J, Lin FY, Maffei E, Raff G, Shaw LJ, Villines TC, Berman DS. Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis. 2014; 232:298–304. PMID: 24468142.

35. Fujimoto S, Kondo T, Kodama T, Orihara T, Sugiyama J, Kondo M, Endo A, Fukazawa H, Nagaoka H, Oida A, Ikeda T, Yamazaki J, Takase S, Narula J. Coronary computed tomography angiography-based coronary risk stratification in subjects presenting with no or atypical symptoms. Circ J. 2012; 76:2419–2425. PMID: 22864230.

36. Park GM, An H, Lee SW, Cho YR, Gil EH, Her SH, Kim YH, Lee CW, Koh EH, Lee WJ, Kim MS, Lee KU, Kang JW, Lim TH, Park SW, Park SJ, Park JY. Risk score model for the assessment of coronary artery disease in asymptomatic patients with type 2 diabetes. Medicine (Baltimore). 2015; 94:e508. PMID: 25634204.

37. Min JK, Taylor CA, Achenbach S, Koo BK, Leipsic J, Norgaard BL, Pijls NJ, De Bruyne B. Noninvasive fractional flow reserve derived from coronary CT angiography: clinical data and scientific principles. JACC Cardiovasc Imaging. 2015; 8:1209–1222. PMID: 26481846.
38. Norgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, Jensen JM, Mauri L, De Bruyne B, Bezerra H, Osawa K, Marwan M, Naber C, Erglis A, Park SJ, Christiansen EH, Kaltoft A, Lassen JF, Botker HE, Achenbach S. NXT Trial Study Group. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol. 2014; 63:1145–1155. PMID: 24486266.
39. Leipsic J, Yang TH, Thompson A, Koo BK, Mancini GB, Taylor C, Budoff MJ, Park HB, Berman DS, Min JK. CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve: results from the Determination of Fractional Flow Reserve by Anatomic CTA (DeFACTO) study. AJR Am J Roentgenol. 2014; 202:989–994. PMID: 24758651.

Fig. 1
Examples of different coronary computed tomography findings. Curved multiplanar reconstructions of the (A) left anterior descending (LAD) coronary artery, (B) left circumflex coronary artery, and (C) right coronary artery of a patient with normal coronary arteries. The curved multiplanar reconstruction of the LAD shows tubular coronary artery disease with a nonobstructive and noncalcified lesion (arrow, D) in a newly diagnosed diabetic patient.
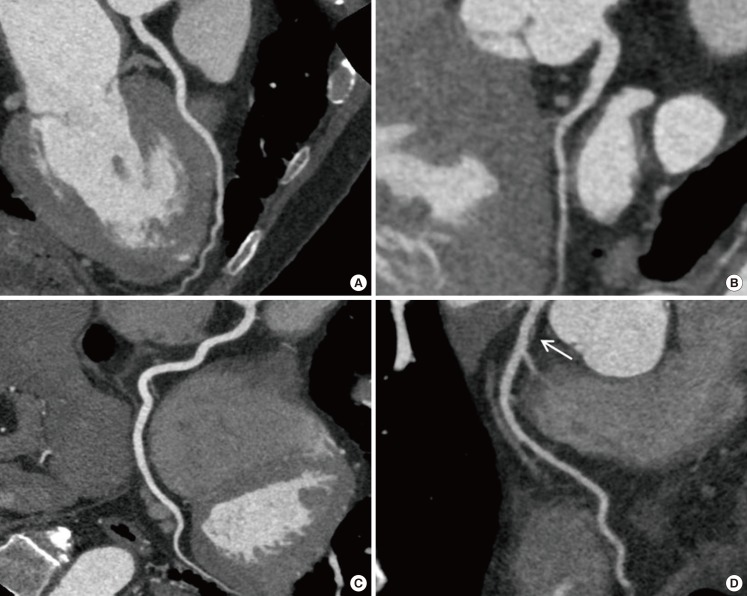
Fig. 2
Proposed algorithm for individualized coronary artery disease (CAD) screening in asymptomatic type 2 diabetes mellitus patients based on a risk-score model. Adapted from Park et al. [36]. CT, computed tomography.
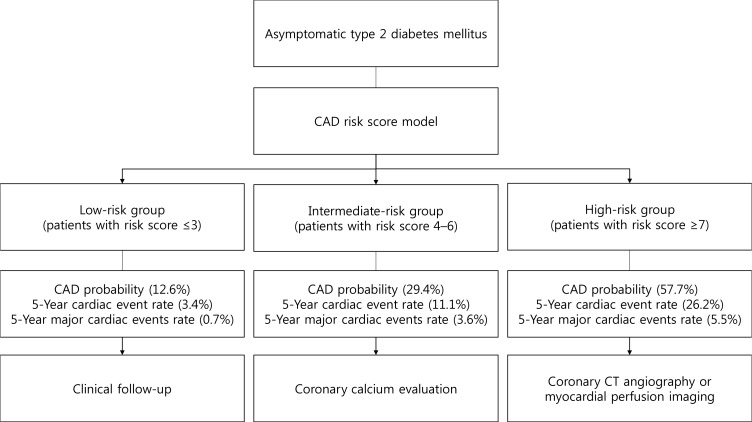
Table 1
Characteristics of coronary atherosclerotic plaque in asymptomatic coronary artery disease in patients with diabetic mellitus
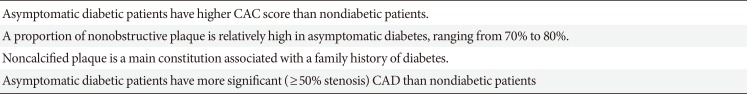
Table 2
Descriptions of the studies for screening of asymptomatic coronary artery disease in patients with diabetic mellitus
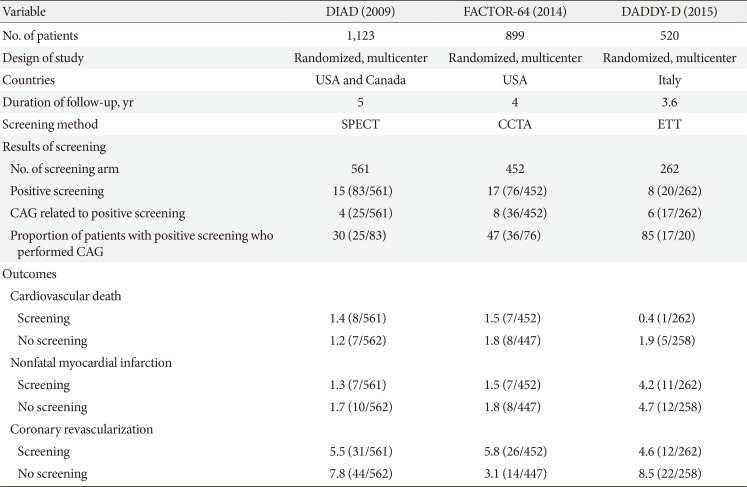
Values are presented as percentage (number/total number).
DIAD, Detection of Ischemia in Asymptomatic Diabetics; FACTOR-64, Screening for Asymptomatic Obstructive Coronary Artery Disease among High-Risk Diabetic Patients Using CT Angiography, Following Core 64; DADDY-D, Does Coronary Atherosclerosis Deserve to be Diagnosed Early in Diabetic Patients; SPECT, single-photon emission computed tomography; CCTA, coronary computed tomography angiography; ETT, exercise tolerance test; CAG, coronary angiography.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download