Abstract
The prevalence of diabetes in Korea has increased six- to sevenfold over the past 40 years with its complications becoming major causes of morbidity and mortality. The rate of death among patients with diabetes is about twice as high as that among persons without diabetes and the most common cause of death is cardiovascular disease (30.6%). Despite the seriousness of diabetic complications, 30 to 70% of patients receive inadequate care, and only 40% of treated diabetic patients achieve the optimal control with HbA1c level <7% in Korea. In 2006, over 30 to 40% of patients with diabetes have microvascular complications and around 10% of them have macrovascular complications from our national data. Despite there are some debates about intensive glycemic control resulting in the deterioration of macrovascular complication, multifactorial treatment approaches including proper glycemic control are important to prevent diabetic complications. There have been needs for finding proper biomarkers for predicting diabetic complications properly but we still need more longitudinal studies to find this correlation with causal relationship. In this article, we wanted to review the recent status of micro- and macrovascular complications of type 2 diabetes in Korea from integration of many epidemiologic studies.
The prevalence of diabetes in Korea has increased six- to sevenfold from 1.5 to 9.9% over the past 40 years [1,2]. The number of people with diabetes worldwide is expected to increase 11.4% from 366 million in 2011 to 552 million by 2030, affecting one in 10 adults [3]. The same trend is expected in Korea. This global increase in the prevalence of diabetes will inevitably lead to increases in the prevalence of diabetic microvascular and macrovascular diseases, and consequently, significantly increased health care expenditure [4].
In Korea, type 2 diabetic patients without complications spend about 1,184,563 won annually on health care. Diabetic patients with microvascular disease spend up to 4.7 times as much, patients with macrovascular disease up to 10.7 times as much, and patients with both complications 8.8 times as much as those with no complications. The medical cost of diabetes mellitus covered by the national health insurance corporation is 3.2 trillion won and accounted for 19.2% of all medical costs [5].
Diabetes and its complications have become major causes of morbidity and mortality in Korea [6]. Although diabetes-related mortality has decreased recently from 25.1 per 100,000 persons in 2002 to 19.6 per 100,000 persons in 2009, diabetes is still the fifth-leading cause of death in Korea [6]. The rate of death among patients with diabetes is about twice as high as that among persons without diabetes [7]. The most common cause of death is cardiovascular disease (30.6%), followed by infectious disease (25.3%), cancer (21.9%), congestive heart failure (7.1%), renal disease (4.7%), liver disease (2.7%), and diabetes itself (1.9%) [2].
Despite the seriousness of diabetic complications, 30% to 70% of patients receive inadequate care [8], and only 40% of treated diabetic patients achieve the optimal control, defined as an HbA1c level <7% [8,9]. The serious outcomes from diabetic complications and inadequate glucose control in diabetic patients prompt the need for more aggressive efforts to provide optimal metabolic control.
Type 2 diabetes mellitus is associated with a high rate of complications related to cardiovascular disease and diabetic nephropathy, retinopathy, and neuropathy. In 2006, 30.3%, 38.3%, and 44.6% of patients were found to have microvascular complications such as microalbuminuria, retinopathy, and neuropathy, respectively from Korean nationwide survey. The prevalence of macrovascular complications including coronary artery disease, cerebrovascular disease, and peripheral artery disease was 8.7%, 6.7%, and 3.0%, respectively [9]. The prevalence of diabetic foot was 4.4%, and 44.8% of patients with an amputated foot had diabetes mellitus [8,10]. The prevalence of macrovascular complications seems underestimated in these data. In a study of 343 patients with diabetes mellitus, the prevalence of cardiovascular complication was 23.6% [11], and in another study of 406 patients with diabetes, extracranial internal carotid artery stenosis ≥40% was detected in 5.2% of the patients [12]. In addition, the prevalence of macrovascular complication was 10.8% from recent The Korean National Diabetes Program (KNDP) data [13] and there is reference from 2005 Korea National Health and Nutrition Examination Survey (KNHANES) data in Table 1.
The role of hyperglycemia in the development of microvascular complications of diabetes, such as nephropathy, retinopathy, and neuropathy, is well documented. The incidence of microvascular complications begins to increase at an HbA1c level >7.0% and increases by 30% to 40% per 1% increase in HbA1c level from over 8,000 patients (Fig. 1). Microvascular complications are closely related to age, duration of diabetes, and glycemic control, and this relationship is stronger than that with macrovascular complications [9].
Diabetic retinopathy is the most common microvascular complication of diabetes mellitus, and its prevalence is strongly related to the duration of diabetes. It is the most frequent cause of new cases of blindness among adults aged 20 to 74 years. In Ansung cohort study (prospective, rural, community cohort in Korea), the prevalence of any diabetic retinopathy was 2.9% and the proper cutoff of HbA1C value for detecting any diabetic retinopathy was 6.6% (unpublished data).
Diabetic nephropathy is characterized by albuminuria (≥300 mg/day) and a reduced glomerular filtration rate. It is often present at the time of the diagnosis of diabetes after the kidney has been exposed to chronic hyperglycemia during the prediabetic phase. Patients with microalbuminuria who progress to macroalbuminuria (300 mg/24 hr) are likely to progress to end-stage renal disease (ESRD) [14]. Diabetes is a major cause of chronic kidney disease (CKD) and is recognized as the most common cause of ESRD in the USA and Korea. About 40% of United States adults with diagnosed or undiagnosed diabetes had some degree of CKD in the 1999 to 2006 National Health and Nutrition Examination Survey [15]. In Korea, 56.7% of CKD patients and 70.5% of ESRD patients has diabetes [8].
The prevalence of peripheral neuropathy has been estimated at 40.0% to 44.6% [9,10]. At present, there is no specific treatment for the underlying nerve damage other than to improve glycemic control, which may slow the progression modestly. Glycemic control reduces microvascular complication outcomes but cannot reverse neuronal loss [16].
Type 2 diabetes increases the risk of coronary heart disease by two- to fourfold [17]. The case fatality rate after myocardial infarction is higher in patients with diabetes than in patients without diabetes [18]. The association between diabetes and coronary heart disease is likely to become more important for two reasons. First, the incidence of type 2 diabetes is increasing among both high-risk and low-risk populations. Second, although the rate of death caused by coronary heart disease in the overall population has declined markedly over the past 35 years, this has not been the case among persons with diabetes [7].
Cardiovascular disease is the major cause of morbidity and mortality for individuals with diabetes and is the largest contributor to the direct and indirect costs of diabetes. Older age, high blood pressure, and smoking history are major risk factors for the development of macrovascular complications. A smoking history in males can be both a risk factor and a predictive factor for earlier development of macrovascular complications in Korean patients with type 2 diabetes [19].
Microvascular complications of diabetes increase the risk of cardiovascular events in diabetic patients. Although diabetic retinopathy is not associated with the presence of atherosclerotic plaque, it is associated with increased carotid intima-media thickness, and the increase in intima-media thickness is associated with the presence of plaque, which predisposes patients to cardiovascular disease. Microalbuminuria and a low glomerular filtration rate (<60 mL/min/1.73 m2) increase the risk of major cardiovascular events and death [20,21]. Diabetic polyneuropathy was also independently associated with a high prevalence of cardiovascular disease in type 2 diabetic patients [22]. These data imply that the microvascular complications of diabetes are related indirectly to the macrovascular complications of diabetes, similar in Korea [23].
Intensive glycemic control has been suggested as an effective treatment for reducing the burden of cardiovascular disease and microvascular complications in people with diabetes. The United Kingdom Prospective Diabetes Study and the Kumamoto study showed that early intensive glycemic control can delay the onset and progression of diabetic retinopathy, nephropathy, and neuropathy compared with conventional treatment [21,24-26]. Intensive glucose control involving gliclazide (modified release) and other drugs as required lowered the HbA1c value to 6.5% and reduced by 10% the relative risk for the combined outcome of major macrovascular and microvascular events, primarily because of a 21% reduction in incidence of nephropathy [27]. In addition, the legacy effect was observed after 10 years of trial in the rate of microvascular complication and myocardial infarction [28]. In the Steno-2 study, the intensive therapy group had a 46% lower risk for all-cause mortality and a 57% lower risk of death from cardiovascular causes. One patient in the intensive therapy group progressed to ESRD compared with 6 patients in the conventional therapy group, and fewer patients in the intensive therapy group required retinal laser therapy [29].
Although there are many benefits of intensive glucose-lowering treatment for preventing macrovascular and microvascular events, it remains uncertain whether these benefits outweigh the risks. Intensive blood glucose control decreases the risk of developing microvascular complications but not macrovascular disease in patients with type 2 diabetes. In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study, an intensive glucose-lowering regimen reduced rate of 5-year nonfatal myocardial infarctions but was associated with a 22% increase in mortality [30,31]. A recent meta-analysis found that intensive glucose-lowering treatment has limited effect on the rates of all-cause mortality and death from cardiovascular causes. The data are conflicting: a 9% reduction to a 19% increase in all-cause mortality and a 14% reduction to a 43% increase in cardiovascular death rates. The harm associated with severe hypoglycemia might counterbalance the potential benefit of intensive glucose-lowering treatment [32]. The microvascular benefits of intensive therapy should be weighed against the increase in total and cardiovascular disease-related mortality, weight gain, and high risk of severe hypoglycemia [16].
However, multifactorial approaches in high risk patients with diabetes, such as tight glucose regulation and the use of anti-hypertensive medication, aspirin, and lipid-lowering agents, have been shown to reduce the risk of nonfatal cardiovascular disease among patients with type 2 diabetes mellitus and microalbuminuria. In high risk patients with type 2 diabetes, intensive treatment approaches with multiple drug combinations and behavior modification had sustained beneficial effects with respect to vascular complications and on rates of death from any cause and from cardiovascular causes [29].
Several adipokines are implicated in the metabolic syndrome, coronary heart disease, and insulin resistance. We want to discuss some adipokines, which showed correlation with diabetes and metabolic syndrome in Korea. Lipocalin family proteins, including adipocyte fatty acid-binding protein (A-FABP), lipocalin-2, and retinol-binding protein 4 (RBP4), have been identified recently as adipokines associated with obesity, type 2 diabetes, and the metabolic syndrome. Serum A-FABP is associated with glucose dysregulation, and its level predicts the development of type 2 diabetes and the development of the metabolic syndrome independently of adiposity and insulin resistance [33,34]. Serum A-FABP level is independently associated with carotid atherosclerosis [35]. Serum lipocalin-2 level is significantly elevated in patients with coronary heart disease and is independently associated with coronary heart disease. These findings suggest that serum lipocalin-2 levels may be useful for assessing coronary heart disease risk [36]. Plasma RBP4 concentration is elevated in persons with impaired glucose tolerance and type 2 diabetes [37]. High RBP4 and low plasma adiponectin concentrations are associated with the severity of glucose intolerance in women with previous gestational diabetes mellitus [38].
A low circulating vaspin level correlates with a high fitness level, whereas physical training in untrained individuals increases vaspin serum concentration [39]. Vaspin is also correlated with metabolic syndrome in men and coronary artery stenosis in women [40]. However, another study reported that circulating visfatin may not be a useful clinical biomarker of metabolic status [41].
A relationship between chemerin levels, cardiometabolic parameters, and degree of coronary stenosis has been reported in Korean patients with coronary artery disease [42].
Serum osteocalcin, an osteoblast-specific protein, has several hormonal features and is secreted into the general circulation by osteoblastic cells. Serum osteocalcin and osteoprotegerin levels are associated with glucose metabolism and atherosclerosis parameters in people with type 2 diabetes mellitus [43,44].
Even though there are many studies about adipokines and metabolic diseases, we need large number, prospective studies to see the causality between the candidate adipokines and diabetic complications more clearly.
The increasing prevalence of diabetes mellitus and its related complications have contributed to a substantial increase in morbidity and mortality in Korea. However, the proportion of patients with type 2 diabetes achieving adequate glucose control is relatively low. Multifactorial treatment approaches that target hypertension, dyslipidemia, and microalbuminuria, and that provide intensive glycemic control are urgently needed to control diabetes. These comprehensive and integrated health interventions will lead to further improvement in the management of diabetes.
Figures and Tables
Fig. 1
Odds ratios of diabetic microvascular complications according to the glycemic control status (HbA1c) (From Kim DJ. Diabetes Metab J 2011;35:303-8) [1].
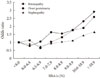
Table 1
Prevalence of type 2 diabetes-related complications in the KNHANES 2005 population

Values are presented as number (%). Statistically significant between males and females by the chi-square test (P<0.05).
KNHANES, Korea National Health and Nutrition Examination Survey; MI, myocardial infarction (From Rhee SY, et al. Diabetes Metab J 2011;35:504-12) [13].
References
1. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011. 35:303–308.
2. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009. 32:2016–2020.
3. International Diabetes Federation. Diabetes atlas. 2011. 5th ed. Brussels: International Diabetes Federation.
4. Harris MI. Diabetes in America: epidemiology and scope of the problem. Diabetes Care. 1998. 21:Suppl 3. C11–C14.
5. Lee KW. Outcome research in diabetes. J Korean Diabetes. 2011. 12:2–5.
6. Statistics Korea: 2009 statistical results about cause of death. 2011. updated 2011 Sep 19. Available from: http://www.index.go.kr.
7. Gu K, Cowie CC, Harris MI. Diabetes and decline in heart disease mortality in US adults. JAMA. 1999. 281:1291–1297.
8. Kim SG, Choi DS. The present state of diabetes mellitus in Korea. J Korean Med Assoc. 2008. 51:791–798.
9. Lim S, Kim DJ, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. A nationwide survey about the current status of glycemic control and complications in diabetic patients in 2006: the Committee of the Korean Diabetes Association on the epidemiology of diabetes mellitus. Korean Diabetes J. 2009. 33:48–57.
10. Nam JH, Lee SH, Lee HJ, Han JH, Kim JG, Ha SW, Kim BW. The prevalence of chronic complications in non-insulin dependent diabetic patients. J Korean Diabetes Assoc. 1999. 23:702–714.
11. Lim S, Koo BK, Cho SW, Kihara S, Funahashi T, Cho YM, Kim SY, Lee HK, Shimomura I, Park KS. Association of adiponectin and resistin with cardiovascular events in Korean patients with type 2 diabetes: the Korean atherosclerosis study (KAS): a 42-month prospective study. Atherosclerosis. 2008. 196:398–404.
12. Park JH, Kim WH, Kim JH, Park TS, Baek HS. Prevalence of and risk factors for extracranial internal carotid artery stenosis in Korean type 2 diabetic patients. Diabet Med. 2006. 23:1377–1380.
13. Rhee SY, Chon S, Kwon MK, Park IB, Ahn KJ, Kim IJ, Kim SH, Lee HW, Koh KS, Kim DM, Baik SH, Lee KW, Nam MS, Park YS, Woo JT, Kim YS. Prevalence of chronic complications in Korean patients with type 2 diabetes mellitus based on the Korean National Diabetes Program. Diabetes Metab J. 2011. 35:504–512.
14. Bakris GL. Recognition, pathogenesis, and treatment of different stages of nephropathy in patients with type 2 diabetes mellitus. Mayo Clin Proc. 2011. 86:444–456.
15. Plantinga LC, Crews DC, Coresh J, Miller ER 3rd, Saran R, Yee J, Hedgeman E, Pavkov M, Eberhardt MS, Williams DE, Powe NR;. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clin J Am Soc Nephrol. 2010. 5:673–682.
16. Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, Cuddihy R, Cushman WC, Genuth S, Grimm RH Jr, Hamilton BP, Hoogwerf B, Karl D, Katz L, Krikorian A, O'Connor P, Pop-Busui R, Schubart U, Simmons D, Taylor H, Thomas A, Weiss D, Hramiak I. ACCORD trial group. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010. 376:419–430.
17. Haffner SM. Coronary heart disease in patients with diabetes. N Engl J Med. 2000. 342:1040–1042.
18. Miettinen H, Lehto S, Salomaa V, Mahonen M, Niemela M, Haffner SM, Pyorala K, Tuomilehto J. The FINMONICA Myocardial Infarction Register Study Group. Impact of diabetes on mortality after the first myocardial infarction. Diabetes Care. 1998. 21:69–75.
19. Lee HR, Yu JM, Choi MG, Yoo HJ, Hong EG. Risk factors for early development of macrovascular complications in Korean type 2 diabetes. Korean Diabetes J. 2009. 33:134–142.
20. Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, Halle JP, Young J, Rashkow A, Joyce C, Nawaz S, Yusuf S. HOPE Study Investigators. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001. 286:421–426.
21. Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, Kojima Y, Furuyoshi N, Shichiri M. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995. 28:103–117.
22. Chung JO, Cho DH, Chung DJ, Chung MY. Association between diabetic polyneuropathy and cardiovascular complications in type 2 diabetic patients. Diabetes Metab J. 2011. 35:390–396.
23. Hong S, Park JH, Lim YH, Park YS, Kim DS, Choi WH, Ahn YH. The relationship between diabetic retinopathy and macrovascular complication in patients with type 2 diabetes. Korean J Med. 2011. 81:351–358.
24. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998. 352:837–853.
25. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998. 317:703–713.
26. ACCORD Study Group. ACCORD Eye Study Group. Chew EY, Ambrosius WT, Davis MD, Danis RP, Gangaputra S, Greven CM, Hubbard L, Esser BA, Lovato JF, Perdue LH, Goff DC Jr, Cushman WC, Ginsberg HN, Elam MB, Genuth S, Gerstein HC, Schubart U, Fine LJ. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010. 363:233–244.
27. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008. 358:2560–2572.
28. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008. 359:1577–1589.
29. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008. 358:580–591.
30. ACCORD Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008. 358:2545–2559.
31. ACCORD Study Group. Gerstein HC, Miller ME, Genuth S, Ismail-Beigi F, Buse JB, Goff DC Jr, Probstfield JL, Cushman WC, Ginsberg HN, Bigger JT, Grimm RH Jr, Byington RP, Rosenberg YD, Friedewald WT. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 2011. 364:818–828.
32. Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassai B, Erpeldinger S, Wright JM, Gueyffier F, Cornu C. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011. 343:d4169.
33. Tso AW, Xu A, Sham PC, Wat NM, Wang Y, Fong CH, Cheung BM, Janus ED, Lam KS. Serum adipocyte fatty acid binding protein as a new biomarker predicting the development of type 2 diabetes: a 10-year prospective study in a Chinese cohort. Diabetes Care. 2007. 30:2667–2672.
34. Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH, Yeung DC, Janus ED, Sham PC, Lam KS. Circulating adipocyte-fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulation. 2007. 115:1537–1543.
35. Yeung DC, Xu A, Cheung CW, Wat NM, Yau MH, Fong CH, Chau MT, Lam KS. Serum adipocyte fatty acid-binding protein levels were independently associated with carotid atherosclerosis. Arterioscler Thromb Vasc Biol. 2007. 27:1796–1802.
36. Choi KM, Lee JS, Kim EJ, Baik SH, Seo HS, Choi DS, Oh DJ, Park CG. Implication of lipocalin-2 and visfatin levels in patients with coronary heart disease. Eur J Endocrinol. 2008. 158:203–207.
37. Cho YM, Youn BS, Lee H, Lee N, Min SS, Kwak SH, Lee HK, Park KS. Plasma retinol-binding protein-4 concentrations are elevated in human subjects with impaired glucose tolerance and type 2 diabetes. Diabetes Care. 2006. 29:2457–2461.
38. Choi SH, Kwak SH, Youn BS, Lim S, Park YJ, Lee H, Lee N, Cho YM, Lee HK, Kim YB, Park KS, Jang HC. High plasma retinol binding protein-4 and low plasma adiponectin concentrations are associated with severity of glucose intolerance in women with previous gestational diabetes mellitus. J Clin Endocrinol Metab. 2008. 93:3142–3148.
39. Youn BS, Kloting N, Kratzsch J, Lee N, Park JW, Song ES, Ruschke K, Oberbach A, Fasshauer M, Stumvoll M, Bluher M. Serum vaspin concentrations in human obesity and type 2 diabetes. Diabetes. 2008. 57:372–377.
40. Choi SH, Kwak SH, Lee Y, Moon MK, Lim S, Park YJ, Jang HC, Kim MS. Plasma vaspin concentrations are elevated in metabolic syndrome in men and are correlated with coronary atherosclerosis in women. Clin Endocrinol (Oxf). 2011. 75:628–635.
41. Ingelsson E, Larson MG, Fox CS, Yin X, Wang TJ, Lipinska I, Pou KM, Hoffmann U, Benjamin EJ, Keaney JF Jr, Vasan RS. Clinical correlates of circulating visfatin levels in a community-based sample. Diabetes Care. 2007. 30:1278–1280.
42. Hah YJ, Kim NK, Kim MK, Kim HS, Hur SH, Yoon HJ, Kim YN, Park KG. Relationship between chemerin levels and cardiometabolic parameters and degree of coronary stenosis in Korean patients with coronary artery disease. Diabetes Metab J. 2011. 35:248–254.
43. Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Kurioka S, Yano S, Sugimoto T. Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2009. 94:45–49.
44. Oh SY, Rhee EJ, Lee WY, Chun HB, Yoo TW, Kang JM, Hwang ST, Kim YC, Oh KW, Oh ES, Baek KH, Kang MI, Kim SW. Relationships between serum osteoprotegerin levels and insulin resistance, cardiovascular risk factors and bone metabolism in type 2 diabetic patients. Korean J Med. 2005. 68:168–177.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download