Abstract
Background
The present study investigated the efficacy and safety of vildagliptin-metformin treatment compared to those of glimepiride-metformin treatment for type 2 diabetes.
Methods
In a randomized, open-label, comparative study, 106 patients with type 2 diabetes were enrolled. The primary endpoint was a reduction in HbA1c from baseline and secondary endpoints included fasting plasma glucose (FPG) or 2-hour postprandial glucose (2h-PPG) reduction from baseline, as well as HbA1c responder rate and HbA1c reduction according to baseline HbA1c category.
Results
Comparable HbA1c reduction was observed with a mean±standard deviation change from baseline to the 32-week endpoint of -0.94±1.15% in the vildagliptin group and -1.00±1.32% in the glimepiride group. A similar reduction in 2h-PPG (vildagliptin group 3.53±4.11 mmol/L vs. the glimepiride group 3.72±4.17 mmol/L) was demonstrated, and the decrements in FPG (vildagliptin group 1.54±2.41 mmol/L vs. glimepiride group 2.16±2.51 mmol/L) were not different between groups. The proportion of patients who achieved an HbA1c less than 7% at week 32 was 50.1% in the vildagliptin group and 56.0% in the glimepiride group. An average body weight gain of 2.53±1.21 kg in the glimepiride group was observed in contrast with the 0.23±0.69 kg weight gain noted in the vildagliptin group. A 10-fold lower incidence of hypoglycemia was demonstrated in the vildagliptin group, in addition to an absence of severe hypoglycemia.
Several clinical studies have demonstrated that tight glycemic control is necessary to prevent diabetic complications in type 2 as well as type 1 diabetic patients [1-4].
However, tight glycemic control is definitely associated with frequent hypoglycemic attacks, and several papers recently reported that aggressive glucose control did not produce any cardiovascular (CV) benefits but rather induced severe hypoglycemia and increased mortality in type 2 diabetes mellitus patients [5-7]. Many type 2 diabetic patients require more than two oral hypoglycemic agents because treatment with a single agent often results in sub-optimal outcomes. Combination therapy early in diabetes management would be a proper approach considering the complex pathophysiologic defects associated with diabetes.
Recently, several new classes of oral hypoglycemic agents have been introduced [8-10]. Vildagliptin is an oral and highly selective dipeptidyl peptidase-4 (DPP-4) inhibitor which prevents the rapid degradation of endogenous glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP) and increases the levels of the intact, active form of endogenous GLP-1. Vildagliptin improves glycemic control in type 2 diabetic patients either as a monotherapy or administered in combination with metformin, sulfonylurea, thiazolidinedione or insulin [11-14]. Improvements in glycemic control are mediated primarily by increased insulin secretion and the suppression of glucagon secretion. Both of these effects depend on plasma glucose concentration, indicating that insulin secretion is suppressed and glucagon secretion is stimulated under low-blood glucose conditions. Vildagliptin has not demonstrated any effects on body weight and does not evoke severe hypoglycemia.
Sulfonylurea is a potent oral hypoglycemic agent and is commonly prescribed as a monotherapy or as a component of combination therapy for the treatment of type 2 diabetic patients over 60 years of age [15,16]. Although sulfonylurea is well-known as being effective in lowering blood glucose, it also induces body weight gain and severe hypoglycemia.
In the present study, the efficacy and safety of vildagliptin-metformin treatment compared to those of glimepiride-metformin treatment were evaluated over 32 weeks in type 2 diabetic patients.
The present study was randomized, open-label and comparative. Patients who attended the outpatient diabetic clinic of Chungbuk National University Hospital were included, and exclusion criteria were evaluated during screening (week -2, visit 1). Type 2 diabetic patients with HbA1c levels greater than 7.0% who were naïve or were receiving monotherapy with oral hypoglycemic agents such as glimepiride (2 to 4 mg) or metformin (500 to 1,000 mg) for less than six months prior to the visit were eligible to participate in the present study. All the patients who received previous medications had to undergo a wash-out period of at least two weeks. Patients with a history of diabetic ketoacidosis, clinically significant liver or renal disease, congestive heart failure requiring pharmacological treatment, coronary artery percutaneous intervention or unstable angina within the past six months, and those over 80 years of age were excluded from the present study. Any of the following laboratory abnormalities at screening also precluded participation: serum creatinine >133 µmol/L, alanine aminotransferase or aspartate aminotransferase >3 times the upper limit of normal and total bilirubin >34 µmol/L.
All patients provided written informed consent prior to participation in the present study. The study protocol was reviewed and approved by the Institutional Review Board of Chungbuk National University Hospital. Eligible patients were assigned randomly at a 1:1 ratio at baseline (day 0) to receive either 50 mg of vildagliptin twice daily or 2 mg glimepiride twice daily in addition to 500 mg of metformin twice daily for 32 weeks. During the follow-up period, glimepiride-metformin treatment was down-titrated in cases of recurrent hypoglycemia.
Assessments included overnight fasting plasma glucose (FPG), 2-hour postprandial glucose (2-h PPG), HbA1c, fasting insulin, fasting C-peptide, body weight, and vital signs at each scheduled visit (week 0, 4, 12, 24, and 32). Homeostasis model assessment of β-cell (HOMA-β) and homeostasis model assessment of insulin resistance (HOMA-IR) were evaluated to assess pancreatic β-cell function and changes in insulin resistance, respectively. The primary efficacy endpoint was a change in HbA1c from baseline at week 32. Secondary efficacy endpoints included FPG or 2-h PPG reduction from baseline, as well as HbA1c responder rate and HbA1c reduction according to baseline HbA1c category. All adverse events and tolerability values were monitored throughout the study. Hypoglycemia was defined as a finger stick glucose concentration of less than 3.9 mmol/L without loss of consciousness. Severe hypoglycemia was defined in the patients with transient dysfunction of the central nervous system who were unable to treat themselves.
Vildagliptin was regarded as comparable to glimepiride if the upper boundary of the two-sided 90% confidence interval around the between-group difference in HbA1c was less than the predefined margin, δ=0.3%. The data were expressed as mean±standard deviation. All statistical tests were performed using the SPSS version 12.0 software package (SPSS Inc., Chicago, IL, USA). The means and frequencies of variables were evaluated using Student's t-test and the χ2 test, respectively. All P values less than 0.05 were regarded as statistically significant.
The present study randomly enrolled 106 patients (52 patients in glimepiride-metformin group and 54 patients in vildagliptin-metformin group). One patient in the glimepiride-metformin group and three patients in the vildagliptin-metformin group were eliminated from the study in the first four weeks due to recurrent hypoglycemia or intolerable gastrointestinal (GI) trouble, respectively. Finally, 51 patients (94.4%) in the vildagliptin-metformin group and 51 patients (98%) in the glimepiride-metformin group completed 32 weeks of treatment. The patients who discontinued medication due to adverse events were not included in the final analysis. The final analyzed patients consisted of 66 males and 36 females, with a mean age of 54 years and an average duration of diabetes of 5.9 years.
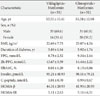
The groups were balanced at baseline with a mean HbA1c of 8.01 vs. 8.13% and FPG of 8.78 vs. 9.34 mmol/L. Table 1 summarizes the baseline demographic and clinical characteristics of the patients.
Mean FPG±standard deviation was decreased from 8.78±2.32 mmol/L at baseline to 7.24±1.64 mmol/L at week 32 in the vildagliptin-metformin group and from 9.34±2.14 mmol/L to 7.18±1.91 mmol/L in the glimepiride-metformin group. The reductions in FPG level were comparable between treatment groups (vildagliptin-metformin 1.54±2.41 mmol/L vs. glimepiride-metformin 2.16±2.51 mmol/L, P=0.508; Fig. 1A). Both treatments showed similar efficacy with regard to the 2h-PPG level; the reduction was 3.53±4.11 mmol/L (from 13.67±3.59 to 10.14±3.46) in the vildagliptin-metformin group and 3.72±4.17 mmol/L (from 14.44±2.22 to 10.72±3.36, P=0.950) in the glimepiride-metformin group (Fig. 1A).
The mean HbA1c was decreased from 8.01 to 7.07 (1.21% to 0.81%) in the vildagliptin-metformin group and from 8.13 to 7.13 (0.86% to 0.81%) in the glimepiride-metformin group; the decrements in HbA1c were also comparable between groups (vildagliptin-metformin 1.15 (-0.94%) and glimepiride-metformin 1.32 (-1.00%), P=0.855; Fig. 1B).
At week 12, when HbA1c was measured first after the initiation of the study, HbA1c was significantly decreased from baseline; the decrements in HbA1c did not differ appreciably between the treatment groups. Additionally, HbA1c remained stable until the endpoint at week 32 (Fig. 1C).
The proportions of patients who achieved an HbA1c less than 7% at the endpoint were also similar in the vildagliptin-metformin (50.1%) and glimepiride-metformin (56%) treatment group. In the subgroup analysis of baseline HbA1c category, both treatments showed similar HbA1c reduction efficiencies in all categories: greater reductions in HbA1c were noted in patients with higher baseline HbA1c concentrations (Fig. 2). The difference between the responders vs. non-responders was assessed, but no differences were observed between the two groups, with the exception of glucose and HbA1c levels.
Baseline fasting insulin, C-peptide, HOMA-β, and HOMA-IR were similar in the vildagliptin-metformin and glimepiride-metformin groups. During the treatment period, the changes in HOMA-β and HOMA-IR were comparable between the two groups (Table 2).
Mean body weight at baseline was 66.2±7.8 kg and 69.7±10.2 kg in the glimepiride-metformin and vildagliptin-metformin groups, respectively. At week 32, significant weight gain was observed in the glimepiride-metformin group (2.35±1.21 kg) compared to that in the vildagliptin-metformin group (0.23±0.69 kg) (P<0.05).
The overall incidence of hypoglycemia was 10-fold higher in patients treated with the glimepiride-metformin combination (ten patients vs. one patient in the vildagliptin-metformin group, P<0.05; Table 3) even though one patient in the glimepiride-metformin group was excluded from the study within the first four weeks of enrollment due to severe hypoglycemia. A majority of the patients had hypoglycemia that did not require medical assistance, although one patient who received glimepiride-metformin required medical assistance due to loss of consciousness. No severe hypoglycemia occurred in any of the patients taking vildagliptin-metformin.
The frequent adverse events in the vildagliptin-metformin group were GI events such as nausea, vomiting and diarrhea. Three patients in the vildagliptin-metformin group discontinued taking the medication due to intolerable GI problems within the first four weeks (Table 3). No meaningful changes were observed in the hematologic, biochemical or urinary analysis of vital signs, nor were any significant increases in liver function or muscle enzyme values observed in either group.
In the present study, the vildagliptin-metformin treatment showed an HbA1c reduction comparable to that of the glimepiride-metformin treatment over a 32-week period. The proportions of patients who achieved an HbA1c of less than 7.0% and HbA1c reduction according to the baseline HbA1c category were similar between treatments. Furthermore, vildagliptin-metformin treatment did not evoke weight gain and provided definite advantages in terms of hypoglycemia incidence reduction.
Regarding safety, the vildagliptin-metformin treatment had a favorable hypoglycemic profile: a 10-fold lower incidence of hypoglycemia, with no severe hypoglycemia observed. Several papers have recently been published regarding the association between hypoglycemia and adverse clinical outcome [9,11]. In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, intensive blood glucose control did not produce any benefits with regard to CV events but did provoke unanticipated excess mortality: 19 of the 41 deaths were attributed to unexpected CV disease, which may have been related to severe hypoglycemia [5].
In another trial, the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE), severe hypoglycemia was strongly associated with increased risks of adverse clinical outcomes. During the follow-up period, severe hypoglycemia was associated with a significant increase in the adjusted risks of major macrovascular events (hazard ratio [HR], 2.88), major microvascular events (HR, 1.81), death from a CV cause (HR, 2.68), and death from any cause (HR, 2.69; P<0.001 for all comparisons) [17]. The results of these analyses showed that the previous severe hypoglycemia occurrence was likely to constitute a marker of vulnerability to a primary CV event or death regardless of the treatment arm. Considering the potential CV risk associated with severe hypoglycemia, the use of medications associated with a low risk of hypoglycemia for the control and management of blood glucose in patients with type 2 diabetes would be prudent. Three patients in the vildagliptin-metformin treatment group discontinued taking medication in the first four weeks due to intolerable GI side effects, but these effects were likely attributed to metformin rather than vildagliptin since the GI side effects in the patients disappeared after vildagliptin monotherapy. Several patients in both treatments complained of GI side effects such as metallic taste, reduced appetite, or dyspepsia. However, the majority of GI symptoms disappeared over time in both treatment groups, and the patients who complained of GI troubles in the initial period of treatment eventually grew tolerant of the medications. DPP-4 inhibitors increase endogenous GLP-1 levels via inhibition of the DPP-4 enzyme. Increased GLP-1 can physiologically inhibit the satiety center in the brain, reduce appetite, and delay stomach emptying [18]. Vildagliptin-metformin treatment has a greater potential to evoke GI side effects compared to glimepiride-metformin treatment in terms of the relevant pharmacological mechanisms, although previous studies did not show any further increase in GI side effects between metformin monotherapy and metformin-vildagliptin combination therapy [19,20]. Although there is no current obvious explanation why only patients in the vildagliptin-metformin treatment group experienced intolerable GI trouble, initiating vildagliptin treatment with a low-dose of metformin in order to ameliorate the GI side effects is advisable.
In the present study, changes in body weight differed between the treatment groups. At 32 weeks, body weight was unchanged in the vildagliptin-metformin treatment group, whereas the patients treated with glimepiride-metformin evidenced weight increase (2.35 kg) relative to baseline. The results were consistent with findings reported in other studies involving vildagliptin or sitagliptin in combination with metformin [21,22]. In another study comparing the efficacies of vildagliptin and glimepiride in combination with metformin, Matthews et al. [22] reported results similar to the present study. In the 52-week follow-up period in that previous study, an HbA1c reduction of -0.44% was reported in the vildagliptin group and a -0.53% reduction in the glimepiride group. DPP-4 inhibitors have been shown to improve glycemic control and measures of pancreatic β-cell function in clinical trials in the Asian population, including patients from China, India, and Korea [23]. Deterioration in the early insulin responses is frequently observed in patients with type 2 diabetes, particularly in the Asian population. DPP-4 inhibitors improved pancreatic β-cell dysfunction and may be associated with more improved responses in Asian than in Caucasian patients [24].
In terms of safety profiles, decreased weight gain and low incidence of hypoglycemia were also observed in the vildagliptin treatment group [23]. In the extended two-year observation period in the previous study, the vildagliptin-metformin combination treatment group still evidenced similar glucose control and better safety profiles [22]. When considering the different patient characteristics, the body mass indexes of the study populations were different between our study and that of Dejager (22 to 23 vs. 31 to 32, respectively); therefore, the vildagliptin-metformin combination treatment can be considered as comparable to the glimepiride-metformin combination treatment in both non-obese and obese type 2 diabetic patients. A previous one-year study [19] comparing the efficacies of sitagliptin or glipizide in combination with metformin showed similar results to those observed in the present study, demonstrating comparable efficacy, less weight gain and lower risk of hypoglycemia with sitagliptin. Collectively, the results indicate that DPP-4 inhibitors added to metformin may represent a more effective combination in type 2 diabetic patients with unfavorable glucose control in monotherapy.
In terms of the incidence of CV events in association with vildagliptin or glimepiride treatments, Dejager's study reported that fewer patients treated with a vildagliptin-metformin combination after 52 weeks of treatment experienced CV events confirmed by the adjudication committee (0.9%) than were observed in the patients treated with a glimepiride-metformin combination (1.6%) [22,23,25]. Although additional long-term studies of CV events in association with DPP-4 inhibitors are warranted, the findings from the present study suggest that a vildagliptin-metformin combination treatment may constitute an effective alternative therapeutic option for type 2 diabetic patients, with relative confidence regarding the initiation of CV disease.
Although the present study had several limitations in terms of the small number of participants and its status as an open-label study without blinding, the results demonstrated that vildagliptin-metformin combination treatment offered comparable efficacy in terms of HbA1c reduction, no weight gain, and a lower risk of hypoglycemia in type 2 diabetic patients with unfavorable blood glucose control. When safety is considered along with effectiveness, the vildagliptin-metformin combination treatment may constitute a better therapeutic option than does the glimepiride-metformin combination treatment.
Figures and Tables
Fig. 1
(A) Mean fasting plasma glucose (FPG) and 2-hour post-prandial glucose (2h-PPG) reduction in vildagliptin or glimepiride treatment. (B) Decrement of HbA1c on the week 32 end-point in vildagliptin or glimepiride treatment. (C) Mean HbA1c changes during 32 weeks in vildagliptin or glimepiride treatment.

ACKNOWLEDGMENTS
This work was supported by a research grant from Chungbuk National University in 2009.
References
1. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998. 352:837–853.
2. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008. 359:1577–1589.
3. Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med. 1993. 328:1676–1685.
4. Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005. 353:2643–2653.
5. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008. 358:2545–2559.
6. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008. 358:2560–2572.
7. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD. VADT Investigators. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009. 360:129–139.
8. Gavin JR 3rd, Bohannon NJ. A review of the response to oral antidiabetes agents in patients with type 2 diabetes. Postgrad Med. 2010. 122:43–51.
9. Palalau AI, Tahrani AA, Piya MK, Barnett AH. DPP-4 inhibitors in clinical practice. Postgrad Med. 2009. 121:70–100.
10. Kulasa KM, Henry RR. Pharmacotherapy of hyperglycemia. Expert Opin Pharmacother. 2009. 10:2415–2432.
11. Rosenstock J, Fitchet M. Vildagliptin: clinical trials programme in monotherapy and combination therapy for type 2 diabetes. Int J Clin Pract Suppl. 2008. (159):15–23.
12. Bolli G, Dotta F, Rochotte E, Cohen SE. Efficacy and tolerability of vildagliptin vs. pioglitazone when added to metformin: a 24-week, randomized, double-blind study. Diabetes Obes Metab. 2008. 10:82–90.
13. Fonseca V, Baron M, Shao Q, Dejager S. Sustained efficacy and reduced hypoglycemia during one year of treatment with vildagliptin added to insulin in patients with type 2 diabetes mellitus. Horm Metab Res. 2008. 40:427–430.
14. Garber AJ, Foley JE, Banerji MA, Ebeling P, Gudbjornsdottir S, Camisasca RP, Couturier A, Baron MA. Effects of vildagliptin on glucose control in patients with type 2 diabetes inadequately controlled with a sulphonylurea. Diabetes Obes Metab. 2008. 10:1047–1056.
15. Rodriguez A, Cipres L, Tofe S, Polavieja P, Reviriego J. Clinical evaluation of combined therapy for type 2 diabetes. Curr Med Res Opin. 2010. 26:1171–1183.
16. Pareek A, Chandurkar N, Zawar S, Agrawal N. Evaluation of efficacy and tolerability of gliclazide and metformin combination: a multicentric study in patients with type 2 diabetes mellitus uncontrolled on monotherapy with sulfonylurea or metformin. Am J Ther. 2010. 17:559–565.
17. Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S. ADVANCE Collaborative Group. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010. 363:1410–1418.
18. Wiedeman PE, Trevillyan JM. Dipeptidyl peptidase IV inhibitors for the treatment of impaired glucose tolerance and type 2 diabetes. Curr Opin Investig Drugs. 2003. 4:412–420.
19. Nauck MA, Meininger G, Sheng D, Terranella L, Stein PP. Sitagliptin Study 024 Group. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trial. Diabetes Obes Metab. 2007. 9:194–205.
20. DeFronzo RA. Current issues in the treatment of type 2 diabetes. Overview of newer agents: where treatment is going. Am J Med. 2010. 123:3 Suppl. S38–S48.
21. Ferrannini E, Fonseca V, Zinman B, Matthews D, Ahren B, Byiers S, Shao Q, Dejager S. Fifty-two-week efficacy and safety of vildagliptin vs. glimepiride in patients with type 2 diabetes mellitus inadequately controlled on metformin monotherapy. Diabetes Obes Metab. 2009. 11:157–166.
22. Matthews DR, Dejager S, Ahren B, Fonseca V, Ferrannini E, Couturier A, Foley JE, Zinman B. Vildagliptin add-on to metformin produces similar efficacy and reduced hypoglycaemic risk compared with glimepiride, with no weight gain: results from a 2-year study. Diabetes Obes Metab. 2010. 12:780–789.
23. Dejager S, Razac S, Foley JE, Schweizer A. Vildagliptin in drug-naive patients with type 2 diabetes: a 24-week, double-blind, randomized, placebo-controlled, multiple-dose study. Horm Metab Res. 2007. 39:218–223.
24. Mohan V, Yang W, Son HY, Xu L, Noble L, Langdon RB, Amatruda JM, Stein PP, Kaufman KD. Efficacy and safety of sitagliptin in the treatment of patients with type 2 diabetes in China, India, and Korea. Diabetes Res Clin Pract. 2009. 83:106–116.
25. Matsumoto K, Miyake S, Yano M, Ueki Y, Yamaguchi Y, Akazawa S, Tominaga Y. Glucose tolerance, insulin secretion, and insulin sensitivity in nonobese and obese Japanese subjects. Diabetes Care. 1997. 20:1562–1568.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download