Abstract
Background and Objectives
Subjects and Methods
Results
Conclusion
Figures and Tables
Fig. 1
Measurement of LVEDP and pre-aLVDP. The pre-aLVDP is measured at the onset of the a-wave, and the measurement of LVEDP is made at the nadir of the atrial contraction wave before the onset of a rapid rise in left ventricular (LV) systolic pressure or at the peak of R-wave on EKG. LVEDP: left ventricular end-diastolic pressure, pre-aLVDP: pre-a left ventricular diastolic pressure, LV: left ventricle, EKG: electrocardiography, P: P wave, QRS: QRS complex, LVSBP: left ventricle systolic blood pressure, LVDBP: left ventricle diastolic blood pressure.

Fig. 2
Association of the invasively measured LVEDPs between the echocardiographic e/e' ratios during leg-raise. Leg-raise, especially active leg-raise, significantly increases all types of LVEDP parameters. Unlike the invasively measured LVEDP, the septal e/e' ratio is not significantly changed during passive and active leg-raise. "p" indicates passive leg-raise, "a" active leg-raise, and "R" recovery period. For example, p30 is at 30-second passive leg-raise. *p<0.05 vs. baseline at passive stage, †p<0.01 vs. at a0. LVEDP: left ventricular end-diastolic pressure.
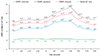
Fig. 3
Time course of the invasively measured LVEDP according to the LVEDP response to leg-raise. In most of the patients (77.9%), LVEDP increased steadily throughout active leg-raise. In contrast, LVEDP in 22.1% of the patients increased moderately during the early stage of active leg-raise and then declined during the late stage, relative to the initial stage. "p" indicates passive leg-raise, "a" active leg-raise, and "R" recovery period. For example, p30 is at 30-second passive leg-raise. *p<0.05 vs. baseline at passive stage, †p%0.01 vs. at a0, ‡p<0.01 vs. ΔLVEDP_frequent>0 mmHg. LVEDP: left ventricular end-diastolic pressure.

Fig. 4
Time course of septal e/e' ratio according to the LVEDP response to leg-raise. Septal e/e' ratios in the ΔLVEDP_frequent≤0 mmHg group were significantly lower at initial, passive, and active stages, as compared with those in the ΔLVEDP_frequent>0 mmHg group. However, septal e/e' ratio showed no significant change during active leg-raise. "p" indicates passive leg-raise, "a" active leg-raise, and "R" recovery period. For example, p30 is at 30-second passive leg-raise. *p<0.05 vs. baseline at passive stage. †p<0.01 vs. at a0, ‡p<0.05 vs. LVEDP of ΔLVEDP_frequent>0 mmHg, §p<0.05 vs. e/e' ratio of ΔLVEDP_frequent>0 mmHg. LVEDP: left ventricular end-diastolic pressure.
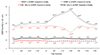
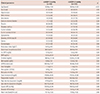
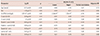
Table 2
Effect of leg-raise exercise on LV hemodynamic parameters

Active leg-raise leads to a significant increase in the value of LV hemodynamic parameters, whereas passive leg raise results in no significant change. *p<0.05 vs. baseline at passive leg-raise, †p<0.05 vs. initial point at active leg-raise. LV: left ventricular, LVSBP: left ventricular systolic blood pressure, LVDBP: left ventricular diastolic blood pressure, LVEDP: left ventricular end-diastolic pressure, pre-aLVDP: pre-a left ventricular diastolic pressure
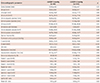
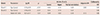
Table 3
Comparison of LV hemodynamic parameters according to the LVEDP response to leg-raise exercise

Table 4
Comparison of clinical characteristics according to the LVEDP response to leg-raise exercise
Data are expressed as number (%) or mean±standard deviation. LVEDP: left ventricular end-diastolic pressure, RAA: renin-angiotensin-aldosterone, NYHA: New York Heart Association, hs-CRP: high sensitivity C-reactive protein, BNP: brain natriuretic peptide, eGFR: estimated glomerular filtration rate, BP: blood pressure
Table 5
Comparison of echocardiographic parameters according to the LVEDP response to leg-raise exercise




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download