Abstract
Background and Objectives
Subjects and Methods
Results
Figures and Tables
Fig. 1
Study flow chart. 1Left ventricular ejection fraction <30% or 30-35% with sustained ventricular tachycardia and/or ventricular fibrillation on electrophysiologic study, 2Patients who were resuscitated from sudden cardiac death with decreased left ventricular systolic function.

Fig. 2
Cumulative probability of the first appropriate implantable defibrillator therapy. (A) shows the shock therapy delivered in all patients, and (B) shows comparison of the shock therapy according to the indication in patients that underwent a device implantation (log rank p=0.015).

Fig. 3
Time-dependence of the first appropriate implantable defibrillator therapy. “Patients entering” refers to the number of patients without appropriate implantable defibrillator therapies for ventricular tachyarrhythmia being followed at the beginning of each time interval. ICD: implantable cardioverter/defibrillator.

Fig. 4
Comparison of cumulative survival rate according to the indication, the etiology, and the type of shock therapy by Kaplan-Meier plots. (A) shows total cumulative survival rate in all patients. (B) shows cumulative survival rate according to the indication in patients that underwent a device implantation (p=0.626). (C) shows cumulative survival rate according to the etiology in patients who underwent a device implantation (p=0.316). (D) shows cumulative survival rate according to the type of shock therapy in patients who underwent a device implantation (p=0.816). CMP: cardiomyopathy.

Table 1
Baseline clinical characteristics of the study patients categorized by the etiology

Data are expressed as mean±standard deviation or number (%). CMP: cardiomyopathy, BMI: body mass index, MI: myocardial infarction, HF: heart failure, Tachy-arrest: cardiac arrest by tachyarrhythmia, Brady-arrest: cardiac arrest by bradyarrhythmia, LVESD: left ventricular end-systolic dimension, LVEDD: left ventricular end-diastolic dimension, LVEF: left ventricular election fraction, ICD: implantable cardioverter/defibrillator, CRT-D: cardiac resynchronization therapy with defibrillator
Table 2
Baseline clinical characteristics of the study patients categorized by the indication for the device implantation

Data are expressed as mean±standard deviation or number (%). BMI: body mass index, MI: myocardial infarction, HF: heart failure, Tachy-arrest: cardiac arrest by tachyarrhythmia, Brady-arrest: cardiac arrest by bradyarrhythmia, LVEDD: left ventricular end-diastolic dimension, LVESD: left ventricular end-systolic dimension, LVEF: left ventricular election fraction, ICD: implantable cardioverter/defibrillator, CRT-D: cardiac resynchronization therapy with defibrillator
Table 3
Rate of shock therapies and the clinical outcomes in the patients according to the etiology

Table 4
Rate of shock therapies and the clinical outcomes in the patients according to the indication for the device implantation

Table 5
Comparison of the shock therapy according to the device category
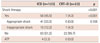
| ICD (n=123) | CRT–D (n=23) | p | |
|---|---|---|---|
| Shock therapy | <0.001 | ||
| Yes | 56 (45.5) | 1 (4.3) | <0.001 |
| Appropriate shock | 41 (33.3) | 0 (0.0) | 0.106 |
| Inappropriate shock | 15 (12.2) | 1 (4.3) | |
| No | 63 (51.2) | 22 (95.7) | |
| ATP | 4 (3.3) | 0 (0.0) |
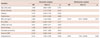
Table 6
Variables associated with all-cause death




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download