Abstract
Background and Objectives
The purpose of this study was to estimate the prevalence, awareness and treatment of high low density lipoprotein-cholesterol (LDL-C) level in Korean adults without coronary heart disease.
Subjects and Methods
National representative cross-sectional surveys, data of 5248 Korean adults (2246 men and 3002 women) aged between 20 and 79 years from the Third Korea National Health and Nutrition Examination Survey (KNHANES III, 2005) was used. High LDL-C level was defined with the risk prediction algorithm published by the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III).
Results
The prevalence of the Korean adults with high LDL-C level who need therapeutic lifestyle changes was 19.9%, treatment with lipid-lowing medication was 2.1% and awareness of this condition was 7.9%. Meanwhile, the prevalence of the Korean with very high LDL-C level who should be considered for drug therapy was 13.5%, treatment with lipid-lowing medication was 2.7% and awareness of this condition was 8.1%. Overall, 47.9% (60.3% in male and 39.1% in female) of participants had a single lipid disorder (high LDL-C, high triglycerides: ≥200 mg/dL, low high density lipoprotein-cholesterol: <40 mg/dL), whereas 15.5% (23.5% in male and 9.7% in female) had at least two. Only 1.9% (2.8% in male and 1.2% in female) of all participants had all three lipid abnormalities as defined.
Dyslipidemia is considered as a major risk factor of cardiovascular disease (CVD), such as hypertension, diabetes mellitus, myocardial infarction, and stroke.1-6) Recently, the Third Korea National Health and Nutrition Examination Survey (KNHANES III, 2005) data showed that the prevalence of dyslipidemia has increased from 32.4% in 1998 to 44.1% in adults.5)
Dyslipidemia can be classified into hypercholesterolemia, hypertriglycemia, low high density lipoprotein-cholesterol (HDL-C) and high low density lipoprotein-cholesterol (LDL-C). Dyslipidemia has been proven one of major risk factors of CVD in many studies, including Framingham Heart Study.7-9) It is shown that the morbidity and mortality of coronary heart disease (CHD) can be decreased by lowering blood cholesterol level. By with the treatment of hypercholesterolemia, CHD mortality can be reduced by 20 to 24%.7)8)10)
Managing dyslipidemia is known to have a great effect in preventing the development of CHD and their complications. National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) provided clinicians with guidelines in the diagnosis and treatment of high blood cholesterol.
The NCEP ATP III guidelines classify patients into CHD risk categories, based on the presence of CHD, risk equivalents of CHD and multiple risk factors according to LDL-C level, to determine their 10-year CHD risk distribution.11) Recently, the Guideline committee of the Korean Society of Lipidology and Atherosclerosis published the modification of the second edition of its dyslipidemia treatment guideline for Koreans.12) This treatment guideline is somewhat similar to the NCEP ATP III guideline, although lipid levels in Korean are lower than those of western population.
In Korea, the prevalence of dyslipidemia has been on the increasing tendency continuously: it is higher in male (54.5%) than female (34.0%) across all age groups, and low HDL-C and hypercholesterolemia were the dominant subtype of dyslipidemia in Korea.5)13) The KNHANES reported a treatment rate was only 6.8%, and 33.3% of patients reached treatment target in patients over 20 years of age with high LDL-C level (LDL-C ≥160 mg/dL).5)
The problem with dyslipidemia control is the 'treatment gap' phenomenon-meaning failure to adhere to the recommendations outlined in established treatment guideline.14)16)17) Overcoming this 'treatment gap' is a crucial part to prevent CVD and improve its prognosis. For this reason, the United States has already been working to decrease the 'treatment gap' and to apply treatment guideline in clinical practice.14-17)
There are many reports on the 'treatment gap' in Korea, raising arguments on their representativeness because most studies are carried out in subjects who visited hospitals and clinics.17-19) This study was designed to analyze lipid levels according to CHD risk categories, and to investigate awareness and treatment rate of high LDL-C level in Korean adults without history of CHD using KNHANES in 2005.
Our research was based on data obtained in the KNHANES III, a cross-sectional health survey of nationally representative samples of Koreans. The KNHANES was conducted in 2005 by the Korea Centers for Disease Control and Prevention. The target population for this survey was non-institutionalized individuals. The total population was 34145 for the purpose of primary sampling. Subjects were randomly sampled throughout South Korea, and included in the Health Interview Survey. From the total sample population, 7597 individuals completed the Health Examination Survey. In total, 5352 individuals aged between the age of 20 and 79 constituted the study population. Subjects diagnosed with CHD and those without measurement of lipid levels were excluded. The final number of study subjects for the Korean dyslipidemia analysis was 5248 (2246 male and 3002 female).
Diabetes mellitus was defined as fasting blood glucose level above 126 mg/dL, and/or treatment with insulin or oral antidiabetic medications, and/or being diagnosed with diabetes mellitus by a doctor. Hypertension was defined as systolic blood pressure (SBP) over 140 mm Hg and/or diastolic blood pressure (DBP) over 90 mm Hg, and/or use of antihypertensive medications and/or diagnosed with hypertension by a doctor. Smoking status was classified as either currently smoking or non-smoking. Current smokers are defined as those who smoked more than 100 cigarettes in the past year. Non-smokers are those who do not smoke currently and those who smoked less than 100 cigarettes in the past year.
Blood pressure was measured by trained investigator using standardized technique.
Cuff size fitting arm circumference was chosen and the subject was sat in a chair a with back rest for 5 minutes to relax before blood pressure was measured three times with a Baumanometer to obtain the average pressure. When blood pressure was only measured twice, average SBP and DBP from two measurements were used. Blood was collected from the vein following an 8-hour fasting state; serum was separated and stored in refrigerated conditions. Samples were transported on the same day to the central institute for analyses within 24 hours. Fasting blood glucose, total cholesterol (TC), HDL-C and triglyceride (TG) were analyzed using a Hitachi 747 auto-analyzer (Tokyo, Japan). LDL-C was calculated using the Friedewald formula, [LDL-C (mg/dL)=TC (mg/dL)-{HDL-C (mg/dL)+TG (mg/dL)/5}] for those with TG level below 400 mg/dL.20)
High LDL-C was classified according to the NCEP ATP III guidelines, taking into account the number of major CHD risk factors and Framingham point score.11) Age (male over 45, female over 55), hypertension, low HDL-C and current smoking status were defined as major CHD risk factors. The target LDL-C level was set according to NCEP ATP III.11) In this study, subjects were divided into two groups by target LDL-C: one group in need of therapeutic lifestyle change (TLC) and the other in need of drug therapy (Table 1).
The awareness and treatment rates of high LDL-C were defined as follows: awareness rate was investigated by a survey asking for disease and diagnosis history among high LDL-C population, including previously diagnosed patients and newly diagnosed patient of dyslipidemia. Treatment rate was investigated by a survey asking whether or not they had been taking oral lipid lowering agents.
All data was analyzed using Statistical Package for the Social Sciences (SPSS) version 12.0 (SPSS, Inc., Chicago, IL, USA) and p<0.05 was considered statistically significant. Continuous variables are expressed in mean±standard deviation, and discrete variables are expressed in numbers and proportions. Differences in categorical data were analyzed using the Chi-square test.
The general characteristics of the study population are shown in Table 2. The mean age of the subjects for male and female was 46.5 years and 46.1 years, respectively. Both male and female showed the highest distribution in the 40-49 age group (male 26.4%, female 24.6%). SBP and DBP were higher in male subjects than in female. The prevalence of CHD risk factors-hypertension, diabetes and current smoking was significantly higher in male than in female subjects.
Distribution of lipid levels according to study subjects and age groups are shown in Table 3 and Fig. 1. TC level did not significantly differ by gender, but LDL-C level was higher in female. Distribution of TC and LDL-C levels did not differ significantly by gender. Mean HDL-C level was significantly lower in male (42.4 mg/dL) than in female (47.3 mg/dL), and those with HDL-C levels lower than 40 mg/dL were significantly more in male. Mean TG level was significantly higher in male than in female, and subjects with higher TG level than 200 mg/dL were twice as many in male (22.4%) as in female (9.6%) (p<0.001).
According to lipid levels by age group, high TC (TC ≥240 mg/dL) and high LDL-C (LDL-C ≥160 mg/dL) in male increased until 40-49 years and then decreased after 50 year of age. However, female showed continuous increase until 50-59 years of age and then decreased. High TG (TG ≥200 mg/dL) in male increased until 40-49 years and then decreased after 50 years of age. However, female increased until 50 years old but the levels stabilized after 50s. Low HDL-C (HDL-C <40 mg/dL) in male didn't differ significantly by age groups, but female showed continuous increase with age.
Subject distribution in need of TLC and drug therapy by risk categories in regard to LDL-C level is shown in Table 4. Among Koreans over 20 years old without history of CHD, 9.8% had risks equivalent to CHD, 29.5% had more than two risk factors and 60.7% had less than two risk factors. Among 483 subjects with CHD-equivalent risks and/or a 10-year CHD risk of >20%, 359 subjects (74.3%) showed LDL-C levels higher than 100 mg/dL in need of TLC and 74.3% was in need of drug therapy with LDL-C levels over 100 mg/dL. Among 1454 subjects with two or more CHD risk factors and a 10-year CHD risk of ≤20%, 31.0% was in need of TLC with LDL-C levels over 130 mg/dL, and 18.9% was in need of drug therapy. Among subjects with 0-1 CHD risk factors, 5.8% was in need of TLC with LDL-C levels higher than 160 mg/dL and 1.0% was in need of drug therapy. Ratio of patients in need of aggressive treatment was the highest in the group with CHD equivalent risk. 13.5% of the study population needed drug treatment.
Subjects with more than one lipid disorder were higher in male when the proportion of subjects with combined high LDL-C, high TG and low HDL-C was analyzed (Fig. 2). 60.3% of male had ≥1 lipid disorder among high LDL-C, high TG and low HDL-C, 23.5% had ≥2 lipid disorders and 2.8% had all three lipid abnormalities. 39.1% of female had ≥1 lipid disorder, 9.7% had ≥2 and 1.2% had all three types of dyslipidemia.
The awareness and treatment rates of high LDL-C level are shown in Table 5. In 984 (19.9%) high LDL-C subjects, the awareness rate was 7.9% (male 7.3%, female 8.5%) and the treatment rate was 2.1% (male 1.2%, female 3.0%). The awareness and treatment rates of high LDL-C level were the highest in the 60-69 age group for both genders. The awareness rate in high LDL-C subjects who required drug therapy was 8.1% (male 7.2%, female 9.5%) and the treatment rate was 2.7% (male 1.5%, female 4.4%). The awareness and treatment rates in both male and female continuously increased from 20-29 to 60-69 years and then decreased from 70-79 years. Female showed higher awareness and treatment rates than male. When the results were analyzed by NCEP ATP III risk categories in regard to LDL-C level, both male and female with 0-1 CHD risk factor showed the lowest awareness and treatment rates. However, the awareness and treatment rates were still less than 8% in the group with CHD equivalent risks.
Recently, cerebrovascular and cardiac diseases were respectively the second and third cause of death, therefore CVD account for 20% of overall death in Korea.21) This study was designed to analyze the distribution of dyslipidemia, the prevalence of high LDL-C level according to the NCEP ATP III criteria and to make useful suggestions that can lead to effective control strategies for high LDL-C level in the Korean population using NHANES in 2005.
The prevalence of hypertension in our study population was 25.9%, which was slightly lower than the outcome of 28.5% in a study conducted in adults, including CHD patients, over 20 years of age in the United States. However, the prevalence of diabetes (8.4% vs. 8.8%) and the rates of current smoking (22.6% vs. 23.6%) were similar.22) In our study, the prevalence of major CHD risk factors was also higher in male than female across all age group. Male demonstrated higher prevalence of hypertension (male 30.6%, female 22.3%), diabetes (male 10.7%, female 6.7%) and current smoking rate (male 47.7%, female 4.3%) than female. In addition, among the mean lipid levels, TG was higher in male (163.5±158.2 mg/dL) than female (114.0±78.1 mg/dL), however, LDL-C (male 113.0±30.4 mg/dL, female 114.7±30.0 mg/dL, p=0.043) and HDL-C (male 42.4±10.2 mg/dL, female 47.3±10.9 mg/dL, p<0.001) were lower in male than female.
Of the study subjects analyzed, 19.9% required TLC and 13.5% required drug therapy according to NCEP ATP III. These results were lower than that of 28.0% and 25.3% from the United States study conducted in adults aged over 20 years, including CHD patients.22)23) In the United States, among subjects in need of TLC and drug therapy by risk categories in regard to LDL-C level, there were a lot of subjects in need of TLC and drug therapy in groups with less than two CHD risk factors. However, in our study, those who needed TLC and drug therapy were highest in subjects with risks equivalent to CHD.22) This outcome indicates a lack of appropriate management of high LDL-C level in the high risk group. In another Korean study conducted in patients aged between 20 and 79 who visited the health promotion center of medical center in 2001, subjects in need of TLC and drug therapy were 12.1% and 6.1%, respectively, showing lower prevalence than this study.24) The reason for this appeared to be due to differences in the characteristics of study subjects. Our study has shown that subjects with high LDL-C level in need of TLC and drug therapy increased by age, and the prevalence of subjects in need of TLC and drug therapy were higher in female than in male (Table 5).
Based on 'Risk assessment chart of a 10-year cardiocerebrovascular disease in Korean's supplement of dyslipidemia guideline in Korean (2008 February edition)', the 10-year ischemic heart disease (IHD) risks were analyzed. No Korean population showed a 10-year IHD risk of >20%, but 363 subjects (11.6%) exhibited IHD equivalent risks, 7 subjects (0.2%) exhibited a 10-year IHD risk of 10-20% and 42.1% exhibited a 10-year IHD risk of <10%. 1441 subjects (46.0%) had less than two risk factors.
Risk estimation scoring system for the Korean population includes SBP, TC, age and current smoking. Except for HDL-C, these are identical to the risk factors outlined in Framingham risk score. However, SBP and TC range were different (range in Koreans: SBP 100-199 mm Hg, TC 160-279 mg/dL are defined) and age range was also different from Framingham risk score, which encompassed ages between 20-79 versus the Korean scoring system, which encompassed ages between 40-70. However, the risk estimation scoring system suggested by the Korean Society of Lipidology and Atherosclerosis should be validated and needs an agreement.
In our study, the proportion of dyslipidemia with combined high LDL-C, high TG and low HDL-C levels in all age groups was compared with that of adults in the United States and France: proportion of high LDL-C group was relatively low, and proportion of low HDL-C and proportion of high TG were relatively high. Apart from these results, lipid disorder comprised of low HDL-C and high TG showed high proportion.23)25) TG correlates negatively to HDL-C and this is caused by HDL-C effect on TG metabolism.26-28) Low HDL-C and high TG are known to be associated with type 2 diabetes and this is related to the Koreans' high carbohydrate diet and obesity.29)30) Bersot et al.31) reported that high TG being a risk factor of type 2 diabetes, acute pancreatitis as well as increased risk of CVD by two-fold. Thus overall management or control of dyslipidemia including high TG as well as high LDL-C and low HDL-C is thought to be crucial.
In the present study, the awareness and treatment rates of high LDL-C group in need of drug therapy was very low, at 8.1% and 2.7% respectively, and this study demonstrated significant difference between the awareness and treatment rates of hypertension in Korean. According to in-depth analysis of KNHANES in 2005, the hypertension awareness and treatment rate in adults over 20 years of age has increased respectively from 24.2% to 58.7% and from 17.0% to 45.7% between 1998 and 2005.5) Also, the political approaches to increase the awareness and treatment rates of high LDL-C level were insufficient compared to that of hypertension.
Since 1960, adherence to federal and state policies to lower TC and LDL-C level resulted in continuous decrease of LDL-C level in the United States, which resulted in decrease of death from CVD. However, Korea lacks the data to establish dyslipidemia guidelines. Currently, the health insurance system covers reimbursement when a patient meets the treatment criteria for dyslipidemia: TC over 250 mg/dL for the prevention of CVD, or TC over 220 mg/dL when risk factors such as IHD history, hypertension, and diabetes are present.32) Recently, LDL-C level is advised to be less than 100 mg/dL, but subjects with high risk may not be treated when the TC level is less than 220 mg/dL. Therefore, we need a change in policies based on evidence, in addition to continuing efforts to increase the low awareness and treatment rates with active education and regular health check-ups.
This study has several limitations. First, this study failed to provide awareness and treatment rate of high LDL-C level in patients with existing CHD because this study was only conducted for those without history of CHD. Since KNHANES uses the self-administered questionnaire to identify the CVD, it was hard to distinguish IHD from other heart diseases. Therefore, our study was proposed to provide guideline for primary prevention measures to those without history of CHD. Second, familial history of CHD (development or death from CHD of parents or siblings before age of 55) among major CHD risk factors by the NCEP ATP III guideline was not investigated. Health examination survey does not include CHD family history with the age of onset, therefore family history with CHD was excluded from the Framingham score analysis. Third, LDL-C level was calculated by the method of Friedewald formula,20) therefore this seem to be insufficiency to reflect the exact concentration.
In conclusion, 19.9% was in need of TLC and 13.5% was in need of drug therapy among Korean subjects without CHD according to NCEP ATP III guideline. The prevalence of high LDL-C was the highest in the group with risks equivalent to CHD. Only 8.1% of the high LDL-C group in need of drug therapy was aware of dyslipidemia and 2.7% of these subjects were on drug therapy, which indicate low awareness and treatment rates in our population. Continuous efforts are therefore needed to decrease the LDL-C levels in the high risk groups to prevent CVD.
Figures and Tables
Fig. 1
The prevalence of TC, LDL-C, HDL-C, and TG levels by age group. TC: total cholesterol, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, TG: triglyceride.

Fig. 2
Proportion of Korean adults with a combination of high LDL-C, high TG, and low HDL-C. High LDL-C: LDL-C ≥100 mg/dL for patients with coronary hear disease (CHD) risk equivalents, ≥130 mg/dL for patients with two or more CHD risk factors, ≥160 mg/dL for those with 0-1 CHD risk factor, High TG: ≥200 mg/dL, Low HDL-C: <40 mg/dL for men and women. LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, TG: triglyceride.

Table 1
LDL-C goals and cutpoints for therapeutic lifestyle changes and drug therapy in different risk categories11)
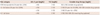
Table 4
Distribution of LDL-C for therapeutic lifestyle changes (TLC) and drug therapy in different risk categories by NCEP ATP III
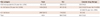
Table 5
Distribution of awareness of this diagnosis, and treatment by TLC or drug therapy with high LDL-C in Korean adults
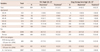
Values for awareness and treatment are n (%). *High LDL-C was defined patients for initiate therapeutic lifestyle change by NCEP ATP III, †Patients for drug therapy by NCEP ATP III, ‡Self-report of any prior diagnosis of dyslipidemia by a health-care professional, §Self-report current use of cholesterol lowering medication. LDL-C: low density lipoprotein-cholesterol, TLC: therapeutic lifestyle changes, CHD: coronary heart disease, NCEP ATP III: National Cholesterol Education Program Adult Treatment Panel III
Acknowledgments
The study was supported by an intramural grant of the National Institute of Health, Korea (4800-4845-300-210, 2007-N63001-00).
References
1. Wilson PWF, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998. 97:1837–1847.
2. Castelli WP. Epdemilology of coronary heart disease: the Framingstudy. Am J Med. 1984. 76:4–12.
3. Stamler J, Dyer AR, Shekelle RB, Neaton J, Stamler R. Relationship of baseline major risk factors to coronary and all-cause mortality, and to longevity: finding form long-term follow-up of Chicago cohorts. Cardiology. 1993. 82:191–222.
4. Stamler J, Daviglus ML, Garside DB, Dyer AR, Greenland P, Neaton JD. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA. 2000. 284:311–318.
5. In-Depth Analysis of the Third Korea National Health and Nutrition Examination Survey (KNHANES III). 2007. Seoul: Korea Centers for Disease Control and Prevention.
6. Lim S, Jang HC, Park HC, et al. Changes in metabolic syndrome of Korean children and adolescents in the period 1998 to 2001. J Endocrinol Invest. 2008. 31:327–333.
7. The Lipid Research Clinics Coronary Primary Prevention Trial. I. Reduction in incidence of coronary heart disease. JAMA. 1984. 251:351–364.
8. Castelli WP, Garrison RJ, Wilson PW, Abbott RD, Kalousidian S, Kannel WB. Incidence of coronary heart disease and lipoprotein cholesterol levels: the Framingham Study. JAMA. 1986. 256:2835–2838.
9. Frick MH, Elo O, Haapak M, et al. Helsinki Heart Study: primary prevention trial with gemfibrozil in middled-aged men with dyslipidemia: safety of treatment, changes in risk factors and incidence of coronary heart disease. N Engl J Med. 1987. 317:1237–1245.
10. The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984. 251:365–374.
11. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004. 110:227–239.
12. Committee of treatment guideline for hypercholesterolemia. Treatment guideline for hypercholesterolemia. 2008. 2nd ed. Seoul: Korea Society of lipidology and atherosclerosis.
13. Ko M, Kim MT, Nam JJ. Assessing risk factors of coronary heart disease and its risk prediction among Korean adults: the 2001 Korea National Health and Nutrition Examination Survey. Int J Cardiol. 2006. 110:184–190.
14. Siegel D. The gap between knowledge and practice in the treatment and prevention of cardiovascular disease. Prev Cardiol. 2000. 3:167–171.
15. Smaha LA. The American Heart Association get with the guidelines program. Am Heart J. 2004. 148:5 Suppl. S46–S48.
16. Sung J, Kim SH, Kim YD, et al. Ten centers study on the present state of treatment for hypercholesterolemia in patients with coronary artery disease. Korean J Med. 2005. 69:371–378.
17. Kim SH, Park JS, Zo JH, Kim MA, Kim HS. Treatment gap in the management of hypercholesterolemia in Korea: return on expenditure achieved for lipid therapy (REALITY). Korean Circ J. 2006. 36:593–599.
18. June JE. Cholesterol lowering therapy in coronary artery disease: with particular reference to statins. Korean Circ J. 2001. 31:849–856.
19. Kim MK, Kim HL, Min HS, et al. Changes of the lipoprotein profiles with time after discontinuation of stain therapy. Korean Circ J. 2008. 38:36–42.
20. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972. 18:499–502.
21. Annual report on the cause of death statistics. 2006. Seoul: Korean National Statistical Office.
22. Hyre AD, Muntner P, Menke A, Raggi P, He J. Trends in ATP-III defined high blood cholesterol prevalence, awareness, treatment and control among U.S. adults. Ann Epidemiol. 2007. 17:548–555.
23. Ghandehari H, Kamal-Bahl S, Wong ND. Prevalence and extent of dyslipidemia and recommended lipid levels in US adults with and without cardiovascular comorbidities: the National Health and Nutrition Examination Survey 2003-2004. Am Heart J. 2008. 156:112–119.
24. Lee YW, Min WK, Lee W, et al. Risk analysis of coronary heart diseases in Korean adults by using the National Cholesterol Education Program Adult Treatment Panel III. J Clin Lab Anal. 2007. 21:178–182.
25. Van Ganse E, Laforest L, Burke T, Phatak H, Souchet T. Mixed dyslipidemia among patients using lipid-lowering therapy in French general practice: an observational study. Clin Ther. 2007. 29:1671–1681.
26. Austin MA. Plasma triglyceride and coronary heart disease. Arterioscler Thromb. 1991. 11:2–14.
27. Schaefer EJ, Levy RI, Anderson DW, Danner RN, Brewer HB Jr, Blackwelder WC. Plasma-triglycerides in regulation of HDL-cholesterol levels. Lancet. 1978. 2:391–393.
28. Castelli WP. The triglyceride issue: a view from Framingham. Am Heart J. 1986. 112:432–437.
29. Hong HS, Park JS, Ryu HK, Kim WY. The association of plasma HDL-cholesterol level with cardiovascular disease related factors in Korean type 2 diabetes patients. Korean Diabetes J. 2008. 32:215–223.
30. Park SH, Choi SJ, Lee KS, Park HY. Waist circumference and waist-to-height ratio as predictors of cardiovascular disease risk in Korean adults. Circ J. 2009. 73:1643–1650.
31. Bersot T, Pépin GM, Mahley RW. Risk determination of dyslipidemia in populations characterized by low levels of high-density lipoprotein cholesterol. Am Heart J. 2003. 146:1052–1059.
32. Insurance standard of dyslipidemia. National Health Insurance Corporation. Avail from: http://www.nhic.or.kr/.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download