Abstract
Multivascular preventive and therapeutic approaches are necessary in patients with coronary artery disease because atherosclerosis has a common systemic pathogenesis. We present a rare case of sudden cardiac arrest with acute myocardial infarction induced by the total occlusion of left subclavian artery (LSCA) in a patient with a history of previous coronary artery bypass surgery using the left internal mammary artery. We initially performed blind-puncture of left brachial artery, attempting percutaneous coronary intervention because pulses were absent in both upper and lower extremities. However, the cause of sudden cardiac arrest was atherosclerotic total occlusion of LSCA. The patient was stabilized after successful revascularization of LSCA by percutaneous transluminal angioplasty with stent insertion.
Coronary artery disease (CAD) is a significant factor in sudden cardiac arrest (SCA), and multivascular therapeutic approaches are necessary in CAD patients because atherosclerosis has a common systemic pathogenesis and simultaneously affects multiple circulation. We report a rare case of SCA with acute myocardial infarction induced by the total occlusion of left subclavian artery (LSCA) in CAD patient with a history of coronary artery bypass surgery (CABG).
A 70-year-old male presented at the emergency room with SCA after complaining of typical chest pain in December 2011. We had only limited information that he had coronary risk factors including hypertension, diabetes, and smoking, and he underwent CABG 4 years ago in another hospital. After cardiopulmonary resuscitation for 15 minutes, the electrocardiogram showed ST elevation in the anterior leads. We promptly referred the patient to the cathroom for primary percutaneous coronary intervention.
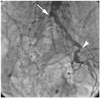
Initiall physical examination revealed absent pulses in both upper and lower extremities. We perforce performed blind-puncture at left brachial artery, and attempted coronary angiography. However, the 035" hydrophilic soft terumo wire (Terumo, Tokyo, Japan) did not pass the LSCA. Transbrachial peripheral angiography showed total occlusion of LSCA, but the graft from left internal mammary artery (LIMA) to mid left anterior descending artery (LAD) was patent (Fig. 1A). After 014" guide wire (Pilot, Abbott, Santa, Clara, CA, USA) passed the lesion, the LSCA was progressively dilated by a 2.0×20 balloon (Lacrosse, Goodman Medical Ireland Ltd., Galway, Ireland) inflated at 16 atm, and a 4.0×20 mm balloon (Lacrosse, Goodman Medical Ireland Ltd., Galway, Ireland) at 18 atm (Fig. 1B). A 7.0×24 mm stent (Coroflex Blue, Braun Vascular Systems, Berlin, Germany) was deployed at the LSCA (Fig. 1C). Transbrachial coronary angiography showed 3 vessels with CAD presenting significant atherosclerotic stenosis of proximal LAD, big obtuse marginal artery, and mid right coronary artery (Fig. 2). Peripheral angiography showed total occlusion of right common iliac artery and left external iliac artery (Fig. 3). Because the patient's vital signs were unstable, we attempted to insert the intra-aortic balloon pump (IABP) via left brachial artery. The IABP successfully passed the deployed stent of LSCA, and was optimally located in descending thoracic aorta. However, the IABP was not operating properly, and we finally removed the IABP. The patient was stabilized with medical treatment after percutaneous transluminal angioplasty (PTA), but unfortunately had sequela of ischemic brain damage.
Coronary artery disease is known to be one of the most common causes of SCA. As newer treatments of CAD continues to reduce mortality and morbidity, cardiovascular physicians increasingly confront the problem of concomitant peripheral arterial disease. There is a need to encourage new therapeutic approaches for the treatment of multivascular atherosclerotic disease in CAD patients.
Left internal mammary artery is the conduit of choice for CABG. Preoperative assessment of LIMA before CABG should be carefully performed because most subclavian atherosclerotic stenoses exist in the absence of symptoms. The comparison of blood pressure measurements in both arms is important to exclude significant subclavian stenoses that may interfere with successful cardiac circulation of the LIMA graft.1) Selective left subclavian angiography with segmental pressure measurement is indicated for patients with suspected subclavian disease who need CABG, and pseudolesions caused by respirophasic kinking of the subclavian arteries should be considered. In our case, unfortunately, we could not know whether or not preoperative evaluation of subclavian artery was precisely performed because this was our patient's first visit with SCA to our cardiovascular center.
Risk factors for atherosclerotic disease of the upper extremity are identical to those for atherosclerosis in coronary or lower extremity arteries with the exception of other etiologies specific to the upper extremity.2-6) The incidence of severe obstruction in the subclavian arteries is known to be lower than that in the iliofemoral systems, and ischemic symptoms are also less frequent because of the lower metabolic work and the propensity for collaterals formation around shoulder and scapula. PTA of atherosclerotic obstruction of the subclavian arteries should be considered for patients with reproducible arm claudication, distal hand atheroembolism, subclavian steal syndrome, and impaired inflow into internal mammary grafts, axillofemoral bypasses, and dialysis access fistulas.7) Although experiences with subclavian stenting are limited to small series, it is known that stenting is superior to balloon dilatation alone.8)9) In this case, we performed primary PTA with stent insertion at the ostium of LSCA because total occlusion of LSCA interfere with cardiac circulation of the LIMA graft, and the lesion was the culprit of SCA in this patient.
Multivascular preventive and therapeutic approaches for patients with diffuse atherosclerotic disease are certainly needed. Cardiovascular surgeons and interventionists should take care of a more proactive clinical role, along with their vascular medicine colleagues. They should also encourage optimal treatment of arterial disease affecting multiple vascular beds guided by an appreciation of the diverse natural histories associated with peripheral arterial disease.
Figures and Tables
Fig. 1
Transbrachial peripheral angiography demonstrates (A) total occlusion of left subclavian artery (LSCA) (arrow) with patent graft from left internal mammary artery to mid left anterior descending artery, (B) balloon angioplasty of LSCA (arrow), (C) successful revascularization with stent insertion at LSCA (arrow).

Fig. 2
Transbrachial peripheral angiography demonstrates (A) total occlusion of left subclavian artery (LSCA) (arrow) with patent graft from left internal mammary artery to mid left anterior descending artery, (B) balloon angioplasty of LSCA (arrow), (C) successful revascularization with stent insertion at LSCA (arrow).

References
1. Shadman R, Criqui MH, Bundens WP, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004. 44:618–623.
2. Cherry KJ. Rutherford RB, editor. Atherosclerotic occlusive disease of brachiocephalic arteries. Vascular Surgery. 2000. 5th ed. Philadephia: W.B. Saunders Company;1140–1141.
3. Arend WP, Michel BA, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990. 33:1129–1134.
4. Singer AJ, Hollander JE. Blood pressure. Assessment of interarm differences. Arch Intern Med. 1996. 156:2005–2008.
5. Fairbairn JF, Juergens JL, Spittell JA. Peripheral Vascular Diseases. 1972. 4th ed. Philadelphia: W.B. Saunders Company.
6. Kappert A. Lehrbuch und Atlas der Angiologie. 1987. 12th ed. Bern: Huber.
7. Azzarone M, Cento M, Mazzei M, Tecchio T, Ugolotti U. Symptomatic subtotal occlusion of the innominate artery treated with balloon angioplasty and stenting. J Endovasc Ther. 2000. 7:161–164.
8. Rodriguez-Lopez JA, Werner A, Martinez R, Torruella LJ, Ray LI, Diethrich EB. Stenting for atherosclerotic occlusive disease of the subclavian artery. Ann Vasc Surg. 1999. 13:254–260.
9. Hadjipetrou P, Cox S, Piemonte T, Eisenhauer A. Percutaneous revascularization of atherosclerotic obstruction of aortic arch vessels. J Am Coll Cardiol. 1999. 33:1238–1245.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download