Abstract
Background and Objectives
The treadmill exercise test (TMT) is used as a first-line test for diagnosing coronary artery disease (CAD). However, the findings of a TMT can be inconclusive, such as incomplete or equivocal results. Aortic valve sclerosis (AVS) is known to be a good predictor of CAD. We determined the usefulness of assessing AVS on 2-dimensional (2D) echocardiography for making the diagnosis of CAD in patients with inconclusive results on a TMT.
Subjects and Methods
This prospective study involved 165 consecutive patients who underwent a TMT that resulted in inconclusive findings, 2D echocardiography to detect AVS, and coronary angiography to detect CAD. Following echocardiography, AVS was classified as none, mild, or severe. CAD was defined as ≥70% narrowing of the luminal diameter on coronary angiography.
Results
CAD was more common
in patients with AVS than in patients without AVS (75% vs. 47%, respectively, p<0.01). Multiple logistic regression analysis showed that AVS was the only independent predictor of CAD {odds ratio=8.576; 95% confidence interval (CI), 3.739-19.672}. The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of the presence of AVS for predicting CAD in a patient with an inconclusive TMT were 62%, 67%, 64%, 75%, and 53%, respectively. During a 1-year clinical follow-up, patients with and without AVS were similar in terms of event-free survival rates.
The treadmill exercise test (TMT) has been used to diagnose angina pectoris in many cardiovascular centers as it is inexpensive, easily performed, and provides real-time results. Despite some inter-investigator variations, a meta-analysis found that the sensitivity and specificity of a TMT for diagnosis of coronary artery disease (CAD) averaged 68% and 77%, respectively.1) However, since a substantial number of patients with angina pectoris also have arthritic or lung diseases due to old age, they cannot reach the target heart beat and the test is terminated without completion, and in young women the depression pattern of the ST segment occasionally shows an upslope, thus making the diagnosis difficult in such cases. Although the diagnosis could be confirmed by stress echocardiography or myocardial single photon emission computerized tomography (SPECT), such modalities are costly and difficult to perform immediately when required. Another alternative is coronary multi-detector CT (MDCT) angiography; however, it involves exposure to radiation in addition to the high cost.
While aortic valve sclerosis (AVS) detected using 2-dimensional (2D) echocardiography is known to be an independent risk factor for predicting the development of CAD,2)3) it has not been investigated in association with a TMT.
The present study determined whether AVS is a predictor of CAD in patients with suspected angina pectoris in whom TMT findings were inconclusive.
The study was conducted prospectively on 354 patients who visited our outpatient clinic with symptoms suspicious of typical stable angina pectoris. All patients underwent TMT and 2D echocardiography. Coronary angiography was performed on 317 patients, excluding patients with negative TMT results. The exclusion criteria were patients with rheumatic valve diseases, patients with significant AV stenosis (a continuous wave Doppler speed of blood flow passing through the aortic valve >2 m/s, or the area of the aortic valve orifice <2 cm2), patients already diagnosed with angina pectoris by coronary angiography, atrial fibrillation, Wolff-Parkinson-White (WPW) syndrome, a history of cardiac surgery, myocardial infarction, heart failure, or left or right complete bundle branch block on electrocardiogram.
The TMT was conducted according to Bruce's protocol, and the results were interpreted based on the American College of Cardiology/American Heart Association (ACC/AHA) guidelines and were scored as negative, positive, incomplete, or equivocal.4) Negative results showed no symptoms, and had no ST segment changes at target heart rate. Positive results showed typical symptoms during the TMT regardless of reaching the target heart beat, with significant ST segment depression (based on baseline, ST segments showed >0.1 mV horizontal or downslope depression that was maintained for longer than 0.08 seconds), or ischemic ventricular arrhythmia. Incomplete results were early TMT termination due to events other than the development of ischemic arrhythmia at <90% target heart beat. Patients who reached >90%, but <100% without typical symptoms and the atypical change of ST segments during the test, were evaluated to be equivocal results.
Patients with incomplete or equivocal TMT results were defined as inconclusive patients. There were 37 (10%) negative cases, 152 (43%) positive cases, and 165 (47%) inconclusive cases.
2D transthoracic echocardiography was performed using a 3.5 MHz Sequoia C256 probe (Acuson Co., CA, USA) or a 3.5 MH Vivid 7 probe (GE Vingmed, Horten, Norway). 2D echocardiographic tests and Doppler tests were performed following the Standard Practical Guideline for 2D echocardiography from the American Society of Echocardiography.5) The area of the aortic valve orifice on the sternal left margin was measured using a static image in which the 3 valves were most widely open, while the aortic valve blood flow speed was measured on the apical 5-chamber view using a continuous wave Doppler. These measurements were taken three times and the mean was used in analysis.
Using a long axis view of the left sternum margin, valve thickness was defined as the value obtained by enlarging the area of the aortic valve, and measuring the thickest valve of the right coronary aortic valve as well as the non-coronary aortic valve during the systolic period. Using a short axis view of the left sternum margin, when movements of the right coronary aortic valve and non-coronary aortic valve during the systolic period were examined by enlarging the aortic root, a valve opening inward concave was defined as normal, whereas a valve opening inward flat or inward convex was defined as showing restricted motion.6)
A diagnosis of AVS was based on an aortic valve thickness >2 mm or restricted motion.7) AVS severity was classified as mild or severe. Mild cases were defined as the cases that only one aortic valve thicker than 2 mm, and non-restricted motion. Severe cases were defined as patients that AVS in more than two aortic valves, or sclerosis detected in one valve that was thicker than 4 mm, or restricted motion.6)
Significant CAD was diagnosed when a coronary angiogram performed through the right femoral artery showed stenosis >70% in diameter in more than one major epicardial artery.
After the TMT, the Duke treadmill score was obtained as a measure of CAD prognosis.8) This score was based on the following expression: {exercise time (min)-5×ST segment deviation (mm)-4×angina (0, 1, 2)}.
All results are presented as the mean and standard deviation. A commercial program was used for statistical analysis. Groups were compared based on the presence or absence of AVS. For continuous variables, unpaired t-tests were applied, while Chi-square tests were used to compare categorical variables. When the patients were divided to three groups according to the presence or absence of AVS and analyzed, test for trend was used. To assess factors associated with CAD, we used multiple logistic regression analysis and calculated odds ratios and 95% confidence intervals. The diagnostic value of AVS was determined using a 2×2 table considering patients with and without CAD and patients with and without AVS. Diagnostic sensitivity, specificity, accuracy, and positive and negative prediction rates were determined. In addition, the survival rate for each group was obtained using Kaplan-Meier curves. Significance was defined as a p<0.05.
This study analyzed 165 patients suspected of having angina pectoris with inconclusive TMT results. The 2D echocardiography and coronary angiography data from these patients were analyzed.
The AVS and non-AVS groups were similar in all characteristics except that the AVS group was older and had CAD more frequently (Table 1).
There were more non-AVS patients in the non-CAD than the CAD group. Conversely, there were more AVS patients in the CAD than the non-CAD group (Fig. 1). For both males and females, the incidence of CAD was higher in the AVS patients. When applying an age threshold of 60 years, we found that the incidence of CAD was higher only in AVS patients >60 years of age (Fig. 2).
Univariate analysis showed that AVS was the only risk factor for CAD in 165 patients who showed inconclusive results in the TMT (p<0.01). Multivariate logistic regression analysis to assess independent risk factors included the traditional risk factors such as, age, gender, hypertension, diabetes, smoking, hyperlipidemia (low density lipoprotein-cholesterol ≥140 mg/dL), and AVS. The results showed that AVS was the only factor predictive for CAD (odd ratio=8.576; 95% confidence interval, 3.739-19.672) (Table 2).
We found that the incidence of CAD increased as the severity of AVS increased (p for trend, p<0.001) (Table 3).
Analysis of combined inconclusive and positive result groups data showed that the sensitivity, specificity, accuracy, positive prediction rate, and negative prediction rates for the presence of AVS for CAD were 57%, 70%, 61%, 80%, and 44%, respectively (Fig. 3). In the inconclusive group, the sensitivity for CAD of severe AVS was 58% and the specificity was 70%.
Patients were analyzed in three groups: non-AVS, mild AVS, and severe AVS. The Duke treadmill scores were 5.0±4.3, 4.9±3.7, and 3.9±4.2, respectively, but the apparent decreasing trend was not found to be significant.
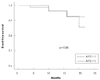
Patients were followed-up clinically for an average of 11±6 months. No patient died during this time. The incidence of major clinical events represented by coronary revascularization or rehospitalization was 5% in the non-AVS group and 4% in the AVS group. The two groups did not differ in terms of event-free survival rates (Fig. 4).
In the present study, 53% of patients had conclusive TMT results, while 47% had inconclusive findings. For the latter group, additional tests, such as coronary angiography, were performed based on risk factors for cardiovascular disease. However, a problem with performing tests by considering risk factors is that unnecessary angiograms may be performed due to a desire to assess the presence or absence of lesions. According to the recent ENCOURAGE study,9) mortality rates were similar for stable angina pectoris patients undergoing either coronary angioplasty or drug treatment. Hence, drug treatment is a useful approach in patients unlikely to have CAD.
Previous studies reported an association between AVS and CAD,10) and AVS patients had a higher incidence of CAD and consequently high mortality rate.11) CAD is more frequently observed in AVS patients because AVS is associated with aorta and carotid artery atherosclerosis. Severe AVS predicts advanced systemic atherosclerosis.12-14) AVS and atherosclerosis show similar progression features, such as the presence of oxidized lipoprotein, inflammatory cells, microscopic calcification, and proteins produced by activated macrophages in tissues. However, the increase in smooth muscle cells, calcium, and protein detected in atherosclerosis are not features of AVS.15)
According to a recent study, coronary angiography revealed the sensitivity was 64% and the specificity was 71% in the diagnostic value of AVS for CAD.2) Similarly, a Korean study reported that AVS patients were examined by coronary angiogram and the results showed that the sensitivity was 65% and the specificity was 66%.3) Those two studies differed from the present study in that they involved patients with stable angina and acute coronary syndrome, whereas our study involved patients with stable angina. Despite this difference, the present study found AVS had a sensitivity of 62% and a specificity of 67% for the diagnosis of CAD, similar to the previous reports.
The present study examined whether gender or age affected the association between AVS and CAD. Gender had no effect, while CAD was more common in AVS patients >60 years of age. We compared coronary angiography findings between inconclusive and all TMT patients and found there was no difference in terms of the diagnostic value of AVS for CAD (Fig. 3).
The Duke treadmill score did not differ between AVS and non-AVS patients, reflecting the change of ST segments (the variable with the largest effect on the score) was not large in either group. AVS and non-AVS patients showed a similar incidence of major clinical events during the approximately 1-year clinical follow-up, which may reflect the short follow-up period. A follow-up study of AVS and stenosis patients by Otto et al.11) found that differences in mortality rates became significant only after 5 years.
In conclusion, if the results of a TMT for patients with chest pain on exertion are inconclusive, the presence of AVS on echocardiography is a good predictor of CAD.
Figures and Tables
Fig. 1
Prevalence of coronary artery disease according to aortic valve sclerosis. CAD: coronary artery disease, AVS: aortic valve sclerosis.

Fig. 2
Prevalence of coronary artery disease according to gender and age. A: prevalence of coronary artery disease in males and females with and without aortic valve sclerosis. B: prevalence of coronary artery disease in patients aged ≤60 years and >60 years with and without aortic valve sclerosis. AVS: aortic valve sclerosis, CAD: coronary artery disease.

Fig. 3
The diagnostic value of aortic valve sclerosis for coronary artery disease. A: in inconclusive and positive treadmill exercise test patients (n=317). B: in inconclusive treadmill exercise test patients (n=165). PPV: positive predictive value, NPV: negative predictive value, AVS: aortic valve sclerosis.
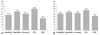
Fig. 4
Kaplan-Meier curves for event-free survival in patients with and without aortic valve sclerosis. Event-free survival was similar in both groups. AVS: aortic valve sclerosis.
References
1. Gianrossi R, Detrano R, Mulvihill D, et al. Exercise-induced ST depression in the diagnosis of coronary artery disease: a meta-analysis. Circulation. 1989. 80:87–98.
2. Sui SJ, Ren MY, Xu FY, Zhang Y. A high association of aortic valve sclerosis detected by transthoracic echocardiography with coronary arteriosclerosis. Cardiology. 2007. 108:322–330.
3. Park YW, Kim DS, Jeong YS, et al. Association between aortic valve sclerosis and risk factors of coronary artery disease in patients with suspected coronary artery disease. Korean Circ J. 2006. 36:374–380.
4. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002. 106:1883–1892.
5. Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guideline (ACC/AHA/ASE Committee to update the 1997 Guideline for the Clinical Application of Echocardiography). Circulation. 2003. 108:1146–1162.
6. Jeon DS, Lee MY, Kim CJ, et al. The severity of aortic valve sclerosis is associated with carotid intima media thickness/plaque in neurologically asymptomatic patients. Korean Circ J. 2004. 34:1049–1055.
7. Tolstrup K, Crawford MH, Roldan CA. Morphologic characteristics of aortic valve sclerosis by transesophageal echocardiography: importance for the prediction of coronary artery disease. Cardiology. 2002. 98:154–158.
8. Mark DB, Shaw L, Harrell FE Jr, et al. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med. 1991. 325:849–853.
9. Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007. 356:1503–1516.
10. Pohle K, Maffert R, Ropers D, et al. Progression of aortic valve calcification: association with coronary atherosclerosis and cardiovascular risk factors. Circulation. 2001. 104:1927–1932.
11. Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med. 1999. 341:142–147.
12. Agmon Y, Khandheria BK, Meissner I, et al. Aortic valve sclerosis and aortic atherosclerosis: different manifestations of the same disease?: insights from a population-based study. J Am Coll Cardiol. 2001. 38:827–834.
13. Adler Y, Levinger U, Koren A, et al. Relation of nonobstructive aortic valve calcium to carotid arterial atherosclerosis. Am J Cardiol. 2000. 86:1102–1105.
14. Tolstrup K, Roldan CA, Qualls CR, Crawford MH. Aortic valve sclerosis, mitral annular calcium, and aortic root sclerosis as markers of atherosclerosis in men. Am J Cardiol. 2002. 89:1030–1034.
15. O'Brien KD, Kuusisto J, Reichenbach DD, et al. Osteopontin is expressed in human aortic valvular lesions. Circulation. 1995. 92:2163–2168.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download