Introduction
Mitral annular calcification (MAC) is a common echocardiographic finding in the elderly, and it is considered to be a chronic degenerative disorder.1) Calcium is deposited in the mitral ring and in the angular space between the posterior left ventricular (LV) wall and the adjacent posterior mitral leaflet.2) A less widely known and rarely described entity is caseous calcification of the mitral annulus, which often resembles a tumor.3) This entity is characterized by a calcified envelope with caseous material inside,4-6) which has been shown to be an admixture of calcium, fatty acids, and cholesterol with a toothpaste-like texture.7)
This variant of MAC rarely causes symptoms and is usually found incidentally on transthoracic echocardiography as a large, round, bright, echogenic mass with a central echolucent area. Such findings occasionally lead to misdiagnoses of intracardiac tumor,3) abscess,8) vegetation, or thrombus9) and result in unnecessary surgery. However, caseous MAC has been shown to be indolent and benign in nature.2) Thus, conservative management is recommended. We report our clinical experience with two cases of caseous MAC.
Case
Case 1
A 74-year-old woman visited the outpatient clinic with New York Heart Association functional class II dyspnea on exertion, which had begun two months previously. Her past medical history was significant for osteoporosis and spine surgery.
Initial physical examination revealed no abnormalities. Her heartbeat was regular, and no cardiac murmurs were audible. Her lung sounds were clear, and there was no peripheral edema.
Liver and renal function and thyroid hormone and hemoglobin levels were normal. Plain chest radiography revealed a nodular mass-like lesion in the left lower lung zone, measuring 23 mm in the largest dimension (Fig. 1).
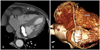
The patient underwent transthoracic echocardiography for assessment of a cardiac condition related to her dyspnea. A round, echogenic structure was found in the posterior mitral annular area. It measured 36 mm×18 mm in diameter and had a smooth border and an echolucent center. The patient had mild mitral regurgitation and grade 1 diastolic dysfunction (the mitral flow E/A ratio was 0.71) (Fig. 2). Cardiac computed tomography (CT) was performed in order to characterize this mass-like lesion. Cardiac CT revealed a dense calcified mass in the mitral valvular annulus, measuring 3.6×16×18 mm. Attenuation in the center of the mass was lower than that seen in the border. The coronary arteries were normal, with no stenosis (Fig. 3).
We thought there was a slight possibility that the caseous MAC was associated with the patient's symptoms, and we decided to follow her condition. She returned three months later and had no symptoms.
Case 2
A 65-year-old woman was brought to a local hospital in an unconscious state. A brain CT scan had revealed no significant findings. As there was no improvement in her clinical status, she was referred to our hospital.
She had no history of relevant clinical illness. Initial physical examination revealed a blood pressure of 241/134 mmHg, a pulse rate of 106 beats/min, a respiratory rate of 30 breaths/min, and a body temperature of 37.4℃. The patient was semi-comatose. Her heart rhythm was regular, and no abnormal heart sounds were detected.
Abnormal laboratory parameters were as follows: white blood cell count, 15,350/µL (segmented neutrophils, 92.1%); hemoglobin, 16.5 g/dL; platelet count, 143×103/µL; prothrombin time, 15.5 seconds (International Normalized Ratio, 1.26); activated prothrombin time, 39.5 second; total cholesterol, 240 mg/dL; low-density lipoprotein cholesterol, 165 mg/dL; high-density lipoprotein cholesterol, 63 mg/dL; triglyceride 93 mg/dL; ionized calcium, 1.39 mmol/L; creatinine kinase MB fraction, 26.14 ng/mL; cardiac troponin I, 5.151 ng/mL; and N-terminal prohormone brain natriuretic peptide, 2,509 pg/mL. No significant ST-T segment changes were noted on the initial electrocardiogram, and the LV ejection fraction and wall motion were normal on echocardiography performed in the emergency room. The next day, the patient's creatinine kinase MB fraction level had decreased to normal.
Brain magnetic resonance imaging showed multiple embolic infarctions, so she was started on anticoagulation therapy. On the third day after presentation, the patient underwent transthoracic echocardiography to assess cardiac abnormalities relevant to the multiple embolic events. A round, echogenic mass, measuring 25.5×12.7 mm, was visualized in the posterior-to-posterolateral mitral leaflet, extending to the endocardium of the LV base. The mass had a central echolucent area, measuring 12.8×9.6 mm. The left and right atria were enlarged, and there was mild mitral stenosis and regurgitation (Fig. 4A and B). On the fourth day, her orientation and consciousness were restored to normal, but there was residual dysarthria and difficulty swallowing.
Transesophageal echocardiography was performed after two weeks of anticoagulation to better characterize the mass and to evaluate for the presence of an intracardiac thrombus. The mass, measuring 17.3×14.0 mm, had a smooth border with central echolucency (11.0×9.5 mm). Mild mitral stenosis was noted, with a mean pressure gradient of 3.4 mmHg, but there was no intracardiac thrombus (Fig. 4C and D).
The patient was treated with anticoagulant and antihypertensive medications. She was followed up in the outpatient clinic, and no additional embolic events occurred over the next six months. At that time, anticoagulation therapy was discontinued, and the patient was switched to an antiplatelet agent.
Discussion
The prevalence of caseous MAC has been reported to be 0.0557)-0.067%2) in general populations referred for echocardiographic evaluation. The hallmark feature of this variant form of MAC is central liquefaction. Histology shows a calcified envelope and an amorphous acellular eosinophilic material surrounded by macrophages and lymphocytes. The mechanism of central liquefaction is unknown.
Both of the current cases showed the typical echocardiographic appearance of caseous MAC: large, round, echo-dense masses with smooth borders, containing central echolucent areas along the posterior mitral annulus.
The first patient had mild dyspnea, but her symptoms had little correlation with the echocardiographic findings. Most of the symptoms associated with caseous MAC that lead to referral for echocardiography are non-specific. The echocardiographic findings of caseous calcification are incidental and are usually unrelated to the symptoms.2)
Because caseous MAC is known to be indolent and benign, most patients are treated conservatively.2) However, in some cases, surgery4-8) is performed based on suspicion of an intracardiac tumor, for prevention of embolism, or for treatment of severe mitral valvular dysfunction.
Although MAC is regarded as a risk factor for systemic embolism and stroke,1) the risk of these entities has not been established in the setting of caseous MAC. Harpaz et al.2) reported that during a mean follow-up period of 3.8 years, 7 (37%) patients had unchanged repeat echocardiographic studies, which suggest the stability of this condition. Most case reports have shown good prognosis with no cerebrovascular events. Interestingly, one study reported spontaneous resolution at the one-year follow-up visit.10) However, at least one case has been reported in association with embolic stroke;6) therefore, patients presenting with a decrease in mass size and flattening in the echolucent center warrant careful follow-up.
The second patient in the current study had cerebral embolic infarction. Neither the transthoracic echocardiography performed on the third day after presentation nor the transesophageal echocardiography performed two weeks after the start of anticoagulation revealed any potential source of embolism. However, it is possible that a thrombus undetected on transthoracic echocardiography resolved after anticoagulation. Therefore, the relationship between caseous mitral calcification and embolism in our cases is still uncertain. In addition, the size of the mass decreased during the short period of 10 days, but the echolucent center did not flatten. Unfortunately, interpretation is limited because earlier measurements were done through the transthoracic window, whereas later measurement were done through the transesophageal window.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download