Abstract
Background and Objectives
Doppler myocardial imaging (DMI) has been suggested as a method of quantifying inducible ischemia during dobutamine stress echocardiography (DSE). Post-systolic motion (PSM) detected by DMI is related to peri-infarct ischemia during DSE. We hypothesized that PSM during DSE would predict recovery of dysfunctional myocardium after successful percutaneous coronary intervention (PCI).
Subjects and Methods
Thirty patients with dysfunctional myocardium in the left anterior descending coronary artery (LAD) territory were divided into two groups according to improvement of wall motion score index (WMSI) in the LAD territory at 6 months after successful PCI of the LAD. DMI was evaluated in the LAD territory during DSE. Fifteen patients showed improved WMSI (1.42±0.39) while the other 15 had unchanged WMSI (1.75±0.46) 1 month after PCI. Myocardial velocity was measured in the mid-septal, apico-septal, and basal anterior segments of the LAD artery territory. PSM was defined as a positive wave appearing after the curve of systolic ejection had reached the zero line.
Patients with coronary artery disease and chronic hypoperfusion develop persistent left ventricular (LV) dysfunction that returns to normal after revascularization, the so called myocardium hibernation.1)2) The distinction between ventricular dysfunction arising from either myocardial fibrosis or underperfused but viable hibernating myocardium has important therapeutic and prognostic implications.3)
For the diagnosis of viable myocardium, several authors4-6) have used dobutamine stress echocardiography (DSE) and demonstrated the usefulness of the color Doppler tissue image (DTI) M-mode with DSE for the prediction of reversible dysfunction early after reperfusion in patients with acute myocardial infarction.
In two experimental animal studies, postsystolic shortening during acute coronary occlusion was correlated to recovery of LV systolic function measured early and late after reperfusion.7)8) These results suggested that postsystolic motion (PSM) may be related to an active process reflecting myocardial viability. Although different methods have revealed PSM of the ischemic myocardial segments as regional asynchrony of myocardial wall motion during acute ischemia,9)10) there are a few reports concerning PSM and its diagnostic value for the improvement of dysfunctional myocardium during DSE after successful revascularization. Therefore, this study was performed to determine whether PSM during DSE predicts functional recovery of dysfunctional myocardium after successful percutaneous coronary intervention (PCI) in patients with chronic stable angina.
We enrolled 30 patients diagnosed with chronic stable angina with dysfunctional myocardium in the left anterior descending coronary artery (LAD) territory, who underwent a successful PCI on the LAD territory by routine methods. A dysfunctional myocardium was defined by wall motion abnormality in the LAD territory. DSE was performed in all 30 patients 1 month after PCI. The patients were divided into two groups according to improvement of dysfunctional myocardium in the LAD territory 6 months later. Exclusion criteria included: prior PCI or myocardial infarction, acute coronary syndrome, a significant lesion at other coronary arteries, dilated cardiomyopathy, significant valvular disease, arterial and ventricular arrhythmia, pacemaker implantation, bundle branch block and an LV ejection fraction below 45%. Signed informed consent was obtained from all individuals before enrollment into the study.
Echocardiographic studies were performed using the commercially available Vivid 7 echocardiography (General Electronics Corp., Horten, Norway) imaging system and a 3.5 MHz transducer equipped with Doppler myocardial imaging (DMI) imaging.
A standard dobutamine stress protocol was used starting at a dobutamine infusion rate of 5 µg/min/kg body weight, and thereafter increasing the dosage every 3 minutes to 10, 20, 30, and 40 µg/kg/min.11) Apical 2 and 4 chamber views were used for the assessment of longitudinal myocardial motion by DMI.
The DMI study during DSE was performed using a real-time color DMI system. At frame rates of >100 frames/s, this system has a high temporal resolution of <20 ms. All images were saved to magneto-optical disks for off-line analysis.
Off-line visual assessment of echocardiographic images was performed independently by two investigators (KSK, LYS), blinded to the functional recovery data. Analysis of the stress test, including wall motion score index (WMSI), was confined to the LAD artery territory. The apico-septal and mid-septal segments in the apical four-chamber view and basal anterior segment in the apical two-chamber view were selected for assessment of WMSI and DMI data of the LAD territory.12) The average value from three beats was taken for each measurement.
To evaluate WMSI in the LAD artery territory, each ventricular segment of the LAD artery territory was scored on a five-point scale: 1=normal, 2=hypokinesis, 3=akinesis, 4=dyskinesis and 5=aneurysm. Following the recommendations of the American Society of Echocardiography,13) a regional WMSI was calculated for each patient as the sum of the scores of the segments in the LAD artery territory divided by three. Functional recovery of dysfunctional myocardium was defined as an increase in WMSI at 6-month follow-up echocardiography.
To assess DMI at the LAD artery territory during DSE, peak systolic velocity, peak velocity of PSM, peak velocity of early ventricular filling, and peak velocity of atrial contraction were determined. PSM was defined as a positive wave appearing after the curve of systolic ejection had reached the zero line (Fig. 1). The inter- and intra-observer concordances of PSM were, respectively, 89 and 91% in our echocardiographic laboratory.
The Statistical Package for Social Science 12.0 (SPSS inc., Chicago, IL, USA) statistical software package was used for all calculations. Data are presented as means±standard deviation (SD) for continuous variables and as percentages for categorical data. DMI data were analyzed using an unpaired Student's t-test. Categorical data and proportions were analyzed using the Chi-square test. Cut-off values for DMI during low-dose DSE for discriminating the presence from the absence of functional recovery were derived from receiver-operating characteristics curves as the points with the highest sum of sensitivity plus specificity; the corresponding areas under the curves were obtained. A p<0.05 was regarded as statistically significant.
Table 1 presents the demographic characteristics of the study populations. There were no differences in age or gender between the groups. In addition, there were no differences in cardiovascular risk factors such as obesity, history of smoking, and diabetes between the groups except for history of hypertension. Medications taken during the 6-month follow-up period were not different between the groups. However, by definition, the regional WMSI in the group where functional recovery was present was significantly decreased compared with that of the group where functional recovery was absent (p<0.05).
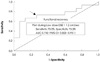
Myocardial Doppler parameters, including peak systolic and diastolic velocity of resting, low and high dose DSE were not different between the functional recovery groups (Table 2). However, PSM of low dose DSE in the presence of functional recovery was significantly increased compared to the group with an absence of functional recovery (Fig. 2). When comparing PSM according to functional recovery, 1.2 cm/sec was found to be applicable as a cut-off value for differentiating between presence and absence of functional recovery; this cut-off was associated with 73% sensitivity and 73% specificity (Fig. 3).
This study evaluated the efficacy of myocardial Doppler imaging during low dose DSE evaluated at one month in dysfunctional myocardium after successful PCI in patients with chronic stable angina.
Postsystolic thickening or motion of myocardium is a myocardial contraction that develops during late systolic or early diastolic phase, and PSM can be considered not only as a marker of acute ischemia but also as a marker of successful myocardial reperfusion in an animal model.14)15)
Several authors have reported that PSM is a useful marker for viability or functional recovery after reperfusion in obstructive coronary artery diseases like acute myocardial infarction and chronic occlusive disease. Hosokawa et al.16) demonstrated that postsystolic shortening in patients with acute anterior myocardial infarction correlates with subsequent recovery of systolic function by ventriculography after revascularization. In addition, Song et al.17) reported that PSM detected by DMI in the infarct territory was related to peri-infarction ischemia or viability at DSE.
In the case of chronic coronary artery disease, Wong et al.18) demonstrated that post-ejection shortening assessed by radionuclide ventriculography causes regional post-systolic emptying, and this correlates with post-revascularization improvement in regional wall motion. Barletta et al.19) reported that regions with PSM were viable and showed a moderate decrease in coronary perfusion. In contrast, Lim et al.20) stated recently that PSM is not a specific marker of viability in chronic LV dysfunction and that delayed myocardial shortening may be associated with scarred segments.
However, several authors suggest the efficacy of PSM during DSE in coronary artery disease. Celutkiene et al.12) reported that the peak velocity of PSM during DSE was the most accurate index of induced ischemia (sensitivity 73-100%, specificity 82-97%). Akutsu et al.21) demonstrated that functional recovery in the stunned myocardium was predicted by DSE performed 1 week after early reperfusion following acute myocardial infarction. Moreover, Rambaldi et al.22) observed that the ratio of ejection phase shortening and post-systolic shortening velocity during DSE could predict a death-free outcome during long-term prospective follow-up after surgical reperfusion in patients with severe LV dysfunction. In our study, PSM during DSE in patients with chronic coronary artery disease and functional recovery at follow-up was increased compared to that in patients with no functional recovery after successful reperfusion of an occluded coronary artery.
The major value of assessing myocardial viability is to select patients who will benefit from revascularization. However, our study was conducted after reperfusion of the occluded coronary artery to diagnose the hibernating myocardium. We therefore propose that recognition and diagnosis of hibernating myocardium is important from a practical standpoint and may affect patient management.23)
The limitations of this study are as follows. First, because the study included a small number of patients and a limited follow-up period, large-scale and long-term follow-up studies are required to confirm our findings. Second, because the dysfunctional myocardium may have been injured more intensely,24) the recovery of dysfunctional myocardium may have been delayed more than 1 month after reperfusion. Third, angle dependency is another limitation of myocardial Doppler imaging, which has been reported to be minimized by the apical approach.25) In addition, myocardial Doppler imaging can evaluate only the longitudinal motion, but not the radial motion. Fourth, we estimated the wall motion of the LAD artery territory only in the apical two- and four-chamber views but, not in the apical three chamber view. Fifth, we assessed the dysfunctional myocardium only by WMSI but not by independent methods, including scintigraphy and magnetic resonance imaging.
Nevertheless, the present results suggest that PSM during DSE predicts functional recovery of dysfunctional myocardium after successful PCI in patients with chronic coronary artery disease.
Figures and Tables
Fig. 1
Myocardial doppler image. Postsystolic motion (PSM) during resting (left panels) and low-dose dobutamine stress echocardiography (DSE) (right panels) states was measured at apical four (upper panels) and two (lower panels) chamber views. The average PSM during low-dose DSE was increased compared to that in the resting state.

Fig. 2
Comparison of post-systolic motion (PSM) between resting and low-dose dobutamine stress echocardiography (DSE). In the resting state, there was no difference in PSM between the functional recovery (FR) (+) and (-) groups. However, PSM of FR (+) was significantly increased compared to that of the FR (-) group.

Fig. 3
Receiver operating characteristic curve of post-systolic motion (PSM) during low-dose dobutamine stress echocardiography (DSE) for the prediction of functional recovery. AUC: area under the curve.
Acknowledgments
This research was supported by research grants from Catholic University of Daegu in 2006.
References
1. van den Berg EK Jr, Popma JJ, Dehmer GJ, et al. Reversible segmental left ventricular dysfunction after coronary angioplasty. Circulation. 1990. 81:1210–1216.
2. Rahimtoola SH. The hibernating myocardium. Am Heart J. 1989. 117:211–221.
3. Jeong MH, Cha KS, Seo JP, et al. Hibernating myocardium in chronic coronary artery disease. Korean Circ J. 1997. 27:206–212.
4. Nishio M, Tanouchi J, Tanaka K, et al. Dobutamine stress echocardiography at 7.5 µg/kg/min using color tissue Doppler imaging M-mode safely predicts reversible dysfunction early after reperfusion in patients with acute myocardial infarction. Am J Cardiol. 1999. 83:340–344.
5. Kim KS. The usefulness of dobutamine stress echocardiography for evaluation of viable myocardium in hibernating myocardium. Korean Circ J. 1998. 28:1233–1236.
6. Lee SH, Park H, Son MS, et al. Evaluation of Doppler echocardiographic patterns of left ventricular filling in the patients with recent acute myocardial infarction. Korean Circ J. 1993. 23:223–229.
7. Brown MA, Norris RM, Takayama M, White HD. Post-systolic shortening: a marker of potential for early recovery of acutely ischemic myocardium in the dog. Cardiovasc Res. 1987. 21:703–716.
8. Takayama M, Norris RM, Brown MA, Armiger LC, Rivers JT, White HD. Postsystolic shortening of acutely ischemic canine myocardium predicts early and late recovery of function following coronary artery reperfusion. Circulation. 1988. 78:994–1007.
9. Kass DA, Midei M, Brinker J, Maughan WL. Influence of coronary occlusion during PTCA on end-systolic and end-diastolic pressure-volume relations in humans. Circulation. 1990. 81:447–460.
10. Hosokawa H, Sheenhan FH, Suzuki T. Measurement of postsystolic shortening to assess viability and predict recovery of left ventricular function after acute myocardial infarction. J Am Coll Cardiol. 2000. 35:1842–1849.
11. Cain P, Baglin T, Spicer D, Short L, Marwick TH. Application of tissue Doppler to interpretation of dobutamine echocardiography and comparison with quantitative coronary angiography. Am J Cardiol. 2001. 87:525–531.
12. Celutkiene J, Sutherland GR, Laucevicius A, Zakarkaite D, Rudys A, Grabauskiene V. Is post-systolic motion the optimal ultrasound parameter to detect induced ischaemia during dobutamine stress echocardiography? Eur Heart J. 2004. 25:932–942.
13. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005. 18:1440–1463.
14. Song JM, Kim JH, Kim YH, et al. Temporal changes and histologic relation of postsystolic thickening in an animal model of acute ischemia and reperfusion. J Am Soc Echocardiogr. 2003. 16:409–414.
15. Citro R, Galderisi M. Myocardial postsystolic motion in ischemic and not ischemic myocardium: the clinical value of tissue Doppler. Echocardiography. 2005. 22:525–532.
16. Hosokawa H, Sheehan FH, Suzuki T. Measurement of postsystolic shortening to assess viability and predict recovery of left ventricular function after acute myocardial infarction. J Am Coll Cardiol. 2000. 35:1842–1849.
17. Song JK, Song JM, Kang DH, Haluska B, Marwick TH. Postsystolic thickening detected by Doppler myocardial imaging: a marker of viability or ischemia in patients with myocardial infarction. Clin Cardiol. 2004. 27:29–32.
18. Wong CK, Freedman SB, Bautovich G, Hutton BF. Correlation between post-ejection shortening and improvement in regional wall motion after revascularization in patients with coronary artery disease. Int J Cardiol. 1996. 54:61–67.
19. Barletta G, Del Bene R, Lo Sapio P, Gallini C, Fantini F. Postejection thickening as a marker of viable myocardium: an echocardiographic study in patients with chronic coronary artery disease. Basic Res Cardiol. 1998. 93:313–324.
20. Lim P, Pasquet A, Gerber B, et al. Is postsystolic shortening a marker of viability in chronic left ventricular ischemic dysfunction?: comparison with late enhancement contrast magnetic resonance imaging. J Am Soc Echocardiogr. 2008. 21:452–457.
21. Akutsu Y, Shinozuka A, Kodama Y, et al. Usefulness of simultaneous evaluations of contractile reserve, perfusion, and metabolism during dobutamine stress for predicting wall motion reversibility (myocardial stunning) after successful PTCA. Jpn Heart J. 2004. 45:195–204.
22. Rambaldi R, Bax JJ, Rizzello V, et al. Post-systolic shortening during dobutamine stress echocardiography predicts cardiac survival in patients with severe left ventricular dysfunction. Coron Artery Dis. 2005. 16:141–145.
23. Pigott JD, Kouchoukos NT, Oberman A, Cutter GR. Late results of surgical and medical therapy for patients with coronary artery disease and depressed left ventricular function. J Am Coll Cardiol. 1985. 5:1036–1045.
24. Boden WE, Brooks WW, Conrad CH, Bing OH, Hood WB Jr. Incomplete, delayed functional recovery late after reperfusion following acute myocardial infarction: "maimed myocardium". Am Heart J. 1995. 130:922–932.
25. Rambaldi R, Poldermans D, Fioretti PM, et al. Usefulness of pulse-wave Doppler tissue sampling and dobutamine stress echocardiography for the diagnosis of right coronary artery narrowing. Am J Cardiol. 1998. 81:1411–1415.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download