Abstract
Background and Objectives
Vasospastic angina is correlated with endothelial dysfunction. We compared endothelial function using flow-mediated vasodilatation (FMD) and circulating endothelial progenitor cells (EPCs) between patients with vasospasm and those without vasospasm and studied the effect of statin therapy on the changes of FMD and EPCs in vasospastic angina patients.
Subjects and Methods
In 133 patients who underwent an ergonovine provocation test, endothelial function was compared based on the presence or absence of spasm. The patients with coronary artery spasm (74 patients) were randomly assigned to either the 10 mg rosuvastatin group or the placebo group. We compared changes in the FMD and EPCs level for 6 months from the time of enrollment between the two groups.
Results
The incidence of cigarette smokers was higher in vasospastic angina patients than in those without spasm (p<0.001). The number of EPCs (68.6±36.1 vs. 103.7±39.3/200 µL, p<0.001) and the FMD (7.1±4.5 vs. 8.6±3.6%, p=0.044) were significantly lower in patients with coronary artery spasm than in those without spasm. After 6 months of rosuvastatin treatment, the number of CD45lowCD34+ vascular endothelial growth factor receptor 2 (VEGFR2)+ cells, which was defined as EPCs, increased significantly from 73.1±37.8/200 µL to 99.1±37.8/200 µL (p=0.002). The FMD was significantly ameliorated from 7.3±4.1 to 9.3±3.4% after 6 months of treatment (p<0.001). The FMD was correlated with the EPCs count before treatment (r=0.229, p=0.049) and after 6 months of treatment (r=0.268, p=0.020).
Variant angina is a disease which is common among Asians, and its main cause is coronary artery spasm. Coronary artery spasm plays an important role in the pathogenesis of various ischemic heart diseases, including not only variant angina, but also unstable angina, myocardial infarction, and sudden death.1) There have been various reports on the pathophysiologic mechanism of vasospastic angina, but recently the mechanism is understood to involve the change in the characteristics of atherosclerosis itself. That is, several studies have reported an increase in the adhesion molecules or inflammatory cells in atherosclerotic lesions in patients with vasospastic angina.2-5) Coronary artery spasm can be induced by acetylcholine when the endothelium is removed or damaged. Thus, patients with coronary artery spasm have a disturbance in the endothelial function of the coronary arteries.6)
Endothelial function is evaluated not only by conventional venous occlusive plethysmography, but also by flow-mediated vasodilatation (FMD) and pulse wave velocity, and the clinical significance of these methods has been studied for various diseases. Recently, endothelial progenitor cells (EPCs) have been in the research spotlight. EPCs are derived from the bone marrow and circulate in the peripheral blood and have been implicated in adult neovasculrization.7) EPCs are capable of proliferation and differentiation into endothelial cells, and are therefore candidates for vascular regeneration.8) An inverse correlation has been found between the number of EPCs and cardiovascular risk factors in healthy people and in patients with coronary artery disease, and the number of EPCs is correlated with endothelial function.9)10)
There are several strategies for treating endothelial dysfunction, but recently the role of statins, the effectiveness of which has been proved in various patient groups and clinical situations, is increasing. In addition, statins are known to be a drug that increases circulating EPCs.11) We therefore designed a prospective randomized study using rosuvastatin, the effect on circulating EPCs of which has been demonstrated in an experimental study.12) Specifically, patients with vasospastic angina were compared with a healthy control group using FMD and EPCs to evaluate endothelial dysfunction. In addition, we determined whether the additional use of a statin was effective in improving endothelial function.
Between July 2006 and November 2007, we studied 133 consecutive patients who underwent an intracoronary ergonovine provocation test. An intracoronary ergonovine test was performed in patients in whom 1) chest pain was noted at rest and 2) significant coronary artery diseases (>50% of the luminal diameter of the major coronary arteries) was absent. Exclusion criteria were as follows: 1) patients in whom acute myocardial infarction occurred within the most recent 6 months, 2) patients in whom coronary intervention had been performed, 3) patients with co-existing infectious diseases, and 4) patients with co-existing hepatic and renal diseases. All patients gave informed consent according to a protocol approved by the Ethical Committee of Wonkwang University Hospital.
In the fasting state, coronary angiography was performed by the Judkin method following the puncture of the femoral artery or via a radial artery approach. Calcium antagonists and long-acting nitrates were discontinued for at least 72 hours prior to coronary angiography, but sublingual nitroglycerin was administered as required. The severity of coronary atherosclerotic lesions was evaluated from at least three projections in all patients.
In patients in which significant coronary stenosis was absent, an ergonovine provocation test was performed, as previously reported.13)14) In brief, ergonovine (in 0.9% saline solution) was injected at 10 µg/min for 4 minutes (a maximal dose of 40 µg) into the right coronary artery and at 16 µg/min over 4 minutes (a total dose of 64 µg) into the left coronary artery, with at least a 5 minutes interval between each injection. The occurrence of chest pain, the change in the ST segment on EKG, and the development of spasm on coronary angiography were examined. Positive results were defined as cases in which >99% of focal spasm was noted on coronary angiography in the presence of typical chest pain or abnormal EKG findings. We divided patients into groups with spasm and without spasm.
In previous reports, circulating mononuclear cells with the phenotype, CD34+CD133+/CD34+CD133+VEGFR2+, were quantified as tentative progenitor cells (PCs)/EPCs.15) Four milliliters of peripheral blood was drawn before coronary angiography, and white blood cells were stained with PE-Cy5-conjugated anti-CD45 monoclonal antibody (Dynona, Korea), fluorescein isothiocyanate (FITC)-conjugated anti-CD34 monoclonal antibody (Dynona), and PE-conjugated anti-vascular endothelial growth factor receptor 2 (VEGFR2) monoclonal antibody (R & D, USA), and further incubated in the dark for 1 hour. After appropriate gating with low cytoplasmic granularity and with low expression of CD45, the number of CD34+VEGFR2+ cells was quantified and expressed as the number of cells per 106 total events or the number of cells per 200 µL of blood. The number of CD45lowCD34+VEGFR2+ cells were then counted (Fig. 1).
Imaging studies of the right brachial artery were performed using an ultrasound machine (Vivid 7; GE, USA) equipped with a 10 MHz linear-array transducer the morning after coronary angiography, based on a standard technique.16) Briefly, baseline data for the diameter and mean blood flow velocity of the brachial artery were quantified after 10 minutes of rest in the supine position in an air-conditioned room at a position that was 1-2 cm above the elbow. Endothelium-dependent vasodilatation was assessed by measuring the change in the diameter of the brachial artery after 60 seconds of reactive hyperemia relative to baseline measurements after deflation of a cuff on the forearm that was inflated to 250 mmHg for 5 minutes. All images were coded and recorded on a disk for subsequent blinded analysis. The diameter of the brachial artery was measured as the R wave on the electrocardiogram, and at the interface between the media and adventitia of the anterior and posterior walls. We measured each diameter three times during two beats, and the mean data was used for final analysis. The intra- and inter-observer variabilities for repeated measurements were 0.00±0.07 and 0.05±0.16 mm, respectively, in our laboratory.
Seventy-five patients in whom coronary artery spasm was induced were randomized to the rosuvastatin or the placebo group in a 1:1 ratio. All patients received long-acting nifedipine, and the nitrate was given at the physician's discretion. In patients with diabetes or uncontrolled hypertension an angiotensin converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) was prescribed in addition to nifedipine.
The patients were observed for 6 months. One patient was dismissed from the study because of an adverse effect related to nifedipine. After 6 months, blood samples for the EPCs count were obtained, and the FMD was measured after a 72 hour cessation of nifedipine. The clinical end point was the occurrence of cardiac death, myocardial infarction, stroke, or peripheral artery disease during the study period. We compared the clinical and laboratory parameters between the two groups.
All measurements are represented as the mean±standard deviation. Inter-group analysis was done using independent t-tests and χ2 tests, which were conducted using Statistical Package for Social Science (SPSS) 12.0 for Windows (SPSS Inc., Chicago, IL, USA). To compare the change in biochemical parameters before and after the medication, we used paired t-tests. Statistical significance was set at p<0.05.
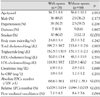
One hundred thirty-three patients underwent an ergonovine provocation test. The patient characteristics are shown in Table 1. The incidence of current smokers was higher in the patients with induced spasm than in those without spasm (40.0% vs. 12.1%, respectively; p<0.001). The number of EPCs (68.6±36.1 vs. 103.7±39.3/200 µL; p<0.001) and the FMD (7.1±4.5% vs. 8.6±3.6%; p=0.044) were significantly lower in patients with coronary artery spasm than in those without spasm. There was no significant difference in the most relevant clinical characteristics between the two groups (Table 1). The circulating number of EPCs in the presence or absence of risk factors is presented in Fig. 2. The patients >65 years of age, obesity, and cigarette smoking revealed a significantly reduced number of EPCs compared with the patients without these risk factors.
Seventy-four patients completed the study. Baseline laboratory findings were similar, and the administration of ACEI or ARB was similar between the patients with or without statin treatment (16.2% vs. 18.9%, respectively; p=0.760). The incidence of cigarette smokers was 34.2% in the statin group and 45.9% in the placebo group (p=0.300). Four patients in the statin group quit smoking {4/13 (30.8%)} and 3 patients in the placebo group quit smoking {3/17 (17.6%)}; p=0.666). After 6 months of rosuvastatin treatment, the levels of total cholesterol and low density lipoprotein (LDL)-cholesterol were significantly reduced in patients with vasospastic angina (Table 2). The number of CD45lowCD34+VEGFR2+ cells, which were defined as EPCs, was 73.1±37.8/200 µL, and 6 months later, the number of CD45lowCD34+VEGFR2+ cells increased to 99.1±37.8/200 µL (p=0.002) (Fig. 3). The change in endothelial function was determined by measuring the FMD before and after statin treatment. The FMD was significantly ameliorated from 7.3±4.1% to 9.3±3.4% in 6 months after the treatment (p<0.001). Myocardial infarction occurred in only one patient in the statin treatment group, and no cardiovascular events developed in the placebo group.
The quantitative analysis of baseline CD45lowCD34+VEGFR2+ cells was correlated with the value of the FMD before statin treatment (Fig. 4). After 6 months of statin treatment, the increase in the number of EPCs and the FMD were also correlated (r=0.268, p=0.020).
In the current study we showed that the number of EPCs was reduced in patients with vasospastic angina, and statin treatment increased the number of EPCs. Also, these findings were correlated with endothelial function, as measured by the FMD.
The vascular endothelium is a multifactorial organ, the integrity of which is essential to normal vascular physiology, and in which dysfunction can be a critical factor in the pathogenesis of vascular disease. Acetylcholine, which is used for provocation tests in patients with vasospastic angina, is an endothelial vasodilator through the release of nitric oxide (NO), and induces coronary dilation in healthy subjects, but causes vasoconstriction in patients with atherosclerosis. Thus, patients with coronary artery spasm have a disturbance in endothelial function of the coronary arteries.6)17)
Endothelial functions can be evaluated in several ways. Venous occlusive plethysmography is a standard test, but cannot be applied widely in the clinical setting because of its invasiveness. In addition, the method of measuring the FMD using the brachial artery is used widely, but it requires a skill set to perform it properly, and the interobserver variability is large. The direct measurement of EPCs is another alternative. EPCs are derived from various types of cytokines, as well as from the bone marrow and peripheral blood by ischemic stimulation, and are involved in neovascularization and the restoration of damaged vessels. EPCs are also known to play an important role in maintaining the integrity of blood vessels.18-20) Hill et al.10) reported that in adult men with various risk factors for cardiovascular disease, the number of EPCs is closely correlated with the risk factors of cardiovascular diseases and the functions of the vascular endothelium. Werner et al.21) reported that the number of circulating EPCs is closely correlated with the prognosis of cardiovascular diseases. There have been reports on the significance of EPCs in various patients groups, but no report has been made on the value in assessing variant angina. The present study revealed that the number of EPCs and the FMD were reduced in patients with vasospastic angina. These results suggest that the pathogenesis of vasospastic angina involves endothelial dysfunction, and it can be measured by the number of circulating EPCs.
There are several methods of improving vascular endothelial function. Statins are known to lower the level of serum lipids and to have "endothelial protective properties" through its anti-oxidative effect, anti-inflammatory effect, and increase in endothelial NO production.22) Studies using the FMD have also reported that various types of statins can improve endothelial function in various patient groups.23-25) Moreover, statins are known to increase the number of circulating EPCs.11) In agreement with previous reports, statin therapy in the present study increased the FMD and the increased FMD and number of EPCs had a good correlation with each other, suggesting that the number of EPCs can be used as a marker of endothelial function.
Smoking cessation also increases the number of circulating EPCs.15) Smoking cessation leads to a rapid restoration of the number of EPCs within 2 weeks. In our study, there was a similar incidence of current smoking and smoking cessation between the two groups; however, it was difficult to conclude the effect of smoking cessation on the number of EPCs because this study was not limited to smoking patients. The group treated with a statin had fewer current smokers enrolled and more patients who had stopped smoking than the placebo group, even though the difference was statistically insignificant, so we presumed that smoking status could affect the number of EPCs.
Our study had several limitations. The study was not blinded, and the sample size was small. We used ergonovine to induce coronary artery spasm, but the results of the ergonovine provocation test might differ from provocation by acetylcholine, which is an endothelium-dependent vasodilator. Another major limitation was the low adverse event rate of vasospastic angina itself. So, we could not compare the prognosis of vasospastic angina patients based on statin treatment. However, a significant difference was observed in the number of EPCs and the FMD between the two groups, so we expected a better prognosis in the patients with vasospastic angina treated with statins. Further study is needed to generalize our results.
In conclusion, the number of circulating EPCs and the FMD were reduced in patients with vasospastic angina, and statin treatment increased the number of EPCs and the FMD. The number of EPCs was correlated with the FMD. Thus, circulating EPCs may play a role as a biologic marker for endothelial function in patients with vasospastic angina.
Figures and Tables
Fig. 1
Quantification of EPCs by flow cytometry. Circulating EPCs were identified by flow cytometry with low cytoplasmic granularity (R1) and with expression of cell surface antigens, such as CD45lowCD34+VEGFR2+. Arrows indicate CD45lowCD34+VEGFR2+ cells. EPCs: endothelial progenitor cells, VEGFR2: vascular endothelial growth factor receptor 2, SSC: side scather, FITC: fluorescein isothiocyanate.

Fig. 2
The number of circulating EPCs in the presence or absence of risk factors. *Obesity was defined by a waist circumference ≥90 cm for men and ≥80 cm for women. EPCs: endothelial progenitor cells, HT: hypertension, HyperL: hyperlipidemia.

Fig. 3
The number of circulating EPCs in peripheral blood and FMD of the brachial artery were increased after 6 months of statin treatment in patients with vasospastic angina. *p<0.001 by paired t-test. VEGFR2: vascular endothelial growth factor receptor 2, EPCs: endothelial progenitor cells, FMD: flow-mediated vasodilatation.

Fig. 4
There is a linear correlation between FMD and EPCs before and 6 months after statin treatment. VEGFR2: vascular endothelial growth factor receptor 2, EPCs: endothelial progenitor cells, FMD: flow-mediated vasodilatation.

References
1. Hillis LD, Braunwald E. Coronary-artery spasm. N Engl J Med. 1978. 299:695–702.
2. Suzuki H, Kawai S, Aizawa T, et al. Histologic evaluation of coronary plaque in patients with variant angina: relationship between vasospasm and neointimal hyperplasia in primary coronary lesions. J Am Coll Cardiol. 1999. 33:198–205.
3. Miwa K, Igawa A, Inoue H. Soluble E-selectin, ICAM-1 and VCAM-1 levels in systemic and coronary circulation in patients with variant angina. Cardiovasc Res. 1997. 36:37–44.
4. Terashima M, Akita H, Kanazawa K, et al. Circulating T-lymphocyte activation in patients with variant angina. Coron Artery Dis. 2002. 13:161–168.
5. Yun KH, Oh SK, Park EM, et al. An increased monocyte count predicts coronary artery spasm in patients with resting chest pain and insignificant coronary artery stenosis. Korean J Intern Med. 2006. 21:97–102.
6. Kugiyama K, Murohara T, Yasue H, et al. Increased constrictor response to acetylcholine of the isolated coronary arteries from patients with variant angina. Int J Cardiol. 1995. 52:223–233.
7. Asahara T, Murohara T, Sullivan A, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997. 275:964–967.
8. Gehling UM, Ergun S, Schumacher U, et al. In vitro differentiation of endothelial cells from AC133-positive progenitor cells. Blood. 2000. 95:3106–3112.
9. Vasa M, Fichtlscherer S, Aicher A, et al. Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res. 2001. 89:E1–E7.
10. Hill JM, Zalos G, Halcox JP, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003. 348:593–600.
11. Vasa M, Fichtlscherer S, Aicher A, et al. Increase in circulating progenitor cells by statin therapy in patients with stable coronary artery disease. Circulation. 2001. 103:2885–2890.
12. Thum T, Tsikas D, Stein S, et al. Suppression of endothelial progenitor cells in human coronary artery disease by the endogenous nitric oxide synthase inhibitor asymmetric dimethylarginine. J Am Coll Cardiol. 2005. 46:1693–1701.
13. Igarashi Y, Yamazoe M, Shibata A. Effect of direct intracoronary administration of methylergonovine in patients with and without variant angina. Am Heart J. 1991. 121:1094–1100.
14. Sueda S, Kohno H, Fukuda H, et al. Clinical impact of selective spasm provocation tests: comparisons between acetylcholine and ergonovine in 1508 examinations. Coron Artery Dis. 2004. 15:491–497.
15. Kondo T, Hayashi M, Takeshita K, et al. Smoking cessation rapidly increases circulating progenitor cells in peripheral blood in chronic smokers. Arterioscler Thromb Vasc Biol. 2004. 24:1442–1447.
16. Koh KK, Quon MJ, Han SH, et al. Additive beneficial effects of losartan combined with simvastatin in the treatment of hypercholesterolemic, hypertensive patients. Circulation. 2004. 110:3687–3692.
17. Shin DI, Seung K, Kim DB, et al. Comparison of the long-term prognosis between coronary vasospasm and intermediate vasoconstriction induced by the administration of acetylcholine. Korean Circ J. 2006. 36:503–509.
18. Walter DH, Rittig K, Bahlmann FH, et al. Statin therapy accelerates reendothelialization: a novel effect involving mobilization and incorporation of bone marrow-derived endothelial progenitor cells. Circulation. 2002. 105:3017–3024.
19. Rafii S, Lyden D. Therapeutic stem and progenitor cell transplantation for organ vascularization and regeneration. Nat Med. 2003. 9:702–712.
20. Gill M, Dias S, Hattori K, et al. Vascular trauma induces rapid but transient mobilization of VEGFR2(+)AC133(+) endothelial precursor cells. Circ Res. 2001. 88:167–174.
21. Werner N, Kosiol S, Schiegl T, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005. 353:999–1007.
22. Bonetti PO, Lerman LO, Napoli C, Lerman A. Statin effects beyond lipid lowering: are they clinically relevant? Eur Heart J. 2003. 24:225–248.
23. Karatzis E, Lekakis J, Papamichael C, et al. Rapid effect of pravastatin on endothelial function and lipid peroxidation in unstable angina. Int J Cardiol. 2005. 101:65–70.
24. Dogra GK, Watts GF, Chan DC, Stanton K. Statin therapy improves brachial artery vasodilator function in patients with Type 1 diabetes and microalbuminuria. Diabet Med. 2005. 22:239–242.
25. Lee Y, Kim K. The short-term effect of atorvastatin on flow-mediated vasodilation, pulse wave velocity and carotid intima-media thickness in patients with moderate cholesterolemia. Korean Circ J. 2008. 38:144–151.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download