Abstract
Obesity is a well-established risk factor for many chronic disorders. However, the effect of weight change after acute myocardial infarction (AMI) is not well known. Among consecutive patients who underwent percutaneous coronary intervention between November 2005 and November 2007 due to AMI, patients who were overweight (23.0≤body mass index [BMI]<27.5 kg/m2, n=341) and obese (BMI≥27.5 kg/m2, n=80) were selected for analysis. According to weight change, the patients were divided into 4 groups: Group I (weight loss>5%, n=61), Group II (0%<weight loss≤5%, n=133), Group III (0%≤weight gain<5%, n=181), and Group IV (weight gain≥5%, n=46). We assessed the association between weight change and major adverse cardiac events (MACE). Greater weight loss was more frequent among older individuals (Group I: 64.1±12.4 years, II: 60.6±12.1 years, III: 59.0±11.9 years, IV: 61.4±10.6 years; p=0.028) and patients with diabetes (Group I: 34.4%, II: 27.1%, III: 21.2%, IV: 15.2%; p=0.009). However, there were no significant differences in baseline characteristics or in angiographic or procedural factors except for the proportions of patients with three-vessel disease, which were higher in patients with weight loss (Group I: 20.8%, II: 23.0%, III: 12.5%, IV: 11.6%; p=0.005). The group with greater weight loss had the highest MACE rate at the 12-month clinical follow-up (Group I: 36.9%, II: 25.0%, III: 25.9%, IV: 17.3%; p=0.020). Although weight loss after AMI appears to be associated with worse outcomes, it remains unclear whether the effect is of cardiac origin.
Generally, overweight and obesity are associated with increased risk for developing cardiovascular disease, and they are prevalent risk factors in patients with acute myocardial infarction (AMI).1-3 However, several studies of patients undergoing revascularization have shown better outcomes or no increased risk in overweight and obese patients.4-9 A study that focused on ST-segment elevation myocardial infarction showed similar results.10 However, these conclusions were derived from analysis of baseline weight and not weight change. It is questionable whether the "obesity paradox" in AMI is solely based on baseline obesity. Despite some reports on the effect of weight change on clinical outcomes,11-13 there are few available data on the prognostic impact of weight change in patients with AMI. In fact, the effects of weight change have been questioned, including in patients with established cardiovascular disease.8,14-17 Furthermore, these previous results were based on Western and not Oriental populations.
Thus, the present analysis was undertaken to evaluate the effect of weight change on clinical outcomes after AMI in a Korean population.
A total of 622 AMI patients, whose body weight and height were available for their first and follow-up visits, were treated by percutaneous coronary intervention (PCI) at Chonnam National University Hospital and Gwangju Veterans Hospital between November 2005 and November 2007. Among these patients, overweight (23.0≤body mass index [BMI]<27.5 kg/m2, n=341) and obese (BMI≥27.5 kg/m2, n=80) patients were selected for analysis according to criteria suggested by the World Health Organization for the Asian population.18 BMI was calculated as the weight in kilograms divided by the square of height in meters. The diagnosis of AMI was based on the triad of chest pain, electrocardiogram changes, and raised serum cardiac enzyme levels. According to weight change, the 421 patients selected for study were divided into 4 groups: Group I (weight loss>5%, n=61), Group II (0%<weight loss≤5%, n=133), Group III (0%≤weight gain<5%, n=181), and Group IV (weight gain≥5%, n=46). Variables analyzed in the present study included age, gender, body mass index, vital signs, Killip class, risk factors, past regular medication, comorbidities, electrocardiographic location of AMI, initial treatment strategy, drugs, angiographic findings, in-hospital complications, medical therapy in hospital, and 12-month rate of major adverse cardiac events (MACE; cardiac death, re-infarction, re-PCI, coronary artery bypass graft), among others. Patient characteristics included medical history (diabetes mellitus, hypertension, smoking, hyperlipidemia, previous AMI, previous angina, previous coronary artery bypass graft, previous PCI, and family history), presentation characteristics (systolic blood pressure, diastolic blood pressure, heart rate, and left ventricular ejection fraction, which was determined within 24 hours after admission in most cases), and laboratory findings (levels of glucose, creatinine, cardiac enzymes, serum cholesterol, high sensitivity C-reactive protein [hs-CRP], and N-terminal pro-brain natriuretic peptide). Medical treatment and angiographic and procedural findings were also recorded. We assessed the association between weight change and MACE.
Statistical analysis was performed by using SPSS software, version 15.0 (SPSS-PC Inc, Chicago, IL, USA). All continuous variables are reported as mean values±standard deviations (SDs). Multiple logistic regression analyses were done to identify the prognostic factors affecting the results. Chi-square tests and independent-sample t-tests were used to identify predictors for mortality and MACE, and logistic regression analysis was used to adjust for confounding factors. A p value<0.05 was considered as significant.
The baseline characteristics of the 4 patient groups are listed in Table 1. Patients with weight loss >5% were significantly older (Group I: 64.1±12.4 years, Group II: 60.6±12.1 years, Group III: 59.0±11.9 years, Group IV: 61.4±10.6 years; p=0.028), had lower left ventricular ejection fraction (Group I: 52.8±13.1%, Group II: 56.7±11.4%, Group III: 56.7±11.9%, Group IV: 56.2±11.4%; p=0.036), and were more often diabetic (Group I: 34.4%, II: 27.1%, III: 21.2%, IV: 15.2%; p=0.009). There were no significant differences in distributions of gender, blood pressure, heart rate, hypertension, smoking, hyperlipidemia, or previous PCI rate among the groups (p>0.05).
Table 2 shows the results of the laboratory examination. Patients with weight loss >5% had higher levels of serum glucose (Group I: 188.9±86.1 mg/dl, II: 177.6±80.9 mg/dl, III: 161.1±64.6 mg/dl, IV: 149.4±61.6 mg/dl; p=0.009), and patients with either weight loss >5% or weight gain >5% had higher levels of hs-CRP (Group I: 2.4±2.7 mg/dl, II: 1.7±3.2 mg/dl, III: 1.7±2.6 mg/dl, IV: 3.0±3.5 mg/dl; p<0.024). There were no significant differences in the levels of serum creatinine, cholesterol, N-terminal pro-brain natriuretic peptide, or cardiac markers among the groups.
At admission, we used aspirin and clopidogrel in all
patients. There were numerically higher rates of use of cilostazol, β-blockers, angiotensin-converting enzyme inhibitors, vasopressors, and diuretics in patients with weight loss >5%; however, there were no significant differences among the other groups (Table 3).
Almost all patients underwent PCI successfully (Group I: 99.0%, II: 99.5%, III: 98.8%, IV: 98.9%; p=0.757) and we used drug-eluting stents in most cases (Group I: 75.5%, II: 83.5%, III: 79.6%, IV: 84.8%; p=0.314). Overall, the mean total stent number used per patient was 1.7±1.0 (Group I: 1.8±0.9%, II: 1.6±0.8%, III: 1.7±1.0%, IV: 1.8±1.0%; p=0.519). In patients with weight loss, there was a higher incidence of three-vessel disease (Group I: 20.8%, II: 23.0%, III: 12.5%, IV: 11.6%; p=0.005). There were no statistically significant differences in distributions of target lesions, lesion classification, or Thrombolysis in Myocardial Infarction (TIMI) flow (Table 4).
Table 5 demonstrates left ventricular ejection fraction at 6 months and rates of MACE at 12 months for each patient group. Left ventricular ejection fraction increased in all groups compared with their respective baseline values; however, patients with weight loss >5% still had a lower ejection fraction than did the other groups (54.6±11.1% in Group I, 60.5±9.6% in II, 60.0±10.7% in III, and 59.8±11.3% in group IV; p=0.020). The higher weight reduction group had a significantly higher rate of MACE at 12 months (MACE: 36.9% in Group I, 25.0% in II, 25.9% in III, and 17.3% in group IV, p=0.012; all-cause mortality: 6.0% in Group I, 4.5% in II, 1.8% in III, and 0% in group IV, p=0.007; non-cardiac death: 3.6% in Group I, 1.9% in II, 0.9% in III, and 0% in group IV, p=0.036). However, there was no significant differences in rates of cardiac death (2.4% in Group I, 2.6% in II, 0.9% in III, and 0% in group IV; p=0.088).
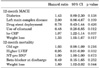
Multiple logistic regression analysis revealed that cilostazol use, hs-CRP level, and weight loss were independent risk factors of MACE at 12 months, whereas left ventricular ejection fraction and weight loss were independent risk factors of mortality at 12 months (Table 6).
Our data revealed that there was a high rate of overweight and obesity (67.7%) among patients treated for AMI and a high rate of weight reduction (46.1%) during the follow-up period. Also, the present study showed worse outcomes in patients with weight reduction >5%. Finally, the rate of noncardiac and not cardiac death was significantly higher in the weight reduction group.
Weight change after AMI was shown in previous studies. According to these studies, the rate of overweight and obesity in AMI was 64.9% in OPTIMAAL (the Optimal Trial in Myocardial Infarction with Angiotensin II Antagonist Losartan),19-21 59.2% in the CONSENSUS II (Cooperative New Scandinavian Enalapril Survival Study II) trial,22 58.6% in 4S,23 and 73.6% in ENRICHD (the Enhancing Recovery in Coronary Heart Disease patients),13 respectively. Although these results are similar to the overall ones of our study (67.7%), the weight reduction rates differed. Of overweight and obese myocardial infarction patients, the rate of weight reduction was 46.1% in our study compared with a rate of weight loss in overweight and obese myocardial infarction patients of 24.9% in OPTIMAAL, 13.2% in CONSENSUS II, and 19.5% in 4S. Meanwhile, the rate of weight reduction>5% was higher in a previous study than in ours (24.4% in ENRICHD vs. 14.9% in the present study). The time of weight measurement differed among the studies. In the present study, we measured follow-up weight at 9.7±5.6 months after AMI. On the other hand, weight was measured at 3 months in the OPTIMAAL and CONSENSUS II trials and at 1 year in 4S. Nevertheless, the tendency for weight reduction was more prominent in our population. Although it is unclear which factors underlie these differences, we presume that racial differences might be one of them. If weight reduction after myocardial infarction influences clinical outcomes, this will be worthy of notice.
As stated above, weight reduction >5% was associated with poor outcomes, which is similar to the findings of previous studies. The all-cause death rate was significantly increased with weight loss after myocardial infarction (hazard ratio in OPTIMAAL: 1.26 [1.01-1.56, p=0.039]; hazard ratio in CONSENSUS II: 1.96 [1.07-3.57, p=0.029]; hazard ratio in 4S: 1.44 [1.13-1.85, p=0.004]; and hazard ratio in ENRICHD: 2.06 [1.20-3.52, p=0.009]).11 Despite the different time periods of weight change, the associations between weight loss and prognosis were remarkably consistent across studies, including the present study. From the known relationship between mortality and obesity in healthy subjects, it would be anticipated that weight loss from an initial condition of obesity or overweight would be associated with decreased risk compared with weight gain. However, studies have yielded results that contradict this presumption. Thus, overweight and obesity contributed the most to the increased risk associated with weigh reduction. Weight loss was associated with more comorbidities at baseline, including older age, decreased left ventricular ejection fraction, diabetes, and more common three-vessel disease. Moreover, despite the slightly increased left ventricular ejection fraction in the weight reduction group during the follow-up, it was still significantly lower than that in the other groups, which suggests that weight reduction might be a marker of cardiovascular disease severity or poorer overall health. Kennedy et al.11 posited that the fact that weight loss was associated with increased risk indicates that severity of the cardiac condition determines prognosis. Also, they proposed that one important reason for the observed association between weight loss and worse prognosis may be pronounced metabolic stress with neurohormonal and cytokine activation,24,25 causing weight loss and increased mortality risk.
Indeed, our data showed increased rates of MACE and mortality. However, cardiac mortality and myocardial infarction rates were not significantly higher in the weight-reduction group, whereas the rate of noncardiac death was significantly increased in the weight-reduction group. This fact suggests that poor prognosis in the weight-reduction group stems from noncardiac and not cardiac causes.
This study had some limitations. Although BMI has been considered to be a marker of obesity, it is a crude indicator of body adiposity and is not a direct measurement of body composition. Therefore, it may not reflect the actual degree of body fat content. We did not define obesity by other methods such as waist circumference, waist-hip ratio, or abdominal height. According to one report, despite an inverse relation of overall obesity as assessed by BMI with mortality in patients with AMI, abdominal obesity as assessed by waist-hip ratio appears to be an independent predictor of all-cause mortality.26
This study was an observational registry with the inherent limitations of a retrospective analysis. Also, the follow-up duration was relatively short. Therefore, we could not exclude the possibility that obesity may influence very long-term outcomes, because obesity may have a delayed effect on the progression of coronary artery disease. Furthermore, we selected patients whose body weight and height were measured during the follow-up period, which may introduce selection bias. Lastly, our sample is not necessarily representative of the Korean population.
Weight reduction after AMI in this Korean study was as prominent as that seen in studies based on Western populations. Although weight loss after AMI was associated with poor outcomes, it is unclear whether the effect has a cardiac origin. Further prospective study is needed to elucidate the effect of intentional weight reduction after AMI.
Figures and Tables
TABLE 1
Baseline clinical characteristics

SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate, BPM: beat per minute, BMI: body mass index, LVEF: left ventricular ejection fraction, STEMI: ST segment elevation myocardial infarction, AF: atrial fibrillation, AMI: acute myocardial infarction, CABG: coronary arterial bypass graft, PCI: percutaneous coronary intervention.
ACKNOWLEDGEMENTS
This study was performed with the support of the Korean Society of Circulation and Korea Ministry of Health and Welfare (A084869), Republic of Korea.
References
1. Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983. 67:968–977.

2. Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005. 366:1640–1649.

3. Lopez-Jimenez F, Jacobsen SJ, Reeder GS, Weston SA, Meverden RA, Roger VL. Prevalence and secular trends of excess body weight and impact on outcomes after myocardial infarction in the community. Chest. 2004. 125:1205–1212.

4. Gurm HS, Whitlow PL, Kip KE. BARI Investigators. The impact of body mass index on short- and long-term outcomes inpatients undergoing coronary revascularization. Insights from the bypass angioplasty revascularization investigation (BARI). J Am Coll Cardiol. 2002. 39:834–840.

5. Gurm HS, Brennan DM, Booth J, Tcheng JE, Lincoff AM, Topol EJ. Impact of body mass index on outcome after percutaneous coronary intervention (the obesity paradox). Am J Cardiol. 2002. 90:42–45.

6. Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002. 39:578–584.

7. Minutello RM, Chou ET, Hong MK, Bergman G, Parikh M, Iacovone F, et al. Impact of body mass index on in-hospital outcomes following percutaneous coronary intervention (report from the New York State Angioplasty Registry). Am J Cardiol. 2004. 93:1229–1232.

8. Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006. 368:666–678.

9. Buettner HJ, Mueller C, Gick M, Ferenc M, Allgeier J, Comberg T, et al. The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J. 2007. 28:1694–1701.

10. Kang WY, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, et al. Korea Acute Myocardial Infarction Registry Investigators. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol. 2010. 55:84–91.

11. Kennedy LM, Dickstein K, Anker SD, James M, Cook TJ, Kristianson K, et al. Weight-change as a prognostic marker in 12 550 patients following acute myocardial infarction or with stable coronary artery disease. Eur Heart J. 2006. 27:2755–2762.

12. Fadl YY, Krumholz HM, Kosiborod M, Masoudi FA, Peterson PN, Reid KJ, et al. Predictors of weight change in overweight patients with myocardial infarction. Am Heart J. 2007. 154:711–717.

13. Lopez-Jimenez F, Wu CO, Tian X, O'Connor C, Rich MW, Burg MM, et al. Weight change after myocardial infarction--the Enhancing Recovery in Coronary Heart Disease patients (ENRICHD) experience. Am Heart J. 2008. 155:478–484.

14. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009. 53:1925–1932.
15. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Woo MA, Tillisch JH. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001. 38:789–795.

16. Lavie CJ, Milani R, Mehra MR, Ventura HO, Messerli FH. Obesity, weight reduction and survival in heart failure. J Am Coll Cardiol. 2002. 39:1563.

17. Allison DB, Zannolli R, Faith MS, Heo M, Pietrobelli A, VanItallie TB, et al. Weight loss increases and fat loss decreases all-cause mortality rate: results from two independent cohort studies. Int J Obes Relat Metab Disord. 1999. 23:603–611.

18. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004. 363:157–163.
19. Dickstein K, Kjekshus J. OPTIMAAL Steering Committee of the OPTIMAAL Study Group. Effects of losartan and captopril on mortality and morbidity in high-risk patients after acute myocardial infarction: the OPTIMAAL randomised trial. Optimal Trial in Myocardial Infarction with Angiotensin II Antagonist Losartan. Lancet. 2002. 360:752–760.

20. Dickstein K, Kjekshus J. OPTIMAAL Trial Steering Committee and Investigators. Optimal Trial in Myocardial Infarction with the Angiotensin II Antagonist Losartan. Comparison of baseline data, initial course, and management: losartan versus captopril following acute myocardial infarction (The OPTIMAAL Trial). OPTIMAAL Trial Steering Committee and Investigators. Optimal Trial in Myocardial Infarction with the Angiotensin II Antagonist Losartan. Am J Cardiol. 2001. 87:766–771.

21. Dickstein K, Kjekshus J. Comparison of the effects of losartan and captopril on mortality in patients after acute myocardial infarction: the OPTIMAAL trial design. Optimal Therapy in Myocardial Infarction with the Angiotensin II Antagonist Losartan. Am J Cardiol. 1999. 83:477–481.

22. Swedberg K, Held P, Kjekshus J, Rasmussen K, Rydén L, Wedel H. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med. 1992. 327:678–684.

23. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994. 344:1383–1389.
24. Remme WJ. Effect of ACE inhibition on neurohormones. Eur Heart J. 1998. 19:Suppl J. J16–J23.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download