Abstract
According to the "drip and ship" concept, patients who are not responsive to intravenous tissue plasminogen activator (IV-tPA) at a community hospital may be candidates for subsequent intra-arterial (IA) thrombolysis at a comprehensive stroke center. We elucidated the efficacy and safety of combined IV/IA thrombolysis via the drip and ship approach. We retrospectively reviewed patients with acute ischemic stroke who underwent combined IV/IA thrombolysis between March 2006 and June 2009. The patients were divided into two groups (inside hospital IV-tPA vs. outside hospital IV-tPA). We compared the short- and long-term clinical outcome, recanalization rate, intracranial hemorrhage after the procedure, and onset to treatment time between the two groups. A total of 23 patients with inside hospital IV-tPA and 10 patients with outside hospital IV-tPA were included. The mean pre-treatment National Institutes of Health Stroke Scale (NIHSS) scores were 15.8 and 17.5, respectively. Baseline characteristics were not significantly different between the two groups. The NIHSS score at 1 week and favorable outcome rate (modified Rankin Scale ≤2) 3 months after the procedure were not significantly different (p=0.730 and p=0.141, respectively). The rate of recanalization and intracranial hemorrhage were not significantly different (p=0.560 and p=0.730, respectively). The onset to IA thrombolysis time was also not significantly different (222.7 vs. 239.3 minutes, p=0.455). Our results suggest that initiation of IV-tPA in a community hospital with rapid transfer to a comprehensive stroke center for subsequent IA thrombolysis can be a safe and feasible therapeutic option in acute stroke management.
Intravenous tissue plasminogen activator (IV-tPA) should be administered to all eligible ischemic stroke patients within 3 hours of stroke onset to achieve early improvement in neurologic deficits. When treatment with IV-tPA is recommended, patients are initially treated at a community hospital and then some patients may be transferred to a comprehensive stroke center where staff are available for continued care. This method of delivering tPA to stroke patients has been referred to as the "drip and ship" approach. To date, three groups have reported that the drip and ship approach is feasible, safe, and efficient.1-3
However, the rate of tPA use among eligible patients remains <5% and IV-tPA does not always lead to a good outcome.4,5 In terms of the "tissue clock" for thrombolysis, some patients who fail IV-tPA may be candidates for subsequent intra-arterial thrombolysis (IAT) for recanalization of an occluded vessel. Favorable outcomes of combined IV/IA thrombolytic therapy have been reported in recent studies.6,7 A single-center report showed that full-dose IV-tPA (0.9 mg/kg) followed by IAT is as safe and efficient as combined thrombolysis with low-dose IV-tPA.8 Thus, if patient selection is carefully controlled, delivering tPA via the drip and ship approach, followed by subsequent IAT at a comprehensive stroke center, could be a useful therapeutic option in the management of patients with acute ischemic stroke (AIS).
Hence, we elucidated the efficacy and safety of patients with combined IV/IA thrombolytic therapy who were administered full-dose IV-tPA at an outside hospital (OH) before IAT, and compared the outcomes with patients who were administered IV-tPA at our hospital (inside hospital [IH]). Additionally, we determined whether there was a significant difference in time delay from stroke onset to thrombolytic treatment between the two groups.
We retrospectively reviewed patients with AIS who underwent IV/IA combined thrombolysis between March 2006 and June 2009. The patients were divided into two groups according to whether t-PA was administered IH or OH. This study, including the protocol and informed consent for subsequent IAT, was approved by the Chonnam National University Hospital Institutional Review Board (CNUH IRB). The reviewers recorded the stroke onset time, time of arrival at the emergency room, tPA bolus time IH or OH, initiation time of IAT, and the National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS) scores at baseline and at 7 days and 3 months after IAT. The time of arrival to the emergency room and tPA bolus times recorded in the OH medical records were considered correct times. All other reported data, including adverse events, outcomes, and the recanalization rate were obtained from our prospective stroke registry.
We reviewed all patients with AIS who were treated with combined IV/IA thrombolytic therapy at our hospital during the study period. Patients who initially received IV-tPA at an OH were included. After the IV-tPA infusion, patients without neurologic improvement underwent MRI (MR diffusion/perfusion imaging and MR angiography) or computed tomography perfusion (CTP) and angiography (CTA). We selected eligible patients for subsequent IAT according to the following criteria: (1) persistent occlusion of a large intracranial vessel, such as the distal internal carotid artery (ICA), M1 of the middle cerebral artery (MCA), or basilar artery (BA); (2) cortical signs and symptoms; and (3) no large hypodense areas (>1/3 of MCA territory) on non-contrast brain CT. If available, a mismatch between the CBV and TTP on CTP (>20% difference on visual inspection), or diffusion-perfusion mismatch on MRI, was also assessed for the selection of candidate patients.
The eligible patients were immediately transferred to the neuro-intervention room for cerebral angiography. A microcatheter and a wire were used in most cases. Before an intra-arterial-urokinase (IA-UK) infusion, the microcatheter system was moved into the clot. The micro-guide wire was used to cross the occluded segments several times to disrupt the clot. After identification of the microcatheter tip location, a 100,000 IU bolus of UK was injected over 5 minutes. Then, with the use of an infusion or syringe pump, UK was administered at a rate of 400,000 IU/hour. Balloon-angioplasty or stenting was allowed as part of this study. After thrombolysis, a noncontrast brain CT was evaluated to screen for postprocedural complications, and patients received anti-thrombotic agents 24 hours later unless contraindicated. A follow-up brain CT or MRI was routinely performed within 48 hours after thrombolysis or at any time in the case of neurologic deterioration.
The efficacy of treatment was determined by the final rate of recanalization and the change in NIHSS score and mRS. The recanalization rates were based on the Thrombolysis in Myocardial Infarction (TIMI) grading system. Complete recanalization was defined as a TIMI grade 3 in both M1 and M2 segments of the MCA. Partial recanalization was defined as a TIMI grade 2 in either MCA segment. Successful recanalization was defined as a TIMI grade 2 or 3.
We obtained the NIHSS score at baseline and after 24 hours and 7 days. The NIHSS scores were compared between the two groups. The mRS scores 90 days after stroke onset were also obtained and compared between the two groups. Early improvement was defined as a reduction in the NIHSS score of <6 points on day 1 or an NIHSS score of <4 at 7 days after treatment. A long-term favorable outcome was defined as an mRS score of 0 to 2 at 3 months after treatment.
Safety was determined by the incidence of life-threatening bleeding within the first 48 hours after treatment and was defined as (1) symptomatic intracranial hemorrhage (ICH) or hemorrhagic transformation (HT) with clinical deterioration >1 point on the NIHSS scale, and (2) other severe systemic bleeding complications, such as groin hematomas, retroperitoneal hematomas, or gastrointestinal bleeding requiring transfusion of >3 U of blood. HT was categorized as a hemorrhagic infarction (type 1 or 2) and parenchymal hematoma (type 3 or 4) according to a previous study.9 HT or ICH was assessed by means of brain CT or MR gradient echo imaging.
Statistical analysis for categorical variables included a χ2 and Fisher exact test when cell sizes were small. Continuous variables were compared by using a Student's t-test, and non-parametric variables were compared by using the Mann-Whitney U test. Statistical analyses were performed by using SPSS, ver. 13.0 (SPSS Inc, Chicago, IL, USA).
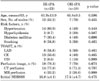
There were 33 patients with AIS who received IV/IA combined thrombolysis therapy during the study period. The numbers of patients in the IH and OH tPA groups were 23 and 10, respectively. The mean age, gender, vascular risk factors, and initial NIHSS scores in the two groups were not significantly different (Table 1).
There were no significant differences between the two groups in recanalization rates (65.2% vs 70% respectively, p=0.999). Early neurological improvement on days 1 and 7 and long-term clinical outcomes at 3 months did not differ significantly between the two groups (Table 2). The proportion of patients with thrombolysis-related symptomatic ICH and any other life-threatening symptomatic hemorrhagic event rate were comparable between the two groups (Table 2). Type 2 parenchymal hematoma developed in three patients, and two patients died despite treatment. Thrombolysis-related HT, including symptomatic and asymptomatic events, within 48 h was observed in 11 (47.8%) of 23 patients in the IH tPA group and in 5 (50%) of 10 patients in the OH tPA group (p=0.999).
With respect to the 10 patients in the OH tPA group, the mean transfer interval from outside the hospital to our hospital was 34.4 minutes, and the mean time from symptom onset to IV-tPA and IAT were 72.6 (±25.6) and 239.3 (±52.7) minutes, respectively. The onset to IV-tPA time was shorter in the patients from the OH tPA group than in the IH tPA group (p=0.000); however, the mean time from stroke onset to IAT was not significantly different between the two groups (p=0.455; Table 3).
In many clinical trials, combined IV/IA thrombolysis has been reported to improve the recanalization rate and yield a favorable clinical outcome in patients with AIS.6,7,10 Those studies were performed at large, comprehensive stroke centers where patients underwent IV-tPA administration with subsequent IAT. Most of the patients were treated with low-dose tPA (0.6 mg/kg) to reduce the occurrence of ICH.
The drip and ship approach for delivering a standard dose of IV-tPA is expected to increase the number of patients who may benefit from IV-tPA treatment within 3 hours after stroke onset. In the present study, the efficacy and safety of IAT after full-dose IV-tPA at an OH were nearly identical to the results of IAT after tPA inside the hospital. NIHSS scores on admission, the recanalization rate, and short- and long-term outcomes of the OH tPA group were not significantly different from those of the IH tPA group. The favorable outcome rate was similar to the results of two previous combined IV/IA thrombolysis studies (IMS-I and IMS-II).6,7 HT was observed in one-half of the OH tPA patients in the present study. However, only 1 patient (10%) met the IMS study criteria of symptomatic ICH, which is similar to the rate of symptomatic ICH in the IMS-I and IMS-II studies (6.3% and 11%, respectively).6,7 These results suggest that combined IAT after tPA at an OH via the drip and ship approach can be a new treatment modality for AIS using a regional referral system.
The nearly identical prognosis and safety between the two groups can be explained by several factors. First, there were similar time delays from stroke onset to IAT between the two groups. After stroke onset, IV-tPA was more rapidly administrated to the OH tPA group than to the IH group, but the time interval between the IV tPA bolus and the onset of IAT treatment was less in the IH tPA group than in the OH group. Therefore, the onset to IAT time was not significantly different between the two groups (222.7 minutes [IH tPA] vs. 239.3 minutes [OH tPA], p=0.455). Second, we tried to identify eligible patients by using MRI or CTP imaging. Patients who had diffusion-perfusion mismatching on MRI, or CVB-MTT mismatching on the CTP image, underwent subsequent IAT, which could be a reason for the good safety results in our study. We previously reported that combined IV/IA thrombolysis based on the presence of mismatches on CTP might have a relatively high rate of recanalization and a favorable outcome.11 These results suggest that if the identification of significant perfusion/diffusion or CVB-MTT mismatching on MRI/CTP is possible, sequential combination thrombolysis has potential benefits in patients with AIS who were transferred from primary hospitals after tPA administration.
IAT therapy after a full dose of IV-tPA (0.9 mg/kg) has generally been perceived as a high risk for ICH; therefore, a low dose of IV-tPA (0.6 mg/kg) has been used in most combination thrombolysis studies. Recently, Shaltoni et al reported that IAT therapy after full-dose IV-tPA in patients with persistent occlusion and/or a lack of clinical improvement appears safe compared with IV-tPA alone or low-dose IV-tPA followed by IAT.8 Our study also demonstrated that full-dose IV-tPA (0.9 mg/kg) followed by IAT had feasibility and safety compared with previous reports. Compared with the results of the tPA alone group in our hospital during the same period of this study, full-dose IV-tPA/IA combination therapy showed a similar symptomatic ICH rate and significantly more favorable outcome rate (90 day mRS ≤1) than the tPA alone group (p=0.744 and p=0.003, respectively). Recently, Pfefferkorn also reported that initiation of full-dose IV-tPA at a community hospital and subsequent on-demand endovascular mechanical recanalization at a specialized stroke center seemed to be feasible and safe in acute basilar artery occlusion.12
Our study had the following limitations: (1) a small number of patients, (2) it was a retrospective study, and (3) when selecting patients eligible for subsequent IAT, identical perfusion imaging methods were not used. Two different perfusion imaging techniques (CTP or MRI) were used according to availability, which may have influenced the selection of patients. Owing to the small patient number, these findings have to be interpreted with caution. However, there are not many patients eligible for combined IV/IA thrombolysis via drip and ship processing in a single stroke center per year. Therefore, a prospective multicenter trial would be ideal.
In conclusion, the efficacy and safety of combined IV/IA thrombolysis via the drip and ship approach are similar to those of IH tPA processing. There was no significant time delay from symptom onset to IAT between the two groups. These results suggest that initiation of IV-tPA in a community hospital with rapid transfer to a comprehensive stroke center for subsequent IAT is a safe and feasible therapeutic option in AIS management. However, randomized controlled prospective trials will be necessary.
Figures and Tables
ACKNOWLEDGEMENTS
This study was supported by a grant (CRI 08033-1) from Chonnam National University Hospital Research Institute of Clinical Medicine.
References
1. Martin-Schild S, Morales MM, Khaja AM, Barreto AD, Hallevi H, Abraham A, et al. Is the drip-and-ship approach to delivering thrombolysis for acute ischemic stroke safe? J Emerg Med. 2011. 41:135–141.

2. Silverman IE, Beland DK, Chhabra J, McCullough LD. The "drip-and-ship" approach: starting IV t-PA for acute ischemic stroke at outside hospitals prior to transfer to a regional stroke center. Conn Med. 2005. 69:613–620.
3. Rymer MM, Thurtchley D, Summers D. America Brain and Stroke Institute Stroke Team. Expanded modes of tissue plasminogen activator delivery in a comprehensive stroke center increases regional acute stroke interventions. Stroke. 2003. 34:e58–e60.

4. Katzan IL, Furlan AJ, Lloyd LE, Frank JI, Harper DL, Hinchey JA, et al. Use of tissue-type plasminogen activator for acute ischemic stroke: the Cleveland area experience. JAMA. 2000. 283:1151–1158.

5. Reed SD, Cramer SC, Blough DK, Meyer K, Jarvik JG. Treatment with tissue plasminogen activator and inpatient mortality rates for patients with ischemic stroke treated in community hospitals. Stroke. 2001. 32:1832–1840.

6. IMS Study Investigators. Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke Study. Stroke. 2004. 35:904–911.
7. IMS II Trial Investigators. The Interventional Management of Stroke (IMS) II Study. Stroke. 2007. 38:2127–2135.
8. Shaltoni HM, Albright KC, Gonzales NR, Weir RU, Khaja AM, Sugg RM, et al. Is intra-arterial thrombolysis safe after full-dose intravenous recombinant tissue plasminogen activator for acute ischemic stroke? Stroke. 2007. 38:80–84.

9. Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA. 1995. 274:1017–1025.

10. Lewandowski CA, Frankel M, Tomsick TA, Broderick J, Frey J, Clark W, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) Bridging Trial. Stroke. 1999. 30:2598–2605.

11. Kim JT, Yoon W, Park MS, Nam TS, Choi SM, Lee SH, et al. Early outcome of combined thrombolysis based on the mismatch on perfusion CT. Cerebrovasc Dis. 2009. 28:259–265.

12. Pfefferkorn T, Holtmannspötter M, Schmidt C, Bender A, Pfister HW, Straube A, et al. Drip, ship, and retrieve: cooperative recanalization therapy in acute basilar artery occlusion. Stroke. 2010. 41:722–726.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download