This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The purpose of this study was to clarify the importance of preoperative pain control using corticosteroid injections in patients with persistent rest pain (RP) before arthroscopic rotator cuff repair (ARCR).
Methods
A total of 360 patients (374 shoulders) who underwent primary ARCR and were followed up for at least 2 years were enrolled. After one-to-one propensity score matching, 266 patients (145 men and 128 women, 273 shoulders) were included in the study. Their mean age was 65.2 ± 7.7 years (range, 42 to 88 years) at the time of surgery. The patients were divided into three groups: those who required several intra-articular or subacromial bursa corticosteroid injections preoperatively for refractory RP (group A+), those in whom RP was resolved preoperatively (group A−), and those who had no RP and did not require any injections (group B). The incidence of postoperative RP and preoperative and final follow-up American Shoulder and Elbow Surgeons (ASES) scores were compared among the three groups.
Results
The incidence of postoperative RP was significantly higher in group A+ (35/91 cases, 38.5%) than in group A− (10/91, 11.0%) and group B (7/91, 7.7%, p < 0.001 for both). The preoperative ASES score was significantly lower in group A+ (33.2 ± 14.2) than in group A− (53.9 ± 11.9) and group B (62.3 ± 11.2, p < 0.001 for both), and it was significantly lower in group A− than in group B (p = 0.000). The final follow-up ASES score was significantly lower in group A+ (92.1 ± 8.4) than in group A− (97.6 ± 5.4) and group B (99.0 ± 2.5, p < 0.001 for both). There was no significant difference in the final follow-up ASES score between group A− and group B (p = 0.242).
Conclusions
Patients in whom preoperative RP could be resolved before surgery achieved postoperative outcomes comparable to those in patients who had no RP before surgery, whereas the outcomes in patients with refractory preoperative RP were inferior. The results suggest that preoperative pain control is important in patients undergoing ARCR.
Keywords: Shoulder, Rotator cuff injury, Arthroscopy, Rehabilitation, Pain management
Over the last decade, compared to open surgery, arthroscopic rotator cuff repair (ARCR) has produced excellent results in terms of clinical outcomes.
12) For successful outcome of shoulder surgery, as important as the surgical technique is the postoperative rehabilitation. Achieving an adequate range of motion (ROM) in the first 3 months after surgery is essential for good final outcome,
3) so appropriate rehabilitation during this time is critical.
However, management of postoperative rest pain (RP) in patients who had persistent RP preoperatively is often difficult, and in some cases, this prolonged RP impedes successful postoperative rehabilitation. Therefore, preoperative management of RP is important. The severity of RP has been reported to correlate with the degree of inflammation of the shoulder joint,
4) for which intra-articular
56) and subacromial bursa
78) corticosteroid injections have been reported to be effective. We have been making efforts to reduce the preoperative RP as much as possible before ARCR by injection of corticosteroids into the intra-articular space or subacromial bursa of the shoulder joint. Although preoperative pain control is considered critical for postoperative rehabilitation, there are few reports on preoperative management of shoulder pain. In this study, we aimed to investigate the relationship between the presence of preoperative RP and clinical outcome of ACLR and to determine the importance of preoperative pain control.
METHODS
Patient Selection
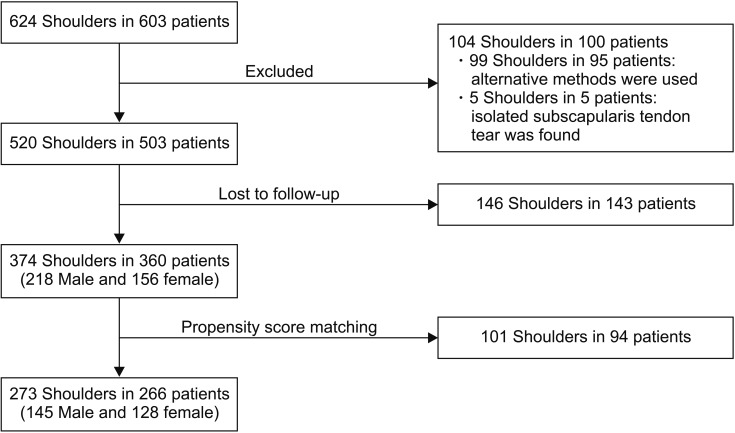
The Institutional Review Board of Funabashi Orthopaedic Hospital approved this study (IRB No. 2018038), and all of the patients provided informed consent. Primary ARCR was performed by the senior author (HS) on 603 consecutive patients (624 shoulders) from January 2005 to February 2010. Of those, 503 patients (520 shoulders) were considered eligible for enrollment. The exclusion criteria were requirement for additional treatment at the time of arthroscopic surgery, such as Bankart lesion repair or augmentation because of a massive retracted irreparable tear (99 shoulders; 95 patients), and an isolated subscapularis tendon tear (five shoulders, five patients). Two years postoperatively, 143 patients (146 shoulders) were lost to follow up, leaving 360 patients (374 shoulders) for enrollment in the study. The follow-up rate was 71.9% (374 of 520 shoulders).
All patients who had RP received injections containing a mixture of 3.3 mg of dexamethasone and 4 mL of 1% mepivacaine into the intra-articular space (in cases with contracture; passive elevation, < 130°) or into the subacromial bursa (for cases without contracture; with passive elevation, > 130°) until the RP had been resolved as much as possible. The patients were then divided into three groups: those who required several corticosteroid injections preoperatively because of refractory RP but the RP persisted (group A+), those whose RP had disappeared by the time of surgery (group A−), and those without RP who did not require any injections (group B).
To adjust for demographic characteristics, we then performed one-to-one propensity score matching based on sex and age. After matching, 266 patients (273 shoulders), comprising 145 men and 128 women with a mean age of 65.2 ± 7.7 years (range, 42 to 88 years) at the time of surgery, were included in the study (
Fig. 1). The final functional evaluation was performed at a mean of 29.6 ± 9.7 months (range, 24 to 73 months) after surgery. Surgery was performed in the dominant extremity in 186 shoulders and in the nondominant extremity in 87. There were 244 full-thickness tears, including 92 small (< 1 cm in length), 82 medium (1–3 cm), 66 large (3–5 cm), and four massive (> 5 cm) tears; and there were 29 partial-thickness tears (24 on the bursal side, four on the articular side, and one intratendinous).
Surgical Technique
All the operations were performed under general anesthesia in a beach chair position. Manipulation under anesthesia was carried out preoperatively in patients with contracture (passive elevation under anesthesia, < 130°: 19 cases in group A+, 18 in group A−, and 13 in group B). After standard posterior and anterior portals were established, initial assessment and treatment of the glenohumeral joint were carried out. The arthroscope was then transferred to the subacromial space. After anterolateral and posterolateral portals were established, subacromial decompression was performed as required. Cuff repairs were accomplished using a double-row or single-row fixation technique depending on the tear size and tendon mobility. On the double-row fixation procedure, after the medial row of suture anchors was inserted through the superolateral portal and located just lateral to the articular surface, number 2 permanent sutures were passed through the medial portion of the cuff in a mattress fashion. The lateral row of suture anchors was inserted through the superolateral or anterolateral portal and placed at the lateral ridge of the greater tuberosity, and sutures were passed through the lateral margin of the rotator cuff in a simple fashion. We performed knot-tying for the lateral row first; the repair was then completed with knot-tying for the medial row. On the single-row fixation procedure, we inserted the suture anchors at the lateral ridge of the greater tuberosity, and the sutures were then placed through the margin of the cuff in a simple fashion, followed by knot-tying.
Postoperative Protocol
After surgery, patients were immobilized in a sling for 3 weeks (for tears < 3 cm and partial-thickness tears) or by an immobilizer with an abduction pillow that allowed about 20° of abduction (for tears > 3 cm). On the day after surgery, all patients were encouraged to initiate isometric cuff exercise to the extent possible and muscle relaxation around the shoulder girdle. Three weeks after surgery, passive ROM exercises were initiated while avoiding provocation of pain. After 6 weeks, patients started strengthening exercises for the rotator cuff and were permitted to participate in light sports activities by 3 months postoperatively. Full return to sports and heavy labor was allowed after 6 months depending on the individual's functional recovery.
Definition of RP
There were various operative indications in the patients who participated in this study, including pain on movement and loss of power. Spontaneous pain at rest has been reported to be the most pestering complaint and is related to inflammation of the intra-articular or subacromial bursa.
91011) Therefore, in this study, RP was defined as aching pain during the day or at night that required anti-inflammatory medication and that disturbed sleep. Movement-related pain, such as pain felt immediately at the time of performing activity and compression pain when lying in a lateral position, was excluded. We carefully interviewed patients about the characteristics of their pain.
Patient Assessment
Patient's sex, and age, preoperative tear size (< 3 cm or ≥ 3 cm), and diabetes status were compared among the three groups. The duration of RP before the first injection and the interval between the final injection and the index surgery were compared between groups A+ and A−. The incidence of postoperative RP and the American Shoulder and Elbow Surgeons (ASES) score, including the pain score, activities of daily living (ADL) score, and total ASES score preoperatively and 2 years after surgery (final ASES score), were evaluated in each group. The preoperative and final ASES scores were also subjected to linear correlation analysis. All patients were assessed by the same examiner for ROM, including forward flexion (FF) and side-lying external rotation (ER), preoperatively and at 3 and 24 months postoperatively. Magnetic resonance imaging (MRI) was performed 1 year after surgery, and the findings were classified according to the system proposed by Sugaya et al.
12) Types IV and V were considered to be retears. The retear rate was compared among the groups. The number of patients who received intra-articular and subacromial bursa injections and their mean total ASES scores were compared.
Statistical Analysis
Demographic data, sex, preoperative tear size, and diabetes status were compared between the groups using the chi-square test. Age was compared among the groups using one-way analysis of variance. The duration of RP before the first injection and the interval between the final injection and the index surgery were compared between groups A+ and A− using the Mann-Whitney U-test.
The incidence of postoperative RP was compared between the groups using the chi-square test and a post-hoc test with Bonferroni's correction. The preoperative and final ASES scores and the FF and ER values at each assessment session were compared using analysis of variance with Tukey's post-hoc test. The preoperative and final ASES scores was also analyzed using Pearson's correlation. The rotator cuff retear rate and the number of injections at each site were compared among the groups using the chi-square test. ASES scores were compared according to the injection site using the Mann-Whitney U-test. A post-hoc test was performed only when a significant difference was detected between the groups using an overall test. A p-value < 0.05 was considered statistically significant.
RESULTS
Demographic Data
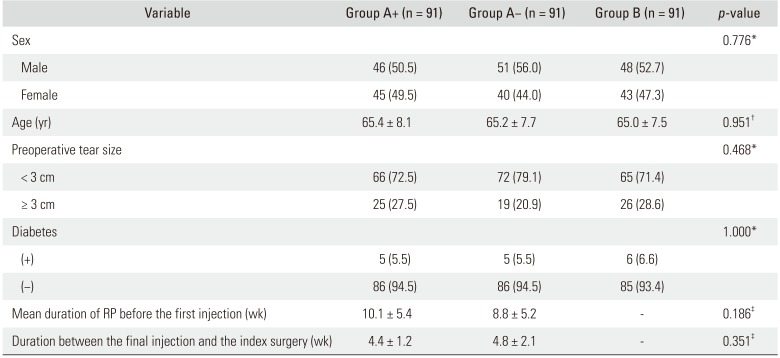
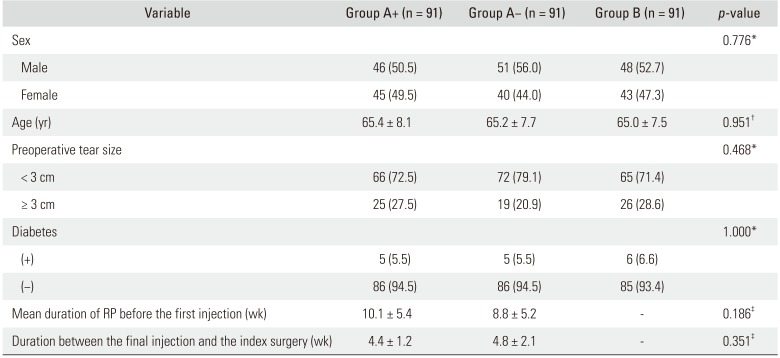
There were 91 patients in each of the three groups: 46 men (50.5%) in group A+, 51 men (56.0%) in group A−, and 48 men (52.7%) in group B; the mean ages were 65.4 ± 8.1 years, 65.2 ± 7.7 years, and 65.0 ± 7.5 years, respectively. The preoperative tear size was small (< 3 cm) in 66 patients (72.5%) in group A+, in 72 (79.1%) in group A−, and in 65 (71.4%) in group B. Diabetes was present in five patients (5.5%) in group A+, in five (5.5%) in group A−, and in six (6.6%) in group B. Mean duration of RP before the first injection was 10.1 ± 5.4 weeks in group A+ and 8.8 ± 5.2 weeks in group A−. The mean interval between the final injection and the index surgery was 4.4 ± 1.2 weeks in group A+ and 4.8 ± 2.1 weeks in group A−. There was no significant difference in sex, age, preoperative tear size, diabetes status, duration of RP, and the interval between the final injection and the index surgery (
p = 0.776,
p = 0.951,
p = 0.468,
p = 1.000,
p = 0.186, and
p = 0.351, respectively) between the groups (
Table 1).
Comparison of the Incidence of Postoperative RP
Incidences of postoperative RP were as follows: group A+, 35 of 91 cases (38.5%); group A−, 10 of 91 cases (11.0%); and group B, seven of 91 cases (7.7%). The incidence was significantly higher in group A+ than in group A− (p < 0.001) or group B (p < 0.001); however, there was no significant difference in the incidence between group A− and group B (p = 0.612).
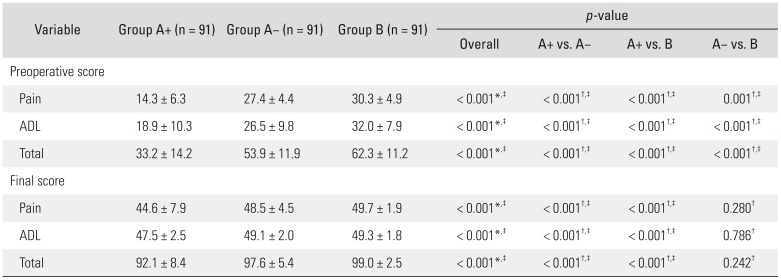
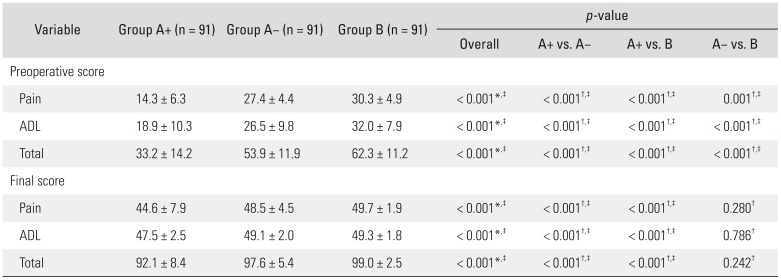
Comparison of Preoperative and Final ASES Scores
Mean preoperative ASES pain scores were 14.3 ± 6.3 in group A+, 27.4 ± 4.4 in group A−, and 30.3 ± 4.9 in group B; the mean preoperative ADL scores were 18.9 ± 10.3, 26.5 ± 9.8, and 32.0 ± 7.9, respectively, and the total preoperative scores were 33.2 ± 14.2, 53.9 ± 11.9, and 62.3 ± 11.2, respectively. All scores were significantly lower in group A+ than in group A− and group B (p < 0.001 for all); scores in group A− were significantly lower than those in group B (mean pain score, p = 0.001; ADL and total scores, p < 0.001).
Mean final ASES pain scores were 44.6 ± 7.9 in group A+, 48.5 ± 4.5 in group A−, and 49.7 ± 1.9 in group B; the mean final ADL scores were 47.5 ± 2.5, 49.1 ± 2.0, and 49.3 ± 1.8, respectively, and the mean final total scores were 92.1 ± 8.4, 97.6 ± 5.4, and 99.0 ± 2.5, respectively. All scores in group A+ were significantly lower than those in group A− and group B (
p < 0.001 for all). However, there was no significant difference in the pain score (
p = 0.280), ADL score (
p = 0.786), and total score (
p = 0.242) between group A− and group B (
Table 2).
With regard to linear correlations between the preoperative and final ASES scores, the correlation coefficients were as follows: pain score (r = 0.391, p < 0.001), ADL score (r = 0.226, p < 0.001), and total score (r = 0.434, p < 0.001). The pain and total scores showed weak or moderate correlations.
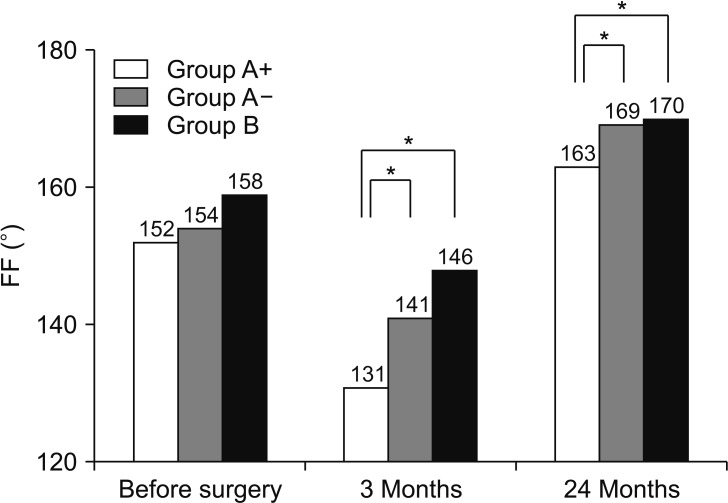
Comparison of FF and ER during the Disease Course
Mean FF values preoperatively and at 3 and 24 months after surgery were 152° ± 25°, 131° ± 28°, and 163° ± 13°, respectively, in group A+, 154° ± 23°, 141° ± 21°, and 169° ± 6°, respectively, in group A−, and 158° ± 24°, 146° ± 21°, and 170° ± 7°, respectively, in group B. There were no significant intergroup differences preoperatively (
p = 0.276). The postoperative
p-values were as follows:
p = 0.022 for A+ vs. A−,
p < 0.001 for A+ vs. B, and
p = 1.000 for A− vs. B at 3 months;
p < 0.001 for A+ vs. A−,
p < 0.001 for A+ vs. B, and
p = 1.000 for A− vs. B at 24 months after surgery. FF values at 24 months after surgery were significantly higher in group A− and group B than in group A+; however, there was no significant difference between group A− and group B (
Fig. 2).
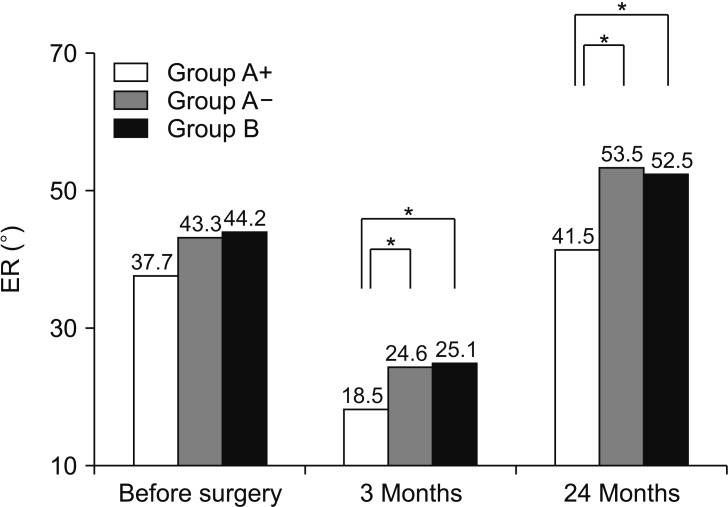
Mean ER values preoperatively and at 3 and 24 months after surgery were 37.7° ± 20.5°, 18.5° ± 16.2°, and 41.5° ± 16.1°, respectively, in group A+, 43.3° ± 17.5°, 24.6° ± 13.8°, and 53.5° ± 12.0°, respectively, in group A−, and 44.2° ± 16.9°, 25.1° ± 14.6°, and 52.5° ± 14.0°, respectively, in group B. There were no significant intergroup differences preoperatively (
p = 0.086). The postoperative
p-values were as follows:
p = 0.018 for A+ vs. A−,
p = 0.010 for A+ vs. B, and
p = 1.000 for A− vs. B at 3 months;
p < 0.001 for A+ vs. A−,
p < 0.001 for A+ vs. B, and
p = 1.000 for A− vs. B at 24 months after surgery. ER values at 24 months after surgery were significantly higher in group A− and group B than in group A+; there was no significant difference between group A− and group B (
Fig. 3).
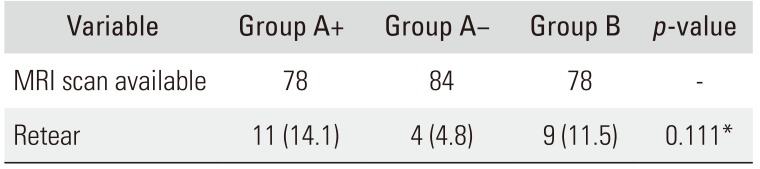
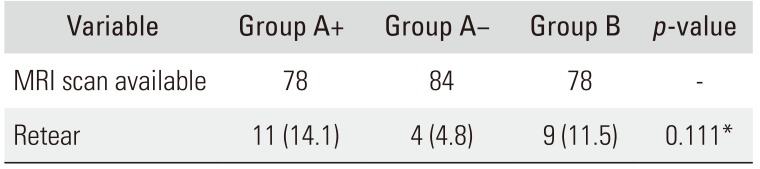
Comparison of Complications, Including Retear Rate
MRI was performed on 240 shoulders at 1 year after surgery. Using the system devised by Sugaya et al.,
12) 129 shoulders were classified as type I; 71, as type II; 16, as type III; 13, as type IV; and 11, as type V. Considering types IV and V as retears, we found retear cases in 24 shoulders (10.0%). The retear rate was 14.1% (11/78) in group A+, 4.8% (4/84) in group A−, and 11.5% (9/78) in group B; there were no significant intergroup differences in the retear rate (
p = 0.111) (
Table 3). There were no cases of injection-related infection.
Comparison between Intra-articular and Subacromial Bursa Injections
Preoperatively, 27 intra-articular injections (29.7%) were administered in group A+ and 15 (16.5%), in group A−; 64 (70.3%) subacromial bursa injections were administered in group A+ and 76 (83.5%), in group A− (p = 0.052). Mean total ASES scores after intra-articular and subacromial bursa injections were as follows: 29.5 ± 14.3 and 34.8 ± 14.0, respectively, preoperatively (p = 0.100) and 88.0 ± 9.0 and 93.8 ± 7.5, respectively, finally in group A+ (p = 0.001); 52.9 ± 11.1 and 54.1 ± 12.1, respectively, preoperatively (p = 0.885) and 96.5 ± 7 .2 and 97.8 ± 4.9, respectively finally in group A− (p = 0.971).
DISCUSSION
RP is one of the most persistent symptoms in patients with rotator cuff injury and is often an important indication for surgery. Various theories have been put forward to explain the etiology of RP, with night pain reported by many authors. Okamura et al.
9) investigated synovial fluid specimens from the shoulder joints of 38 patients with rotator cuff injury and reported an association of the visual analog scale scores at rest and at night with the interleukin-8 level in joint fluid. Santavirta et al.
10) investigated 12 patients who underwent acromioplasty and reported that pain experienced at rest and at night was a result of clinical inflammation in tissues other than the bursa. Therefore, there may be a relationship between RP and inflammation in the shoulder joint. However, there are a number of reports on the efficacy of corticosteroid injection for this type of inflammation. Lee et al.
7) evaluated subacromial bursitis on ultrasonography in 69 patients with rotator cuff injury and reported that corticosteroid injections could be expected to be more effective in patients with subacromial bursitis than in those with a normal bursa. Furthermore, a number of authors have reported the efficacy of corticosteroid injections into the intra-articular
56) and subacromial
8) bursa in patients with rotator cuff injury.
A variety of factors that can affect the outcome after ARCR have been reported, including the suture method used,
13) presence of diabetes,
14) preoperative contracture,
15) and postoperative physiotherapy.
1617) The presence of persistent pain during the perioperative period would also affect the final outcome. However, few studies have reported on the correlation between RP before and after surgery or between preoperative RP and the clinical outcome. In this study, the incidence rate of postoperative RP in group A+ reached nearly 40%, which was significantly higher than the values in group A− and group B; the incidence rate in group A− was less than 10%, not significantly different from that in group B. Therefore, preoperative pain control is important for reduction of the risk of postoperative RP.
Although the preoperative ASES (pain, ADL, and total) scores were significantly lower in group A− than in group B, there was no significant difference in the final scores between these two groups. However, both the preoperative scores and the final scores in group A+ were significantly lower than those in group A− and group B. Therefore, in shoulders with preoperative RP, provided that effective pain control is achieved, the final ASES score may be equivalent to that in shoulders without preoperative RP. In contrast, patients in whom preoperative RP was refractory tended to have inferior final outcomes. For patients with preoperative RP, effective pain control before surgery is considered to be important in terms of not only pain relief but also ADL.
FF and ER values were significantly lower in group A+ than in group A− and group B by 24 months after surgery. Therefore, patients in whom RP could not be fully resolved before surgery had an inferior outcome in terms of final ROM; however, if their RP could be improved preoperatively, they would be able to achieve an ROM (in both FF and ER) equivalent to that in patients without preoperative RP.
Bhatia et al.
18) administered subacromial corticosteroid injections to 230 patients with subacromial impingement syndrome, grouped them according to whether they received less than three or three or more injections, and found no significant difference in findings of rotator cuff damage on MRI between the two groups. In the present study, there was no significant difference in rotator cuff retear rate between the three groups, which also suggests that use of corticosteroid injections to control RP should not be considered a causative factor in rotator cuff damage.
In this study, intra-articular corticosteroid injections were administered for patients with RP and contracture and subacromial bursa corticosteroid injections for those without contracture. It seems reasonable that ASES scores would tend to be lower in patients who require intra-articular injections than in those who need subacromial bursa injections because the latter did not have contracture. However, while the difference was significant in group A+, it was barely noticeable in group A− at 24 months postoperatively. Therefore, patients whose RP could be controlled by corticosteroid injections can be expected to have good results regardless of whether or not contracture is present.
Preoperative pain control is important in patients with rotator cuff injury and RP. Providing that RP can be improved preoperatively, the outcome of ARCR in these patients should be similar to that in patients who do not have preoperative RP without an increase in the retear rate. However, corticosteroid injection is still controversial in terms of the risk of infection and tendon healing. Although there were no injection-related infections and no increase in the retear rate in this study, further research is needed to investigate these complications.
There are several limitations to this study. First, there were no clinical evaluation data, such as the ASES score before the first injection, so whether or not there was a difference in the initial severity of inflammation between group A+ and group A− is unclear. Second, almost 28% of the patients were lost to follow-up. Finally, the severity of RP was not assessed objectively using, for example, a visual analog scale.
In summary, patients in whom preoperative RP could be resolved before surgery achieved postoperative outcomes comparable to those in patients who had not experienced any RP before surgery, whereas the outcomes in patients with refractory preoperative RP were inferior. Our results suggest preoperative pain control is important in patients undergoing ARCR.
Fig. 1
Flowchart of patient enrollment and follow-up.
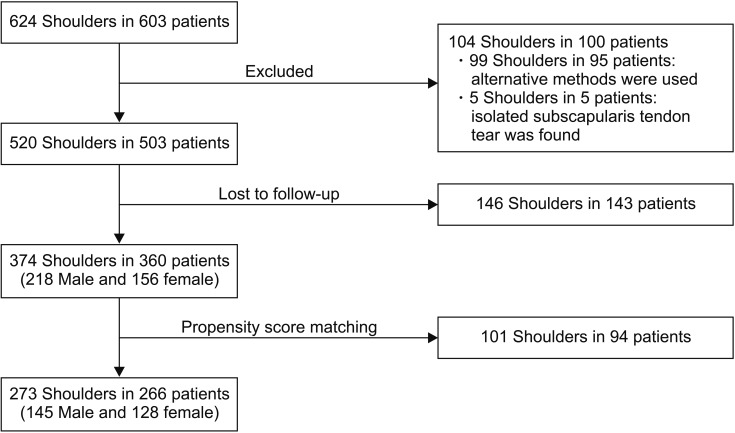
Fig. 2
Comparison of forward flexion (FF) preoperatively and at 3 and 24 months after surgery. FF value at 24 months after surgery is significantly higher in group A− and group B than that in group A+ with no significant difference between group A− and group B. Group A+: those who required several corticosteroid injections preoperatively because of refractory RP but the RP persisted, Group A−: those whose RP had disappeared by the time of surgery, Group B: those without RP who did not require any injections, RP: rest pain. *p < 0.05.
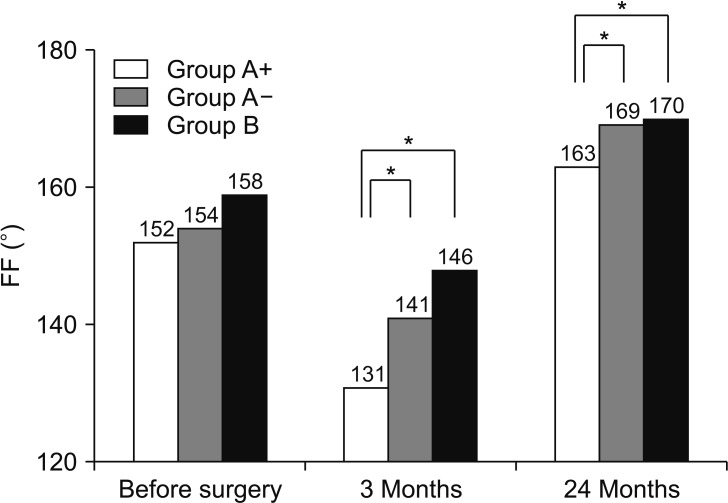
Fig. 3
Comparison of side-lying external rotation (ER) preoperatively and at 3 and 24 months after surgery. ER value at 24 months after surgery is significantly higher in group A− and group B than that in group A+ with no significant difference between group A− and group B. Group A+: those who required several corticosteroid injections preoperatively because of refractory RP but the RP persisted, Group A−: those whose RP had disappeared by the time of surgery, Group B: those without RP who did not require any injections, RP: rest pain. *p < 0.05.
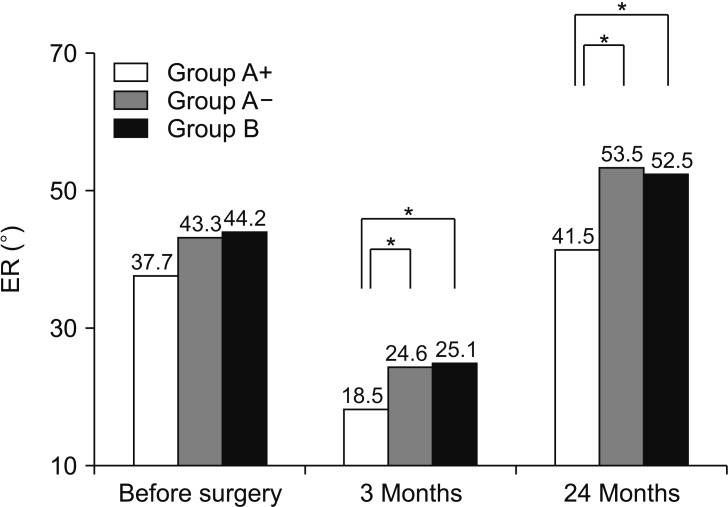
Table 1
Preoperative Patient Clinical and Demographic Data
|
Variable |
Group A+ (n = 91) |
Group A− (n = 91) |
Group B (n = 91) |
p-value |
|
Sex |
|
|
|
0.776*
|
|
Male |
46 (50.5) |
51 (56.0) |
48 (52.7) |
|
|
Female |
45 (49.5) |
40 (44.0) |
43 (47.3) |
|
|
Age (yr) |
65.4 ± 8.1 |
65.2 ± 7.7 |
65.0 ± 7.5 |
0.951†
|
|
Preoperative tear size |
|
|
|
0.468*
|
|
< 3 cm |
66 (72.5) |
72 (79.1) |
65 (71.4) |
|
|
≥ 3 cm |
25 (27.5) |
19 (20.9) |
26 (28.6) |
|
|
Diabetes |
|
|
|
1.000*
|
|
(+) |
5 (5.5) |
5 (5.5) |
6 (6.6) |
|
|
(−) |
86 (94.5) |
86 (94.5) |
85 (93.4) |
|
|
Mean duration of RP before the first injection (wk) |
10.1 ± 5.4 |
8.8 ± 5.2 |
- |
0.186‡
|
|
Duration between the final injection and the index surgery (wk) |
4.4 ± 1.2 |
4.8 ± 2.1 |
- |
0.351‡
|
Table 2
Preoperative and Final ASES Scores According to Groups
|
Variable |
Group A+ (n = 91) |
Group A− (n = 91) |
Group B (n = 91) |
p-value |
|
Overall |
A+ vs. A− |
A+ vs. B |
A− vs. B |
|
Preoperative score |
|
|
|
|
|
|
|
|
Pain |
14.3 ± 6.3 |
27.4 ± 4.4 |
30.3 ± 4.9 |
< 0.001*,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
|
ADL |
18.9 ± 10.3 |
26.5 ± 9.8 |
32.0 ± 7.9 |
< 0.001*,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
|
Total |
33.2 ± 14.2 |
53.9 ± 11.9 |
62.3 ± 11.2 |
< 0.001*,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
|
Final score |
|
|
|
|
|
|
|
|
Pain |
44.6 ± 7.9 |
48.5 ± 4.5 |
49.7 ± 1.9 |
< 0.001*,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
0.280†
|
|
ADL |
47.5 ± 2.5 |
49.1 ± 2.0 |
49.3 ± 1.8 |
< 0.001*,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
0.786†
|
|
Total |
92.1 ± 8.4 |
97.6 ± 5.4 |
99.0 ± 2.5 |
< 0.001*,‡
|
< 0.001†,‡
|
< 0.001†,‡
|
0.242†
|
Table 3
Retear of Rotator Cuff in Each Group at 1 Year after Surgery
|
Variable |
Group A+ |
Group A− |
Group B |
p-value |
|
MRI scan available |
78 |
84 |
78 |
- |
|
Retear |
11 (14.1) |
4 (4.8) |
9 (11.5) |
0.111*
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download