Abstract
Background
Treatment of unstable clavicle fractures remains a challenge for orthopedic surgeons, but the evolution of treatment strategies has allowed for reliable results with minimal complications. Although several surgical options exist, open reduction with plating remains the treatment of choice for clavicle fractures. The purpose of this study is to determine an easy way to achieve successful preplating reduction while minimizing surrounding soft tissue damage during treatment of midshaft fractures of the clavicle.
Methods
A retrospective study included all consecutive adult patients operated on by a single surgeon for acute displaced clavicular midshaft fracture between January 2010 and October 2014. Hybrid technique with interfragmentary cerclage wiring, temporary axial K-wire pinning, or their combination was used in all patients. The demographic data and clinical outcomes, including operation time, union time, restoration of anatomy, shoulder functional score, and complications were evaluated.
Results
There were 54 male and 19 female patients, with an average age of 39.3 years (range, 18 to 77 years) for males and 58.3 years (range, 39 to 77 years) for females. They were followed up for 24 months (range, 12 to 44 months). All patients had reliable bone union after surgery using interfragmentary cerclage wiring and temporary axial K-wire fixation; fracture union was obtained at an average of 11.7 weeks (range, 8 to 21 weeks) postoperatively. Additionally, there was no postoperative loss of fracture reduction or plate loosening. At the final follow-up, all patients had regained excellent functional outcomes.
Conclusions
The cognizant effort to achieve anatomic reduction without surrounding soft tissue insult before definitive plating allows excellent radiologic and functional outcomes. Interfragmentary cerclage wiring and temporary axial K-wire pinning can overcome difficulties associated with unstable clavicle fractures to allow proper fracture reduction. In this article, we introduce a concise technique for achieving the desired outcomes reliably and efficiently when treating unstable clavicle midshaft fractures.
Clavicle shaft fractures can happen with various fracture patterns, from simple transverse fractures to comminuted and unstable configurations. When midshaft clavicle fractures are significantly displaced or comminuted, poor outcomes, such as nonunion, and cosmetic issues may occur at a markedly higher rate, especially in young and active patients.12) Therefore, accurate restoration of the fractured clavicle is of paramount steps in the operative procedure. Although some surgeons have proposed surgical stabilization of these types of complex midshaft clavicle fractures with various internal fixation devices, complications such as nonunion, malunion, delayed union, metal failure, and infection from the surgical treatment may inevitably result. During the operation, unintentional soft tissue insults and subperiosteal stripping around the fracture site may disrupt the bone and soft tissue healing process. Thus, we devised our own surgical techniques by combining anatomical locking bridging plates with temporary axial Kwire pinning, interfragmentary cerclage wiring, or their combinations. These techniques not only help with maintenance of reduction but also minimize the damage to the surrounding soft tissue as well.
The protocol of this study was approved by Institutional Review Board of Gumi CHA Hospital (IRB No. 2017- 17) and performed in accordance with the principles of the Declaration of Helsinki. Seventy-three patients older than 18 years of age with unstable midshaft fractures who underwent operations performed by a single surgeon (JD) between January 2010 and October 2014 were enrolled in this study. All the patients had a displacement of > 2 cm, shortening of > 2 cm, or significant comminution after injury. Exclusion criteria were fractures in the medial or lateral one-third of the clavicle, pathological fracture, open fracture, and concomitant ipsilateral upper extremity injury. Surgical fixation with interfragmentary cerclage wiring, temporary axial K-wire pinning, or their combination was employed in all patients (Fig. 1). In all cases, we used anatomical plates (Depuy Synthes, Zuchwil, Switzerland) because they are anatomically precontoured and have more options for lateral screw positions.
We placed the patient in the supine position on a radiolucent table under general anesthesia, as proper positioning of the patient is necessary for achieving anatomic reduction. A rolled towel was placed below the interscapular area so that we could partially reduce the shortened and displaced fragment. On the fracture site, the curvilinear longitudinal incision was made along the upper side of the clavicle, and the subcutaneous tissue and fascia were dissected, preserving the supraclavicular nerve as much as possible. Then, the fracture site was exposed with minimal dissection of the surrounding soft tissues. If the fracture was shortened or comminuted, we first pulled both sides of the main fracture's ends with a clamp to obtain general alignment and then bound the fragments with several interfragmentary cerclage wires (Fig. 2).
After the cerclage wires were passed through the fragments and the surrounding soft tissue, each end of the wire was tightened with each other using gentle tension; there is no need to tighten the wires too strongly, because we need only the strength to maintain the reduction throughout the whole procedure and, also, the wires should not be tightened too hard to maintain periosteal blood flow. This procedure substantially changed the comminuted fracture to a simple fracture and provided stability during definitive fixation. After this procedure, the anatomical locking plate was placed to fix the main fracture segments. The plate should have at least three locking screws at each end to neutralize and protect against deforming forces (Fig. 3). During the procedure, interfragmentary cerclage wires have low profiles, so they do not interfere with placement of the precontoured locking plate on the upper surface of the clavicle.
In other cases of displaced transverse fracture, we used temporary intramedullary axial K-wire pinning. For this technique, a K-wire with a diameter of 1.5 mm or 2.0 mm was inserted in a retrograde manner into the medullary cavity of the distal fragment and advanced laterally to penetrate the posterior cortex of the lateral curve, deltoid muscle, and skin. Then, the K-wire was retracted from the lateral end until the medial end of the wire reached the medial end of the lateral fracture fragment. After the fracture had been reduced, the K-wire was advanced in an anterograde manner into the medial fragment to maintain the fracture reduction (Fig. 4). Intramedullary K-wire pinning can provide stability during definitive fixation.
Next, an anatomical plate was placed on the upper surface of the clavicle. The K-wire was removed after each locking screw was placed into the most distal and proximal holes. If the intramedullary K-wire affected the placement of the first screw in the most proximal holes, a short, single cortical locking screw was placed first and then eventually replaced with a bicortical locking screw.
In the postoperative period, the extremity was immobilized in a sling for 3 weeks, during which, in order to prevent the stiffness, active range of motion exercises for the elbow and shoulder pendulum movement exercises were encouraged. Three weeks after surgery, passive mobilization of the shoulder was increased while gradually transitioning to active exercises. Strength training was started after radiological and clinical healing had been achieved.
All patients were asked for follow-up monthly after surgery until fracture union, and then every 3 to 6 months after radiographic union. The duration of surgery and blood loss during the procedure were recorded. Functional evaluation was made using a visual analogue scale, the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire, University of California at Los Angeles (UCLA) Shoulder Score, and the Constant Shoulder Score (CSS). Postoperative complications that were documented included hypoesthesia, infection, nonunion, and implant failure. A total of 76.7% of the patients (56/73) underwent a second surgery to remove the implant, which was nonmandatory and done at the patient's request.
This study enrolled 54 male and 19 female patients. The mean age at the time of surgery was 39.3 years (range, 18 to 77 years) for males and 58.3 years (range, 39 to 77 years) for females. Thirty-nine patients were involved in low energy injury such as fall down and direct blow, and 34 patients were involved in traffic accidents and high-level falls. The mean follow-up period was 24 months (range, 12 to 44 months). Based on the Orthopedic Trauma Association fracture classification system, 30 patients were classified as type 15.2A, 19 as type 15.2B, and 24 as type 15.2C.
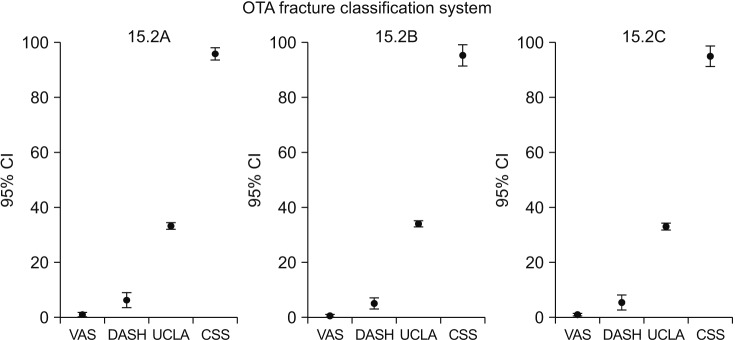
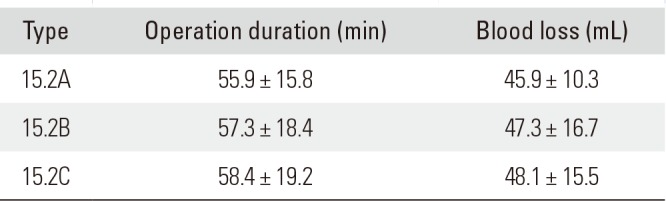
The average time between injury and surgery was 3.6 days (range, 1 to 10 days). Among 73 patients, 45 patients were reduced with interfragmentary cerclage wires, 11 patients with temporary intramedullary axial K-wire pinning, and 17 patients with both techniques. All patients had reliable bone union after surgery, and the fracture union was obtained at an average 11.7 weeks postoperatively (range, 8 to 21 weeks). The mean surgery duration and blood loss in the subgroups are shown in Table 1. There were no significant difference between the subgroups (p > 0.05). The length of both clavicles was measured to evaluate anatomic restoration after bone union, and their comparative lengths were recorded as the length ratios. The length ratios were all within 5% of the length (95% to 105%) of the other clavicle at their last follow-up. Additionally, there was no postoperative loss of fracture reduction or plate loosening, which might have caused malunion or late deformity. At the final follow-up, they did not present with postoperative complications related to surgical intervention itself, such as infection and implant issues, except for a few cases of paresthesia. Numbness over the incision was noted in seven patients, but it did not limit normal daily activity. Neither any serious neurovascular impairment nor pulmonary injury was noted postoperatively.
One patient experienced metal breakage from another traffic accident 3 months after the initial surgery for the clavicle fracture. He was subsequently treated with repeat open reduction and plating. The overall functional results were excellent in the majority of patients, and there were no significant subgroup differences in visual analogue scale, DASH, UCLA Shoulder Scores, and CSS at the final follow-up (Fig. 5).
Fractures of the clavicle account for 2.6%–4% of all fractures. The vast majority (69%–82%) of these fractures are located in the midshaft of the clavicle.3) The treatment of clavicle fractures is aimed at quickly restoring function to the upper extremity and preventing disability.45)
Previous studies6) indicate that nonunion rates are higher than expected and that malunions are associated with poor outcomes. Hill et al.6) reviewed patients with completely displaced middle third clavicular fractures, and the overall results could be regarded as satisfactory, but the 15% incidence of nonunion was strongly associated with an unsatisfactory result, as was the initial shortening of ≥ 20 mm. There was also a relatively high incidence of other problems, including pain and nerve compression syndromes.78)
Recent high-quality randomized clinical trials, demonstrating superior functional outcomes in the surgical group, have revived interest in surgical fixation of this fracture in a certain group of patients.910) Currently, there is a growing trend toward treating displaced midshaft clavicle fractures with primary open reduction and internal fixation.9111213) Plate fixation is biomechanically superior to intramedullary fixation, and it can allow full range of motion by providing rigid fixation, which is favorable for early rehabilitation protocol,14) but they require longer incisions and more extensive soft tissue stripping.15) Also, implant failures, including plate bending, plate breakage, or screw pullout, may occur in 14% of patients.16)
According to van der Ven Denise et al.'s report,12) although patient satisfaction was higher in the operative group compared to the conservative group, more complications and a higher rate of physical complaints were seen in the operative group. These undesirable consequences, such as nonunion and infection, were due to operation-specific complications (i.e., implant-related and operative techniques), which could not occur in the non-operative treatment group.15)
To avoid operation-related complications and improve outcomes, we consider that minimal soft tissue handling and neutralizing excessive deforming forces are the key priorities of the procedure. When a clavicle midshaft fracture occurs, the surrounding muscles and gravity pull and rotate the fragments, and thus leads to shortening of the shoulder girdle. Excessive deforming forces are what make achieving initial reduction difficult and are the reasons for fixation failure and mal-reduction that commonly occur after surgery.17)
We introduced a technique that can minimize soft tissue injury, maintain the initial reduction and neutralize deforming forces. First, we performed an indirect reduction of the main fracture ends by elevating the upper arm, and then used intramedullary K-wires or interfragmentary cerclage wiring techniques to fix main fracture fragments temporarily to maintain the reduction. These procedures have shown to facilitate temporary reduction and simplify surgery. Some surgeons recommend using interfragmentary lag screws to fix comminuted fragments and simplify complex fractures.15) However, we did not use this technique because using lag screws may cause iatrogenic soft tissue damage, such as periosteal stripping. We only stripped the superior surface of the clavicle to protect the soft tissue attachment and blood supply, and we bound the comminuted fragments and surrounding soft tissue together with cerclage wire. The reduction of displaced fragments can be relatively simple, and we can precisely settle their original position by gentle tightening of wires. Interfragmentary cerclage wire fixation has raised some concerns about excessive compression that might reduce periosteal blood circulation and interfere with the fracture healing. However, Yum et al.18) reviewed patients who had undergone cerclage wire fixation and concluded that the procedure does not influence bone healing and that the procedure should be considered safe and satisfactory.
Finally, we applied anatomical locking plates of appropriate length to bridge the main fracture. The anatomical locking plates are offset from the surface of the bone, as the screws do not need to compress the plate to the bone to maintain fixation, which may simplify surgery, allow for rigid fixation of a butterfly fragment, and protect the periosteal blood supply.1920) A locking bridging plate may preserve blood supply to the bone, and sufficient stress resistance to implant failures and can allow full range of motion by providing rigid fixation, which is favorable for early rehabilitation protocols.2021)
The authors do recognize the retrospective nature of this study. Although authors analyzed the subgroups, there was no alternative treatment or control group with which to compare results. Future work is needed to conduct a prospective, randomly controlled study with a longer follow- up to fully analyze and understand clinical outcomes. It also remains to be shown which surgical method may best address different patient groups and fracture types. However, despite the relatively small number of patients, radiologic and functional results were favorable, and complications, such as malunion, delayed union, and deep infection, were not observed. Our results demonstrate that these surgical techniques are safe, simple, effective, and practical and lead to rapid recovery, a high rate of union, and excellent functional and anatomic restoration.
Treatment of unstable midshaft clavicular fractures remains a challenge, but with technological advancements, reliable results with low complications can be obtained. Using interfragmentary cerclage wiring and temporary axial K-wire pinning before plate fixation to aid reduction can simplify surgery and protect the surrounding soft tissue from damage. Our study revealed that these soft tissue-friendly procedures facilitate the surgical process and make complex fractures into a simple fracture for improved handling as well as minimal complications.
References
1. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012; 94(8):675–684. PMID: 22419410.

2. Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: a prospective study of 222 patients. Acta Orthop. 2005; 76(4):496–502. PMID: 16195064.
3. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002; 11(5):452–456. PMID: 12378163.

5. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968; 58:29–42. PMID: 5666865.
6. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997; 79(4):537–539. PMID: 9250733.

7. Jeray KJ. Acute midshaft clavicular fracture. J Am Acad Orthop Surg. 2007; 15(4):239–248. PMID: 17426295.

8. Wijdicks FJ, Van der, Millett PJ, Verleisdonk EJ, Houwert RM. Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg. 2012; 132(5):617–625. PMID: 22237694.

9. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007; 89(1):1–10.
10. Lenza M, Belloti JC, Andriolo RB, Faloppa F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev. 2014; (5):CD007121. PMID: 24879341.

11. Smekal V, Oberladstaetter J, Struve P, Krappinger D. Shaft fractures of the clavicle: current concepts. Arch Orthop Trauma Surg. 2009; 129(6):807–815. PMID: 18989685.

12. van der Ven Denise JC, Timmers TK, Flikweert PE, Van Ijseldijk AL, van Olden GD. Plate fixation versus conservative treatment of displaced midshaft clavicle fractures: functional outcome and patients' satisfaction during a mean follow-up of 5 years. Injury. 2015; 46(11):2223–2229. PMID: 26315667.

13. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013; 95(17):1576–1584. PMID: 24005198.
14. Golish SR, Oliviero JA, Francke EI, Miller MD. A biomechanical study of plate versus intramedullary devices for midshaft clavicle fixation. J Orthop Surg Res. 2008; 3:28. PMID: 18631380.

15. Naderipour A, McKee MD. Precontoured plate fixation with interfragmentary lag screw use in a middle third clavicle fracture fixation. J Orthop Trauma. 2015; 7. 28. [Epub]. DOI: 10.1097/BOT.0000000000000402.

16. Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma. 1997; 43(5):778–783. PMID: 9390489.

17. Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture: a clinical and biomechanical analysis. J Bone Joint Surg Br. 1988; 70(3):461–464. PMID: 3372571.

18. Yum JK, Shin YW, Lee HS, Park JG. Does interfragmentary cerclage wire fixation in clavicle shaft fracture interfere the fracture healing? J Korean Fract Soc. 2011; 24(2):138–143.

19. Celestre P, Roberston C, Mahar A, Oka R, Meunier M, Schwartz A. Biomechanical evaluation of clavicle fracture plating techniques: does a locking plate provide improved stability? J Orthop Trauma. 2008; 22(4):241–247. PMID: 18404033.

20. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004; 18(8):488–493. PMID: 15475843.

21. Kontautas E, Pijadin A, Vilkauskas A, Domeika A. Biomechanical aspects of locking reconstruction plate positioning in osteosynthesis of transverse clavicle fracture. Medicina (Kaunas). 2012; 48(2):80–83. PMID: 22491383.

Fig. 1
(A) An unstable clavicle fracture with displaced, wedge-shaped fragments reduced with the combined technique of interfragmentary cerclage wiring and temporary axial K-wire pinning. The temporary axial K-wire penetrated the posterior cortex of the lateral curve. (B) Fluoroscopic image showing satisfactory reduction.
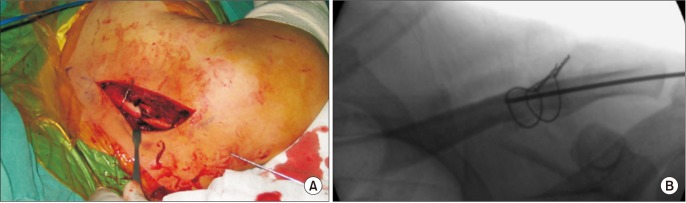
Fig. 2
(A) A wire passer was used to deliver thin wires under the fracture fragment with the surrounding soft tissue. Significant care was taken to minimize soft tissue injury. (B) Fluoroscopic image showing the position of the wire passer.
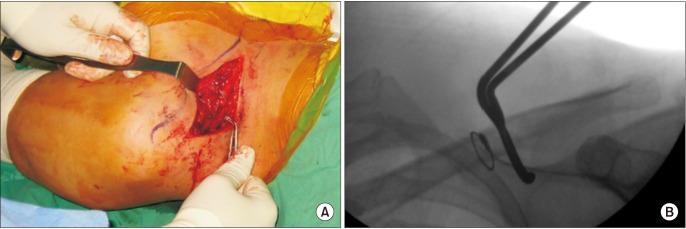
Fig. 3
(A) The cerclage wires between the clavicle and the anatomical plate were not obstacles for proper plate placement. (B) Fluoroscopic image showing the position of the wires and plate.
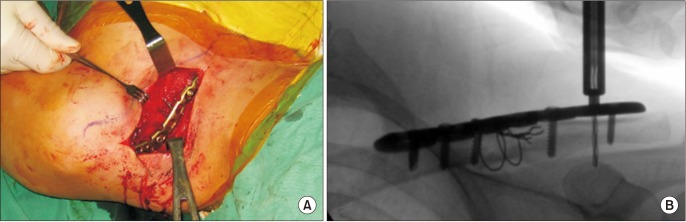
Fig. 4
The K-wire was retracted from the lateral fracture fragment through the skin until the medial end of K-wire reached the medial end of the lateral fracture fragment. After the fracture was reduced, the K-wire was further advanced into the medial fracture fragment.
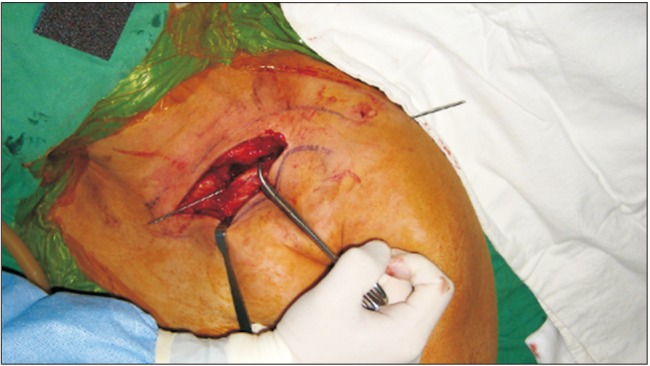
Fig. 5
Error bar graphs showing the functional results. The subgroups' clinical scores showed no statistically significant difference (p > 0.05). The error bars indicate 95% confidence intervals (CIs). OTA: Orthopedic Trauma Association, VAS: visual analogue scale, DASH: Disabilities of the Arm, Shoulder, and Hand, UCLA: University of California at Los Angeles Shoulder Score, CSS: Constant VAS DASH UCLA CSS Shoulder Score.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download