Abstract
Background
Persistent pain after total knee arthroplasty (TKA) is dissatisfying to the patient and frustrating to the surgeon. The purpose of this study is to evaluate the aseptic causes and clinical course of intractable pain following TKA.
Methods
Of the total 2,534 cases of primary TKA reviewed, 178 cases were classified as having aseptic persistent pain that was not resolved within 1 year after surgery. Except for the cases with periprosthetic fracture (56 knees), 122 cases of aseptic painful TKA were divided into two groups: intra-articular group (83 knees) and extra-articular group (39 knees).
Results
In the intra-articular group, the main reasons for pain were aseptic loosening (n = 40), polyethylene wear (n = 16), instability (n = 10), recurrent hemarthrosis (n = 5), patellar maltracking (n = 4), tendon ruptures (n = 4), and stiffness (n = 2). In the extraarticular group, 10 knees (25.6%) were found to have nerve entrapment in the spine, 6 knees (15.4%) were found to have hip osteoarthritis or femoral head avascular necrosis. The reasons for persistent knee pain in the remaining 23 knees (59.0%) still remain elusive.
Conclusions
Persistent pain after TKA originated from pathology of extra-articular origin in a considerable number of cases in this study. Therefore, it is important to perform thorough preoperative evaluations to reduce pain resulting from extra-articular causes. Furthermore, meticulous surgical procedures and optimal alignment are required to reduce pain of intra-articular origin related to implant wear, instability, and patellar maltracking.
The main goal of patients undergoing total knee arthroplasty (TKA) is to walk freely without pain. TKA has been performed with increasing frequency due to aging and economic development, and it has provided successful results with improvement of prostheses and surgical techniques. 12) Although TKA generally offers good pain relief for patients with end-stage knee arthritis, up to 20% patients complain of persisting pain.34) This persistent pain after TKA is dissatisfying to the patient and frustrating to the surgeon. In addition, it significantly increases the cost to the healthcare system.
Some authors suggested that revision TKA should be performed during a relatively early period (within 2–5 years after primary surgery) to have a long-term survival and better results in 60%–80% of all revisions.567) However, revision surgery after TKA is always an unfortunate event. Furthermore, it can be even detrimental if the proper time for revision surgery is missed. Therefore, it is important to make a timely and accurate decision on revision surgery through diagnosis of chronically persistent pain after TKA. In addition, it is advised to ensure psychological stability and offer additional nonsurgical treatment for patients who do not require further surgical treatment.
The cause of aseptic persistent pain after TKA should be identified not only for appropriate diagnosis and treatment of the pain but also for improvement of the outcomes of TKA in the future. Evaluation of painful TKA includes variable assessments including clinical examination, serological investigation, radiological evaluation, and microbiological analysis to identify the underlying etiology. 78910) Causes that can result in intractable pain after TKA is generally classified into two categories: septic and aseptic. Of these, pain caused by infection is relatively obvious and not difficult to diagnose, whereas aseptic pain after TKA is not clear in many cases. The purpose of the present study is to investigate the causes of aseptic persistent pain after TKA according to the intra-articular and extraarticular origins and describe the progression of pain of each origin.
Clinical and radiological evaluations were approved by the Hospital Ethics Committee and Institutional Review Board of our institution (IRB No. CNUH-2014-299). A total of 2,590 knees in 2,434 patients with a mean age of 69 years (range, 49 to 91 years) underwent primary TKA in our hospital between January 2004 and December 2012. Of those, 56 knees in 50 patients were lost to the 6-month follow-up. Therefore, 2,534 knees in 2,384 patients were reviewed at postoperative 6 months. A total of 1,015 knees in 964 patients had persistent pain even at 6 months after primary TKA. At postoperative one-year follow-up, the 1,015 knees were reviewed. Of the 1,015 knees, 88 knees (8.7%) were excluded due to infection (32 knees) and periprosthetic fracture (56 knees) following TKA and 805 knees (79.3%) were classified as having unusual prolonged postoperative pain that was relieved within twelve postoperative months. Ultimately, the remaining 122 knees (12.0%) were classified as having aseptic persistent pain with a mean visual analogue scale (VAS) score of 6.1 that was not resolved within 1 postoperative year (Fig. 1).
During the follow-up period, all patients underwent a pain assessment protocol involving history taking, physical examination, analysis of inflammatory markers such as white blood cell (WBC) count, C-reactive protein (CRP) level, and erythrocyte sedimentation rate (ESR), and radiological evaluation. Joint aspiration was performed when the risk of infection was considered high.
All previous medical history including anesthetic and surgical reports, laboratory or aspiration results such as culture and cell counts, and previous antibiotic treatments were reviewed. Furthermore, socio-economic situation, psychological and physical status, patient's expectations, and legal disputes of patients were investigated.
On the physical examination, swelling, active, and passive range of motion, walking with or without supports, tests for any other mechanical symptoms including locking, patellar tracking, and instability were checked. Considering radiating knee pain is related to the hip and spine, examinations on the hip and spine were also performed. Complex regional pain syndrome (CRPS) was evaluated according to the International Association for the Study of Pain (IASP) criteria.11)
Radiological evaluation included weight-bearing anteroposterior and lateral knee radiographs, patellar Merchant view, teleorentgenogram, and computed tomography (CT) scan of the knee. Weight-bearing anteroposterior and lateral knee radiographs and patellar Merchant view were used to assess fixation, position, and size of the component, osteolysis, and maltracking of the patella. Teleorentgenogram was used to assess disease of hip and varus or valgus malalignment. Inclusion criteria for this study included all visible radiographic aseptic loosening osteolytic defects measuring > 30 mm2 in size on at least one radiographic projection (anteroposterior, lateral, or oblique radiograph) and progressively widening interfaces greater than 2 mm in width suggesting loosening without infection (Fig. 2). Polyethylene wear was evaluated by measuring the shortest distance from the femoral condyle to a transverse line through the middle of the superior surface of the baseplate on the anteroposterior and lateral views to obtain an estimate of the insert thickness (Fig. 3).12) After calculating the shortest femorotibial distance, wear and creep deformity of the polyethylene was defined with an accuracy of 0.1 mm or better.13) We defined a stiff knee as one having a flexion contracture of ≥ 15° and/or < 75° of flexion.14)
CT scan was used to assess rotation of the femoral and tibial components and signs of loosening. If an infection was suspected, an aspiration and culture of the knee joint fluid were performed. Further investigations and procedures such as magnetic resonance imaging (MRI) of the spine or hip were carried out if the source of pain was suspected to be from other than the knee.
According to a normality test, intergroup comparisons of age and body mass index (BMI) were made using the Mann-Whitney U-test. Correlations among gender, rheumatoid arthritis, cruciate-retaining implant, and additional procedures were analyzed using the chi-square test. Statistical analysis was done using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) and all analyses were independently reviewed by a statistician.
The 122 painful aseptic TKA knees were largely divided into two groups according to the cause except for infection and periprosthetic fracture: intra-articular group (83 knees, 68.0%) and extra-articular group (39 knees, 32.0%). The mean age at the time of primary surgery was 69.5 years (range, 53 to 85 years) in the intra-articular group and 69.6 years (range, 57 to 91 years) in the extra-articular group. There were 51 males (36 in the intra-articular group and 15 in the extra-articular group) and 71 females (47 in the intra-articular group and 24 in the extra-articular group). There was no statistically significant intergroup difference in age, gender ratio, BMI, cause of primary surgery, implant type, and additional procedure (p > 0.05) (Table 1).
In the intra-articular group, the main reasons for pain were as follows: aseptic loosening (n = 40, 48.2%), polyethylene wear (n = 16, 19.3%), instability (n = 10, 12.0%), recurrent hemarthrosis (n = 5, 6.0%), stiffness (n = 5, 6.0%), patellar maltracking (n = 4, 4.8%), and tendon ruptures (n = 3, 3.6%; 1 quadriceps tendon rupture and 2 patellar tendon ruptures) (Table 2).
Of the 40 patients with painful knees caused by aseptic loosening, 16 were relieved from persistent pain after revision surgery performed within 5 years and 24 patients underwent revision surgery after 5 years. Of the latter 24 patients, 2 complained of knee pain at the time of the last follow-up. In all 16 patients with polyethylene wear-related pain, diagnosis was made within a mean of 6.4 postoperative years and revision surgery was performed; however, 2 patients were not relieved from pain. Ten patients were diagnosed with unstable TKA and were subsequently revised (6 patients within 5 years and 4 patients after 5 years). All these patients did not complain of pain after revision surgery. In a majority of other knees where the causes of pain were recurrent hemarthrosis, patellar maltracking, tendon rupture, and stiffness, revision surgery was performed within 5 years. However, the condition became poor after 5 years in one of the patients with a ruptured tendon who showed only mild symptoms and active extension and walking ability at the time of onset. Pain was not resolved in 1 patient with stiffness.
The pain in the extra-articular group (39 knees) could be due to hip or spine (Table 3). Thus, these patients were referred to other departments in our institute for evaluation of the hip, spine, or vascular problems. Ten knees (25.6%) had nerve entrapment in the spine, all of which were treated with conservative methods such as medication only, selective nerve root block, or epidural block. Pain in 8 of the 10 knees was resolved within 2 years with those treatment methods. Of the 39 knees in the extra-knee group, 6 (15.4%) were found to have hip osteoarthritis (n = 5) or femoral head avascular necrosis (n = 1). Only one of them was treated with total hip arthroplasty. The rest of them were treated with conservative methods such as medication and hip joint injection. Of the six knees, pain was relieved in 2 (33.3%) including the patient with total hip arthroplasty. For the remaining 23 knees (59.0%), the reason for persistent knee pain still remains elusive. Seventeen (73.9%) out of the 23 knees had pain relief without any specific treatment other than the use of nonsteroidal anti-inflammatory drug for 2 years. The remaining 6 knees (15.4%) where the cause was not identified even after 2 years were reviewed at postoperative 4.2 ± 1.4 years. Overall, of the 39 knees in the extra-articular group, 27 (69.2%) did not experience significant pain after 2 years of follow-up.
TKA can provide a better quality of life by improving the range of motion and eliminating knee pain for patients who have chronic knee osteoarthritis. Therefore, postoperative pain is a major cause of dissatisfaction among patients after TKA. Studies have demonstrated that poor management of acute pain after TKA is strongly associated with development of chronic pain, emphasizing the importance of appropriate control of acute pain after TKA.1516) Early diagnosis is very important for the treatment of intractable pain following TKA. A reoperation conducted without identification of a specific reason carries a high risk of failure.1718) Therefore, this study was aimed at improving early diagnosis and facilitating appropriate treatment based on the identification of the underlying causes of pain after TKA.
Some reports suggested that evaluating the character of pain thorough medical history or physical examination would be helpful in determining the cause of pain after TKA.791019) Hofmann et al.7) described several typical patterns of painful TKA and provided evidence for reasons of pain. Similarly, Dennis9) classified such reasons according to the onset of pain. They suggested that component loosening or failure, ligamentous instability, or hematogenousbased infection would be the primary source of pain. For pain developing in months or years after TKA, prosthetic malalignment or nonarticular causes should be the first consideration.
In this study, aseptic loosening, polyethylene wear, instability, recurrent hemarthrosis, patellar maltracking, extensor tendon rupture, and stiffness were categorized as intra-articular reasons of pain after TKA. Spine problems and hip diseases were categorized as extra-articular reasons. Al-Hadithy et al.20) reported that pain after TKA had an unknown origin in most cases, and spine problems and hip osteoarthritis were the second most common causes of pain after TKA. In the present study, a considerable number of cases of aseptic painful TKA had an extra-articular origin, which could be managed with thorough preoperative evaluation on the nature of the pain and appropriate procedures such as epidural block in the perioperative period.
There are numerous intra-articular causes of persistent pain after TKA. Sharkey et al.6) suggested that polyethylene wear was the most common cause of early and late failures, and infection was most responsible (25.4%) for early failures. In another research, aseptic loosening (23.1%) was the most common cause of revision, whereas infection was the second common cause.21) In this study, aseptic loosening, polyethylene wear, instability, and spine problems were all responsible for a high percentage of pain after TKA. We also demonstrated numerous intraarticular causes of painful TKA such as aseptic loosening, polyethylene wear, and instability. Meticulous surgical procedures and efforts to create optimal alignment and uniform tension throughout the range of motion are required to decrease the incidence of pain after TKA resulting from intra-articular causes.
Despite the rigorous clinical and radiological evaluation, 23 knees (18.9%) were classified as having unknown causes in our study. Similarly, Dalury et al.21) reported that pain after operation occurred in one in 8 patients despite the absence of clinical or radiological abnormalities. Therefore, a multidisciplinary approach involving a physiotherapist and a pain management team would be helpful in overall management of pain even if the exact etiology of painful TKA is unidentified.19)
This study was performed to evaluate the causes of persisting pain after TKA and reviewed over 2,500 patients. However, there are some limitations of the present study. First, our study was not standardized in terms of surgical method including the variable prosthesis and additional procedures such as lateral release and patellar resurfacing. Thus, studies using a standardized implant and procedure are required. Second, we did not evaluate the radiological outcomes such as the postoperative mechanical axis and prosthesis position although it is known that postoperative radiological malalignment is related to postoperative persistent pain. Lastly, we did not investigate correlations between pain after TKA and psychological problems, although many authors have reported that psychological distress had great effect on pain after knee or hip arthroplasty.222324)
In conclusion, surgeons should carefully evaluate the preoperative nature of pain to decrease pain of extra-articular origin after TKA. Furthermore, meticulous surgical procedures and optimal alignment should be performed to reduce pain resulting from extra-articular causes such as implant wear, instability, and patellar maltracking.
Figures and Tables
Fig. 1
Flowchart of patients with painful aseptic knee after total knee arthroplasty (TKA). PE: polyethylene, OA: osteoarthritis, AVN: avascular necrosis.

Fig. 2
Postoperative 5-year anteroposterior X-ray (A) and lateral X-ray (B) showing subsidence of the femoral component with osteolysis greater than 2 mm in width around the prosthesis in a 66-year-old female. Anteroposterior X-ray (C) and lateral X-ray (D) taken after revision total knee arthroplasty.

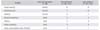
Fig. 3
Postoperative 2-year anteroposterior X-ray (A) and lateral X-ray (B) showing a decrease in the femorotibial distance defined as the shortest perpendicular distance from the femoral condyle to the tibial baseplate. Intraoperative photographs of the thin worn polyethylene inserts (C) and the thick revised polyethylene inserts (D).
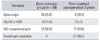
Table 1
Demographic Data of Painful Aseptic Total Knee Arthroplasty*

Table 2
Cause of Pain in the Intra-articular Group
ACKNOWLEDGEMENTS
This study was supported by a grant from Chonnam National University Bitgoeul Hospital Research Institute of Clinical Medicine (No. BCRI14001-51).
References
1. Bae DK, Yoon KH, Kim HS, Song SJ, Yi JW, Kim YC. The results of revision total knee arthroplasty. J Korean Orthop Assoc. 2003; 38(7):689–694.

2. Cameron HU, Hunter GA, Welsh RP, Bailey WH. Revision of total knee replacement. Can J Surg. 1981; 24(4):418–420.
3. Bonnin MP, Basiglini L, Archbold HA. What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc. 2011; 19(9):1411–1417.

4. Lingard EA, Riddle DL. Impact of psychological distress on pain and function following knee arthroplasty. J Bone Joint Surg Am. 2007; 89(6):1161–1169.

5. Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001; (392):315–318.

6. Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper: why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002; (404):7–13.
7. Hofmann S, Seitlinger G, Djahani O, Pietsch M. The painful knee after TKA: a diagnostic algorithm for failure analysis. Knee Surg Sports Traumatol Arthrosc. 2011; 19(9):1442–1452.

8. Dennis DA. A stepwise approach to revision total knee arthroplasty. J Arthroplasty. 2007; 22:4 Suppl 1. 32–38.

9. Dennis DA. Evaluation of painful total knee arthroplasty. J Arthroplasty. 2004; 19:4 Suppl 1. 35–40.

10. Bader R, Mittelmeier W, Steinhauser E. Failure analysis of total knee replacement: basics and methodological aspects of the damage analysis. Orthopade. 2006; 35(9):896–903.
11. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome underdiagnosed. J Fam Pract. 2005; 54(6):524–532.
12. Fehring TK, Murphy JA, Hayes TD, Roberts DW, Pomeroy DL, Griffin WL. Factors influencing wear and osteolysis in press-fit condylar modular total knee replacements. Clin Orthop Relat Res. 2004; (428):40–50.
13. Hoshino A, Fukuoka Y, Ishida A. Accurate in vivo measurement of polyethylene wear in total knee arthroplasty. J Arthroplasty. 2002; 17(4):490–496.

14. Kim J, Nelson CL, Lotke PA. Stiffness after total knee arthroplasty: prevalence of the complication and outcomes of revision. J Bone Joint Surg Am. 2004; 86(7):1479–1484.
15. Puolakka PA, Rorarius MG, Roviola M, Puolakka TJ, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol. 2010; 27(5):455–460.

16. Perkins FM, Kehlet H. Chronic pain as an outcome of surgery: a review of predictive factors. Anesthesiology. 2000; 93(4):1123–1133.
17. Cho WS, Ahn HS, Kim MY, Seol ES, Lee SW, Choi JW. Pain after total knee arthroplasty. J Korean Orthop Assoc. 2006; 41(1):129–133.

18. Mont MA, Serna FK, Krackow KA, Hungerford DS. Exploration of radiographically normal total knee replacements for unexplained pain. Clin Orthop Relat Res. 1996; (331):216–220.

19. Mandalia V, Eyres K, Schranz P, Toms AD. Evaluation of patients with a painful total knee replacement. J Bone Joint Surg Br. 2008; 90(3):265–271.

20. Al-Hadithy N, Rozati H, Sewell MD, Dodds AL, Brooks P, Chatoo M. Causes of a painful total knee arthroplasty: are patients still receiving total knee arthroplasty for extrinsic pathologies? Int Orthop. 2012; 36(6):1185–1189.

21. Dalury DF, Pomeroy DL, Gorab RS, Adams MJ. Why are total knee arthroplasties being revised? J Arthroplasty. 2013; 28:8 Suppl. 120–121.

22. Merle C, Brendle S, Wang H, Streit MR, Gotterbarm T, Schiltenwolf M. Multidisciplinary treatment in patients with persistent pain following total hip and knee arthroplasty. J Arthroplasty. 2014; 29(1):28–32.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download