Abstract
Background
The purpose of this study was to determine the shape of the distal femur of Korean women compared with the prostheses currently available in Korea.
Methods
Morphometric data (5 parameters) were measured in 356 resected femurs of Korean women undergoing primary total knee arthroplasty (TKA) utilizing the LCS knee implant (DePuy). The data were then compared with 5 additional contemporary TKA implant systems.
Results
Implant designs based on Caucasian population data do not ideally match the distal femoral morphology of Korean women. Overhang at the anterior mediolateral width was observed in 84.8% for the LCS while a gender-specific implant resulted in undercoverage of the bone in 86%. Posterior overhang was observed in up to 51.2%. Most implant designs have a narrower intercondylar notch than the morphologic data of Korean women.
Conclusions
Since there is some difference between the shape of distal femur of Korean women and that of the implants, surgeons should have this in mind when selecting an implant for a patient. These data may also be used as a guideline for future prosthetic design options for Korean women population.
Total knee arthroplasty (TKA) has proven to be a highly successful operation for both pain relief and functional improvement. However, several studies have shown that up to one-third of patients were dissatisfied with their outcome even though they were thought to have had successful results by their surgeons.12) With the increasing availability of knee arthroplasty in Asian populations, functional demands for high flexion activities, such as kneeling and cross-legged sitting, have also increased, which resulted in modification of surgical techniques and implant design.
Traditionally, implant companies have used anthropometric data to create implant sizes that fit the average patients within a predetermined range.3) These data came from a variety of sources, measuring the anteroposterior (AP) and mediolateral (ML) dimensions of knees.456) However, most of these data came from Caucasian populations, and consequently prostheses may not be suitable for Asian populations for various reasons including overhang of the femoral component.7891011) Moreover, there is little information describing knee morphology of the Asian population which is necessary to assist in designing appropriate size-matched TKA components. Although there are several studies that have sought to address this issue, they have limitations. The number of patients reported was small and measurements were limited to AP and ML dimensions, while the dimensions were measured from imaging inclusive of computed tomography (CT) and magnetic resonance imaging (MRI).78101213) Direct measurements of the prepared bone surfaces will provide more accurate data.6914)
The purpose of this study was to analyze the anatomic data collected from a large group of Korean women patients undergoing primary TKA and compare these measurements with the dimensions of contemporary femoral component prostheses. These data will provide an insight into implant sizing for a Korean population.
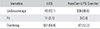
Morphologic data from the distal femoral surfaces for 356 knees in 236 women who underwent primary TKA were collected between November 2007 and August 2008 and were analyzed retrospectively. The study was approved by the Institutional Review Board and a consent form was signed by each patient. Demographic information of these patients is shown in Table 1. The mean age of the patients at the time of the index procedure was 69 ± 7.2 years (range, 51 to 84 years). The mean body weight was 60.1 ± 8.5 kg (range, 37 to 81 kg), the mean body height was 152.5 ± 5.9 cm (range, 138 to 167 cm), and the mean body mass index was 25.8 ± 3.2 kg/m2 (range, 17.6 to 38.3 kg/m2). All patients were Korean women with a diagnosis of osteoarthritis or rheumatoid arthritis. As the dimension of cutting surface would be influenced by the amount of distal femoral cutting, to minimize the bias, patients with severe varus or valgus deformity and flexion contracture of more than 30° were excluded.
The LCS Mobile Bearing Total Knee System (DePuy, Warsaw, IN, USA) was employed in this patient population with bone cuts following standard accepted surgical procedures.15) All medial, lateral, and posterior osteophytes were removed before measurements. To achieve consistent flexion gaps, the implant size was chosen based on the AP dimension rather than the ML dimension. As patients who have severe varus or valgus deformity and flexion contracture were excluded, additional cutting of the distal femur was not needed and a constant insert with a thickness of 12.5 mm was used in all patients. After appropriate component size selection and all bone cutting, each dimension was measured in millimeters with the use of a sterilized caliper and a depth gauge according to a standardized protocol. The measurements included: (1) anterior ML (AML) as the ML width on the anterior cut surface of the distal femur; (2) posterior ML (PML) as the ML width on the posterior cut surface of the distal femur; (3) medial posterior condyle (MPC); and (4) lateral posterior condyle (LPC) as the medial and lateral lengths of the posterior condyle, respectively; as well as (5) intercondylar (IC) notch as the width of the posterior aspect of the IC (Fig. 1). All measurements were performed by one surgeon to eliminate interobserver bias.
These data were compared with the following 6 implant designs: LCS (DePuy), PFC Sigma (DePuy Synthes, Warsaw, IN, USA), NexGen LPS (Zimmer, Warsaw, IN, USA), NexGen LPS Gender (Zimmer), Triathlon (Stryker, Mahwah, NJ, USA), and ACS Hyperflex (Implantcast, Buxtehude, Germany). As the AP size was determined as part of the procedure, attempts were made to compare the dimensions from each implant with similar AP dimensions.6) For data analysis, best fit lines were calculated with use of least-squares regression.
Measured data of all patients for each AP size pertaining to the LCS system (DePuy) is shown in Table 2. Each dimension, AML, PML, IC, MPC, and LPC, was then compared with those of 5 further contemporary knee implant designs available in Korea.
Graphs showing the resected femoral AML and PML data plotted against each LCS AP size along with the available AP sizes of the other 5 knee implants are shown in Fig. 2, respectively. The LCS design showed the largest AML dimension, resulting in an implant overhang of ≥ 1 mm in 84.8% of this patient population (Fig. 3). In contrast, the NexGen LPS Gender had the smallest AML dimension, potentially resulting in bone undercoverage of ≥ 1 mm in 86% (Table 3). Further, at the PML site, most implant designs had narrower dimensions than the measured data. Exposed bone beyond the edge of the implant of ≥ 1 mm was observed in 90.4% of the LCS patient population.
To compare the overall shape of the resected femur with that of the implants, the AML/PML ratio was calculated as AML width/PML width × 100 (Fig. 4). The majority of the implant designs studied had a higher AML/PML ratio than the measured data. This means that the shape of the distal femur of Korean women is more trapezoidal than the implant designs.
The mean values of the MPC and LPC were 19.4 ± 2.3 mm (range, 14 to 26 mm) and 18.9 ± 2.3 mm (range, 12 to 26 mm), respectively. A graph showing the LPC plotted against each LCS AP size along with the available AP sizes of the other 5 knee implants is presented in Fig. 5A. Values of the MPC displayed a similar pattern (Fig. 5B). As each implant design has a different inner surface design for the chamfer, direct comparison of the measured posterior condylar length of the other implant designs studied was possible only with LCS. Overhang of ≥ 1 mm was observed on the MPC and LCP in 37.3% and 51.2%, respectively, of the LCS patient population (Fig. 6).
The mean value of the IC was 19.6 ± 1.5 mm (range, 16 to 24 mm). Although each implant design has a different patella groove depth and angle, comparison of the measured width showed that most designs had narrower ICs than the morphologic data obtained from Korean women (Fig. 7).
The results of this study demonstrate that knee implant designs based on Caucasian population data do not ideally match the distal femoral morphology of Korean women.
Previous studies radiographically measured the ML width and AP length to evaluate the morphology of the distal femur.781012131617) While these data provide information on the overall shape of the distal femur, they may not be suitable for femoral implant designs as radiographic dimensions will be different from the actual width and length after bone cutting in surgery. In agreement with previous studies,6811) all measurements of the distal femur were performed after the completion of all bone cuts and are thought to be more accurate and useful in designing implants.
Some previous studies have demonstrated that Asian knees are generally smaller than Caucasian knees,71114) but they only compared the AP and ML ratio of the distal femur and did not describe detailed shape differences required for prosthesis design development. In this study, not only were the AP and ML dimensions of the distal femur measured, but also the AML and PML, posterior condylar length (LPC and MPC), and IC width.
Compared with a previous study by Hitt et al.6) using the same measuring method for a Caucasian population, the AP/ML ratio of the distal femur was similar between Caucasian and Korean women. However, when detailed measurements including AML, PML, LPC, MPC, and IC were compared with those of several prostheses, size differences were observed.
The majority of implants studied had higher AML/PML ratios than the measured data in Korean women. This implies that the shape of the distal femur of Korean women is more trapezoidal than the implants measured and explains why overhang is commonly observed at the AML site of the distal femur. Guy et al.18) also reported that 58% of females had an overhang of greater than 2 mm when they had been given a standard femoral component. Although it is not known whether this overhang influences clinical outcomes, overhanging of femoral components in the ML dimension could potentially lead to altered soft tissue tension and patellofemoral stresses.36) Mahoney and Kinsey,19) in a clinical study, concluded that greater than 3 mm femoral component overhang approximately doubles the occurrence of knee pain at 2 years after TKA.
Conversely, one gender-specific design (NexGen LPS Gender) had a lower AML/PML ratio than the measured data from Korean women. Therefore, undercoverage of the bone at the anterior femur could be expected in 86% of the LCS patient population. This finding is consistent with previous reports by Kim et al.2021) where distal femoral undercoverage was observed in 89.1% of the patients with a NexGen Gender CR-Flex knee and in 84% with a NexGen Gender LPS-Flex knee. They postulated that more exposed cancellous bone may lead to higher blood loss postoperatively and result in increased osteolysis from wear debris in the long term.
During surgery, appropriately sized femoral components can be determined by the AP dimension of the distal femur.1522) If an appropriately sized femoral component then overhangs in the ML dimension, the surgeon may have three options. First, the surgeon can accept overhang of the implant. Although there is a paucity of literature as to the degree that affects clinical results, overhang has a potential to impact soft tissue irritation, soft tissue balance, motion, patellofemoral stresses, and pain.6919) Second, downsizing of the implant can be adopted; however, this may cause notching of the anterior cortex with a posterior reference system or widening of the flexion gap with an anterior reference system.1822) Third, an implant with a narrow ML dimension such as a gender-specific design can be chosen for better fit; however, as the current study shows, gender-specific designs can cause overly exposed cancellous bone. Therefore, it is important for the surgeon to have a selection of implant sizes that will match their patient population most accurately.
When the measured LPC and MPC were compared with those of the LCS prosthesis, the reported range within the same AP size indicates that optimal fit is unlikely. Bellemans et al.,23) demonstrating large variable dimensions of the femur for any given AP size, concluded that the shape of the knee is determined both by gender and morphotype of the patient. Our study also confirms this variability of distal femoral dimensions for a given AP size. Although we could compare the measured posterior condylar length only with 1 implant (LCS), the potential for overhang of the posterior condyle can happen with any implant design. This may cause overstuffing, which can limit postoperative range of motion. Harwin et al.,24) observed higher flexion with implants utilizing a shorter posterior condylar design and surmised that this finding was due to less tension on the posterior capsule. However, a longer-term follow-up is needed to prove this finding. Overhang of the posterior condyle also may have negative effects on the longevity of the implant. Choi et al.,25) in a clinical report analyzing the patterns and causative factors of early aseptic loosening after TKA, documented that protrusion of the femoral component over the posterior condyle was more prominent in the loosened group than in the control group. Other researchers2627) have pointed out that inadequate support of the posterior femoral condyle may cause the femoral component to migrate during deep knee flexion and contribute to femoral loosening. Again, more reliable research is needed to prove whether the posterior implant overhang has biomechanical effects that promote loosening of the femoral component. An overhanging metallic edge may also cause capsular or popliteal impingement.28)
Our data also showed that Korean women have wider ICs than the implant designs studied. Ryu et al.,29) in a clinical report comparing favorable post-TKA flexion group (≥ 120°) with poor post-TKA flexion group (≤ 90°), reported that the patellar thickness increased in the poor flexion group. Mihalko et al.,30) in their cadaveric study, reported that 2 mm and 4 mm build-up in the trochlear groove and patella resulted in a flexion loss of 1.8° and 4.4°, respectively. Similarly, the narrower IC of a prosthesis may have a negative effect on the postoperative range of motion, as it increases the trochlear groove height in the anterior compartment.
To our knowledge, this study is the first that has comprehensively evaluated diverse dimensions of the distal femur after bone preparation including the AML, PML, posterior condyle, and IC. Our results showed several size differences between the measured data and the dimension of implants and also demonstrated how often component overhang or undercoverage can happen. However, there are some limitations of the present study. First, it is difficult to rule out the possibility of some bias in data collection because it is entirely dependent on the surgeon's judgement to determine the best femoral component size that fits the AP dimension of each patient and the degree of femoral external rotation that is applied to each patient. Second, as each implant has different inner surface designs with regard to the chamfer angle and implant thickness, it may not be accurate to directly compare the measurements of the cutting surface of one implant system with those of other implants.
Since we found some differences between the shape of the distal femur of Korean women and that of the implants, we suggest that the surgeon should have this in mind when selecting an implant for a given patient. Our data also may be used as a guideline for future prosthetic design options for Korean women population.
In conclusion, the distal femoral shape of Korean women was different in a substantially large primary TKA patient population from that of currently available TKA implants designed based on the anthropometric data of Caucasian populations. Although clinical evidence concerning the effects of overhang or undercoverage of the femoral component is not sufficient, surgeons should consider these differences when selecting an implant design and determining the best-fit size. Our data also may be used as a guideline for future prosthetic design options for Korean women population.
Figures and Tables
Fig. 1
Visualization of the definition of each measured dimension after distal femoral bone cut. (A) The anterior mediolateral (AML), posterior mediolateral (PML), and intercondylar notch (IC) were measured with a caliper. (B) Medial posterior condyle (MPC) and lateral posterior condyle (LPC) length dimensions were obtained using a depth gauge.

Fig. 2
Measured anterior mediolateral (AML, A) and posterior mediolateral (PML, B) data plotted against the LCS (DePuy) anteroposterior (AP) size along with the available AP sizes of the other 5 knee implants studied including PFC Sigma (DePuy Synthes), NexGen LPS (Zimmer), NexGen LPS Gender (Zimmer), Triathlon (Stryker), and ACS Hyperflex (Implantcast).

Fig. 3
Intraoperative picture showing the overhang of an LCS (DePuy) implant beyond the resected surface of the distal femur at the anterior mediolateral site.

Fig. 4
The anterior mediolateral (AML) / posterior mediolateral (PML) ratio (AML width / PML width × 100) was calculated and plotted against the anteroposterior (AP) size of all implants including LCS (DePuy), PFC Sigma (DePuy Synthes), NexGen LPS (Zimmer), NexGen LPS Gender (Zimmer), Triathlon (Stryker), and ACS Hyperflex (Implantcast).

Fig. 5
Measured lateral posterior condyle (A) and medial posterior condyle (B) data plotted against the LCS (DePuy) anteroposterior (AP) size along with the available AP sizes of the other 5 knee implants studied including PFC Sigma (DePuy Synthes), NexGen LPS (Zimmer), NexGen LPS Gender (Zimmer), Triathlon (Stryker), and ACS Hyperflex (Implantcast).

Fig. 6
Postoperative radiograph (A) and line drawing (B) showing posterior condylar overhang of the LCS prosthesis (DePuy).

Fig. 7
Measured intercondylar data plotted against the LCS (DePuy) anteroposterior (AP) size along with the available AP sizes of the other 5 knee implants studied including PFC Sigma (DePuy Synthes), NexGen LPS (Zimmer), NexGen LPS Gender (Zimmer), Triathlon (Stryker), and ACS Hyperflex (Implantcast).

Table 1
Summary of Patient Demographics

| Parameter | Value |
|---|---|
| No. of knees | 356 |
| Age (yr) | 69 ± 7.2 (51–84) |
| Weight (kg) | 60.1 ± 8.5 (37–81) |
| Height (cm) | 152.5 ± 5.9 (138–167) |
| Body mass index (kg/m2) | 25.8 ± 3.2 (17.6–38.3) |
Table 2
Summary of Morphometric Data (n = 356) after All Distal Femoral Bone Cuts

ACKNOWLEDGEMENTS
The authors would like to thank A. Seth Greenwald and Christine S. Heim (Orthopaedic Research Laboratories, Cleveland, OH, USA) for their valuable contributions and assistance to this research.
References
1. Dickstein R, Heffes Y, Shabtai EI, Markowitz E. Total knee arthroplasty in the elderly: patients' self-appraisal 6 and 12 months postoperatively. Gerontology. 1998; 44(4):204–210.

2. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006; 452:35–43.

3. Barrett WP. The need for gender-specific prostheses in TKA: does size make a difference? Orthopedics. 2006; 29:9 Suppl. S53–S55.
4. Rostlund T, Carlsson L, Albrektsson B, Albrektsson T. Morphometrical studies of human femoral condyles. J Biomed Eng. 1989; 11(6):442–448.

5. Chin KR, Dalury DF, Zurakowski D, Scott RD. Intraoperative measurements of male and female distal femurs during primary total knee arthroplasty. J Knee Surg. 2002; 15(4):213–217.
6. Hitt K, Shurman JR 2nd, Greene K, et al. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003; 85:Suppl 4. 115–122.
7. Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty. 2000; 15(1):79–85.
8. Urabe K, Miura H, Kuwano T, et al. Comparison between the shape of resected femoral sections and femoral prostheses used in total knee arthroplasty in Japanese patients: simulation using three-dimensional computed tomography. J Knee Surg. 2003; 16(1):27–33.
9. Ho WP, Cheng CK, Liau JJ. Morphometrical measurements of resected surface of femurs in Chinese knees: correlation to the sizing of current femoral implants. Knee. 2006; 13(1):12–14.
10. Cheng FB, Ji XF, Lai Y, et al. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee. 2009; 16(5):341–347.
11. Chaichankul C, Tanavalee A, Itiravivong P. Anthropometric measurements of knee joints in Thai population: correlation to the sizing of current knee prostheses. Knee. 2011; 18(1):5–10.

12. Cheng FB, Ji XF, Zheng WX, et al. Use of anthropometric data from the medial tibial and femoral condyles to design unicondylar knee prostheses in the Chinese population. Knee Surg Sports Traumatol Arthrosc. 2010; 18(3):352–358.

13. Lim HC, Bae JH, Yoon JY, Kim SJ, Kim JG, Lee JM. Gender differences of the morphology of the distal femur and proximal tibia in a Korean population. Knee. 2013; 20(1):26–30.

14. Chin PL, Tey TT, Ibrahim MY, Chia SL, Yeo SJ, Lo NN. Intraoperative morphometric study of gender differences in Asian femurs. J Arthroplasty. 2011; 26(7):984–988.

15. Dorr LD, Boiardo RA. Technical considerations in total knee arthroplasty. Clin Orthop Relat Res. 1986; (205):5–11.

16. Matsuda S, Matsuda H, Miyagi T, Sasaki K, Iwamoto Y, Miura H. Femoral condyle geometry in the normal and varus knee. Clin Orthop Relat Res. 1998; (349):183–188.

17. Matsuda S, Miura H, Nagamine R, et al. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res. 2004; 22(1):104–109.

18. Guy SP, Farndon MA, Sidhom S, Al-Lami M, Bennett C, London NJ. Gender differences in distal femoral morphology and the role of gender specific implants in total knee replacement: a prospective clinical study. Knee. 2012; 19(1):28–31.

19. Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010; 92(5):1115–1121.

20. Kim YH, Choi Y, Kim JS. Comparison of a standard and a gender-specific posterior cruciate-substituting high-flexion knee prosthesis: a prospective, randomized, short-term outcome study. J Bone Joint Surg Am. 2010; 92(10):1911–1920.

21. Kim YH, Choi Y, Kim JS. Comparison of standard and gender-specific posterior-cruciate-retaining high-flexion total knee replacements: a prospective, randomised study. J Bone Joint Surg Br. 2010; 92(5):639–645.
22. Greene KA. Gender-specific design in total knee arthroplasty. J Arthroplasty. 2007; 22:7 Suppl 3. 27–31.

23. Bellemans J, Carpentier K, Vandenneucker H, Vanlauwe J, Victor J. The John Insall Award: both morphotype and gender influence the shape of the knee in patients undergoing TKA. Clin Orthop Relat Res. 2010; 468(1):29–36.

24. Harwin SF, Greene KA, Hitt K. Early experience with a new total knee implant: maximizing range of motion and function with gender-specific sizing. Surg Technol Int. 2007; 16:199–205.
25. Choi YJ, Kang JH, Lee KW, Joo YS, Park JS, Choo HH. Early aseptic loosening after total knee replacement using legacy posterior stabilized-flex prosthesis. J Korean Orthop Assoc. 2012; 47(1):35–40.

26. King TV, Scott RD. Femoral component loosening in total knee arthroplasty. Clin Orthop Relat Res. 1985; (194):285–290.

27. Zelle J, Janssen D, Van Eijden J, De Waal Malefijt M, Verdonschot N. Does high-flexion total knee arthroplasty promote early loosening of the femoral component? J Orthop Res. 2011; 29(7):976–983.

28. Barnes CL, Scott RD. Popliteus tendon dysfunction following total knee arthroplasty. J Arthroplasty. 1995; 10(4):543–545.

29. Ryu J, Saito S, Yamamoto K, Sano S. Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis. 1993; 53(3):35–40.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download