Abstract
Background
Percutaneous lateral hemiepiphysiodesis of the lower extremity is a simple and excellent method to correct the angular and length problems cosmetically. However, the efficacy of percutaneous lateral hemiepiphysiodesis is not well established in the literature. The purpose of this study was to evaluate the efficacy of percutaneous lateral hemiepiphysiodesis for angular corrections in adolescent idiopathic genu varum patients with proximal tibia vara and identify the factors affecting the amount of deformity correction of the lower limb in the coronal plane.
Methods
We retrospectively reviewed 20 patients (40 lower limbs) who had percutaneous lateral hemiepiphysiodesis on the proximal lateral tibia between 1997 and 2010. Radiographic evaluations were made using (1) the hip-knee-ankle angle and (2) the length of the tibia. Furthermore, the intercondylar distance was evaluated at the level of the knee joint. Preoperative factors (gender, age, body mass index, intercondylar distance, preoperative hip-knee-ankle angle, remaining growth of tibia, and calculated correctable angle) were analyzed, as well as their correlation with the degree of the actual correction angle.
Results
The amount of coronal deformity of the lower limb was improved from its preoperative state. The median average of hip-knee-ankle angle improved from 8.0° (interquartile range [IQR], 7.0° to 10.0°) preoperatively to 3.0° (IQR, 2.5° to 4.0°) at the final follow-up (p < 0.001). The median percent ratio of the angular correction was 60% (IQR, 50% to 71.3%). The correlation coefficients were –0.537, 0.832, 0.791, and 0.685 for the bone age, preoperative hip-knee-ankle angle, the remaining growth of tibia, and calculated correctable angle, respectively.
Conclusions
Despite the excellent cosmetic outcome of percutaneous lateral hemiepiphysiodesis on the proximal lateral tibia in adolescent idiopathic genu varum, the effect was limited in most cases. For optimum results, surgery a few months earlier is recommended, rather than at the calculated operation time.
There are multiple surgical options for the correction of coronal deformities of the lower limb. The corrective osteotomy is used for acute correction, while the asymmetrical epiphysiodesis is a method of gradual correction involving temporal and permanent hemiepiphysiodesis. Among the various methods, percutaneous lateral hemiepiphysiodesis (PLH) is an ablation of a selected and limited area of the growth plate. PLH is advantageous because it is less invasive, has a low morbidity, requires only a short hospital stay, produces minimal scarring, and does not require a second operation for hardware removal.1) Scarring is a serious problem that cannot be ignored in adolescents. Studies have reported positive results of percutaneous permanent epiphysiodesis for leg length discrepancy.23) However, there are few reports on the effect of PLH on angular correction. 4) Additionally, the ideal timing for optimal results of correction is still unknown.
Therefore, we investigated the efficacy and clinical outcomes of PLH with respect to angular correction. Correction of coronal plane deformities of the lower limb by PLH on only the proximal tibia and factors associated with the amount of correction of angular deformities of the lower limb were evaluated, and the results were presented.
This retrospective study included 25 patients with idiopathic genu varum (50 lower limbs) who underwent PLH on the proximal lateral tibia for a varus angular deformity from 1997 to 2010. The study was approved by the Institutional Review Board of Samsung Medical Center. The need for informed consent was waived because of the retrospective nature of the study.
The inclusion criteria were patients aged ≤ 16 years who underwent PLH on the proximal lateral tibia for idiopathic genu varum and were followed until skeletal maturity. Skeletal maturation was determined with evidence of epiphyseal plate closure from radiographs.
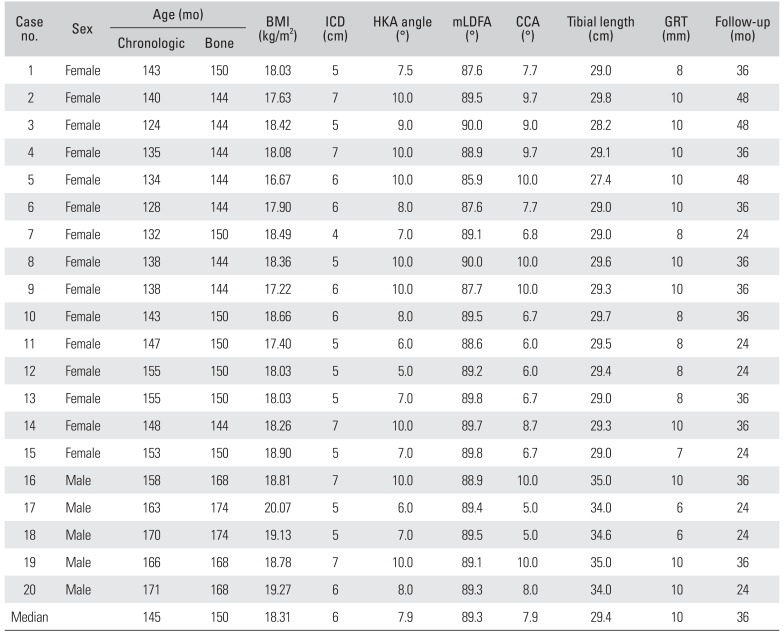
Indications of surgery were (1) varus deviation of a mechanical axis at the knee joint level of more than 5° with a proximally migrated fibular head above the epiphysis of tibia; (2) more than 5 cm of intercondylar distance (ICD) in the knee joint; (3) appropriate remaining growth of tibia on the Anderson and Green graph;5) and (4) normal range of mechanical lateral distal femoral angle (mLDFA; 86° to 89°). Five patients who did not have follow-up data until skeletal maturation were excluded. Demographic data were reviewed (Table 1). The total of 20 patients included 15 girls and 5 boys. The median and interquartile range (IQR) of bone age at the time of surgery was 144 months (IQR, 144 to 150 months) and 168 months (IQR, 168 to 174 months) in girls and boys, respectively. The mean body mass index (BMI) was 18.3 kg/m2 (IQR, 18.0 to 18.8 kg/m2). The median follow-up period was 33.6 months (range, 24 to 48 months).
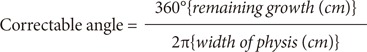
The timing of PLH was determined by using calculated correctable angle. Correctable angle was calculated by the following equation (Fig. 1):1)
The bone age was checked at the preoperative visit. Subsequently, the remaining growth of tibia was calculated from the Anderson and Green graph.5) For example, a girl of 144-month-old (bone age) with 10° of hip-knee-ankle (HKA) angle has a 6 cm of physis width; the remaining growth of tibia was 1 cm by using the Anderson and Green graph. Subsequently, the correctable angle was calculated by the above equation. Finally, the result was 9.5°. We considered that the timing for operation was appropriate if the HKA angle matched the calculated correctable angle by the above equation.
All procedures were performed by a senior surgeon (JSS). The lower extremity was surgically prepared under general anesthesia with a pneumatic tourniquet on the operated limb. Physis area was identified under image intensifier control. A 1-cm surgical incision was made over the lateral physis of the proximal tibia. The proximal one third lateral tibia epiphyseal plate was removed with drills of increasing bit size. The epiphysiodesis was completed by curettage and the remaining cartilaginous material was checked. Concomitant proximal fibular epiphysiodesis was conducted. After thorough irrigation, we removed any bony material from the soft tissues to prevent the formation of heterotopic bone.6) Postoperatively, patients used a cylinder splint for 1 week. Partial weight bearing was permitted after the first week.
Preoperative and postoperative full-length hip-to-ankle radiographs were used to measure the HKA angle. Standing radiographs (from the femoral head to the ankle joint) were obtained using standard protocols. Postoperative radiographs were taken at 6 weeks and every 3 months after surgery, and as required, until skeletal maturation was evident. Preoperative and final follow-up radiographs were analyzed retrospectively. All radiographic evaluations were performed by two independent examiners (YSL, KW).
Radiographic measurements were evaluated by using a picture archiving and communications systems (PACS; General Electric, Chicago, IL, USA) monitor that computed lengths and angles automatically. The following were measured: (1) the degree of pre- and postoperative knee deformity or HKA angle was determined on the standing full-length radiographs as the angle between the mechanical axis of the femur (center of the femoral head to the center of the knee) and the mechanical axis of the tibia (center of the knee to the center of the ankle plafond) 7) and (2) tibial growth was measured by calculating the differences of tibial length between the preoperative and final follow-up periods. Tibial lengths were measured from the lowest point of the intercondylar eminence of the tibia (tibial spine) to the center of the ankle formed by the tibia and the fibula.8)
We reviewed the medical records of all patients. The clinical assessment consisted of intercondylar distance and postoperative complications such as wound problems, nonunion, delayed union, leg length difference and overcorrection. ICD was measured as the gap between the medial femoral condyle in keeping feet together. The other minor and transient complications investigated involved temporal altered sensation and patient discomfort. Furthermore, we investigated secondary deformities in sagittal plane, such as procurvatum or recurvatum despite the attempts to correct the deformity in coronal plane.
We compared the results on degree of the HKA angular correction. The percent ratio of the correction was defined as the ratio of the amount of angular correction to the preoperative angular deformity. The amount of angular correction was determined as the difference between the preoperative and final HKA angles.
Although operation was bilateral in all patients, data were selected from right single limb for analysis to ensure statistical independency. Data were presented as median and IQR for all measured parameters. The Wilcoxon rank sum test was used to determine significant differences in angulation between the preoperative and final HKA angles. The correlation between preoperative factors and the amount of angular correction with Pearson correlation analysis was analyzed. All statistical analyses were carried out using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). A p-value < 0.05 was considered statistically significant.
The amount of coronal deformity of lower limb was significantly improved, as compared to the preoperative values. The coronal deformity of knee joint with HKA angles was assessed. The median values of the HKA angle improved from 8.0° (IQR, 7.0° to 10.0°) preoperatively, to 3.0° (IQR, 2.5° to 4.0°) at the final follow-up (p < 0.001). The median correction angle was 4.9° (IQR, 3.7° to 6.2°). The median value of the percent ratio of the correction of the HKA angle was 60.0% (IQR, 50.0% to 71.4%). There was no case of overcorrection. We obtained one case with 100% of the percent ratio of the correction (complete correction) and one case with 0% of the percent ratio of the correction (failure of correction). The median ICD at final follow-up was 3.0 cm (IQR, 2.0 to 3.3 cm) and the amount of improvement was 3.0 cm (IQR, 2.0 to 4.0 cm).
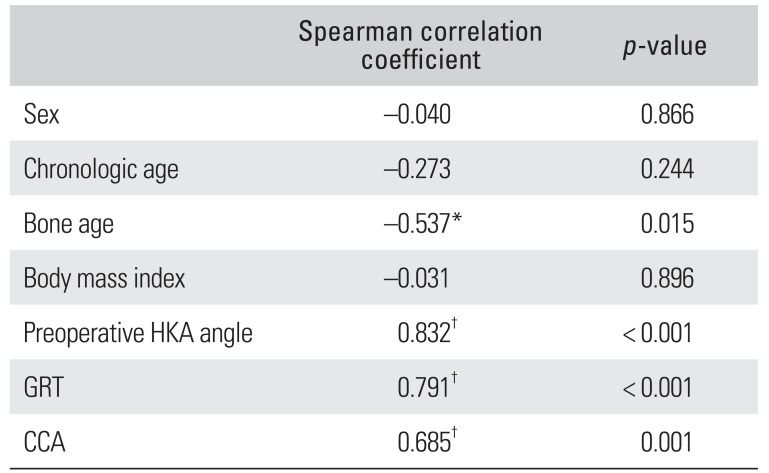
There were significant correlations between the bone age, preoperative HKA angle, growth remaining of tibia or calculated correctable angle and the actual correction angle. The correlation coefficients for the bone age, preoperative HKA angle, growth remaining of tibia, and calculated correctable angle were –0.537, 0.832, 0.791, and 0.685, respectively. However, there were no significant correlations between body mass index or chronological age and actual correction angle (p > 0.05) (Table 2).
A total of 3 postoperative complications occurred in three different patients. We identified one case of temporal knee joint pain and two cases of temporal hypoesthesia. There were no cases of persistent non-union of proximal tibia, wound problems, leg length differences, or other minor or transient complications. Additionally, there was no sagittal secondary deformity, such as procurvatum or recurvatum.
PLH is a reasonable procedure with low morbidity for treating young age patients with coronal angular deformity of the knee. Nevertheless, there is uncertainty regarding the degree of correction due to the individuality of patients. Thus, reports on PLH and the angular correction of knee joint are valuable for patient consultation and management. We accordingly investigated factors that correlated with the actual correction angle in idiopathic genu varum patients.
The most important finding of the present study is that PLH of the proximal tibia can achieve misalignment correction in idiopathic adolescent genu varum. Our results indicated that PLH performed on a proximal tibia had an approximately 60% correction power to the coronal deformity of whole lower limbs. A previous report showed outcomes for PLH of the combination of both distal femur and proximal tibia; however, our results showed that PLH performed only on the proximal tibia provided a reliable correction of angular deformity.49) Since all our patients had normal mLDFA, the normal femoral structure was not manipulated. The mean error of angular correction (actual versus predicted) of the genu varum deformities was 3.2° (range, 0° to 6°). The correction error of our procedure was more than the results of a previous report. Inan et al.9) reported about 1.5° of correction error with combined PLH on the distal femur and proximal tibia in idiopathic genu valgum. PLH on only the proximal tibia has an expectedly weaker correction power than PLH on both the distal femur and proximal tibia.
PLH requires an accurate calculation of the remaining growth in order to determine the exact timing of the procedure.1011) Hemiepiphysiodesis is a challenging procedure and surgeons cannot guarantee definite postoperative corrections. The inaccurate timing of surgery in PLH can lead to a miscorrection of the deformity. However, although we obtained almost the exact timing window for conducting the procedure, numerous factors such as a disease of physis, and various union periods could lead to under- or over-correction of the deformity.41213) Therefore, Khoury et al.14) suggested that close follow-up is a necessity.
We suggest that patients undergo PLH on the proximal tibia at an earlier point than that based on correctable angle. Given our results, that over 80% of the cases showed a corrective outcome greater than 50% relative to the preoperative values, there was still an amount of residual deformity (Fig. 2). After PLH, the bone needs time for union or healing; and this interval could be the potential cause of under-correction. We therefore recommend this procedure a few months earlier than calculated. However, because of the limitation of small sample size, we could not determine at what earlier time point the surgery is required, as compared to the calculated operation timing. Thus, further investigation is required.6)
In this study, we determined the correlation of surgical results with bone age, preoperative HKA angle, calculated expected values of tibial growth, and angle of correction. Our results indicated that the completely corrected case (no. 3) showed the largest tibial growth (Fig. 3) with 10 mm of remaining growth. This was the largest in the cohort. In contrast, case no.11, which showed no correction, had the smallest tibial growth (Fig. 4) with 6 mm of remaining growth of tibia. This was the smallest in the cohort. These results suggested that residual growth potential and bone age are critical to the success of PLH.
Gradual correction of genu varum is possible by temporary hemiepiphysiodesis such as stapling,15) applying transphyseal screws16) or the eight-Plate.11) However, permanent hemiepiphysiodesis was performed because of better outcomes in morbidity, cosmetics, and cost, as compared to temporary hemiepiphysiodesis. As noted above, PLH has low morbidity because it is a less invasive method and requires short hospital stay. It only produces minimal scarring, which can be a serious concern for adolescents. Temporary hemiepiphysiodesis requires a second operation for hardware removal unlike PLH.1) PLH reduces not only the financial burden, but also the anesthetic risk of the patients.
We did not perform PLH in the patients younger than 120 months of bone age, because it is difficult to predict the remaining angular growth or determine of proper time for hemiepiphysiodesis in young patients. Also, since young patients have greater growth potential, permanent hemiepiphysiodesis can result in overcorrection. Thus, in this study, surgery was not performed in patients younger than 120 months of bone age.
This study had several limitations that require consideration. First, it included had a relatively small number of patients and no control group. Second, the study was retrospective. However, to the best of our knowledge, this study was conducted on the largest idiopathic genu varum patient cohort. Additionally, we conducted the operation only for the tibial lesion in patients with normal femoral anatomy. We used skeletal maturation as the end point for our study for follow up in all patients.
In conclusion, PLH on the lateral tibia is a simple, safe and cosmetically excellent procedure for adolescent idiopathic genu varum patients. However, this operation had a limited correction effect in most of the patients. For optimum results, this surgery should be performed a few months earlier than the calculated operation time. After careful growth calculation, surgery should be performed only in patients with sufficient remaining growth.
References
1. Bowen JR, Leahey JL, Zhang ZH, MacEwen GD. Partial epiphysiodesis at the knee to correct angular deformity. Clin Orthop Relat Res. 1985; (198):184–190. PMID: 4028549.

2. Babu LV, Evans O, Sankar A, Davies AG, Jones S, Fernandes JA. Epiphysiodesis for limb length discrepancy: a comparison of two methods. Strategies Trauma Limb Reconstr. 2014; 9(1):1–3. PMID: 24271553.
3. Horn J, Gunderson RB, Wensaas A, Steen H. Percutaneous epiphysiodesis in the proximal tibia by a single-portal approach: evaluation by radiostereometric analysis. J Child Orthop. 2013; 7(4):295–300. PMID: 24432090.

4. Ferrick MR, Birch JG, Albright M. Correction of non-Blount's angular knee deformity by permanent hemiepiphyseodesis. J Pediatr Orthop. 2004; 24(4):397–402. PMID: 15205622.

5. Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963; 45-A(1):1–14. PMID: 14040773.

6. Lee SC, Shim JS, Seo SW, Lim KS, Ko KR. The accuracy of current methods in determining the timing of epiphysiodesis. Bone Joint J. 2013; 95-B(7):993–1000. PMID: 23814256.

7. Sheehy L, Felson D, Zhang Y, et al. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011; 19(1):58–64. PMID: 20950695.

8. Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989; 7(1):132–137. PMID: 2908904.

9. Inan M, Chan G, Bowen JR. Correction of angular deformities of the knee by percutaneous hemiepiphysiodesis. Clin Orthop Relat Res. 2007; 456:164–169. PMID: 17065845.

10. Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FO. Failure of Orthofix eight-Plate for the treatment of Blount disease. J Pediatr Orthop. 2009; 29(1):57–60. PMID: 19098648.

11. Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007; 27(3):253–259. PMID: 17414005.
12. Shin SJ, Cho TJ, Park MS, et al. Angular deformity correction by asymmetrical physeal suppression in growing children: stapling versus percutaneous transphyseal screw. J Pediatr Orthop. 2010; 30(6):588–593. PMID: 20733425.
13. Wiemann JM 4th, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop. 2009; 29(5):481–485. PMID: 19568021.

14. Khoury JG, Tavares JO, McConnell S, Zeiders G, Sanders JO. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007; 27(6):623–628. PMID: 17717460.

15. Blount WP. A mature look at epiphyseal stapling. Clin Orthop Relat Res. 1971; 77:158–163. PMID: 5140445.
16. Metaizeau JP, Wong-Chung J, Bertrand H, Pasquier P. Percutaneous epiphysiodesis using transphyseal screws (PETS). J Pediatr Orthop. 1998; 18(3):363–369. PMID: 9600565.
Fig. 1
Schematic presentation for the correctable angle by asymmetrical lateral proximal tibia epiphysiodesis.
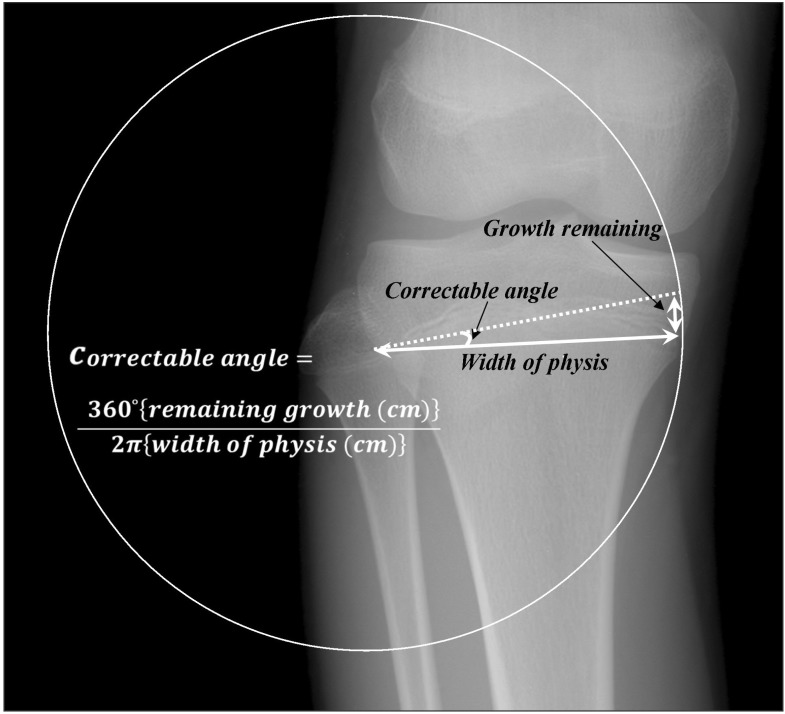
Fig. 2
Comparison of the correction angle between the calculated expectation values and actual values. CCA: calculated correctable angle, ACA: actual correction angle at final follow-up.
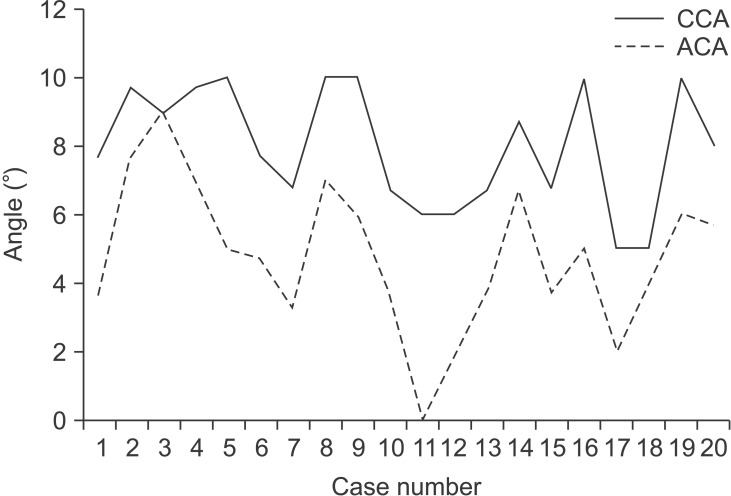
Fig. 3
Case number 3. A 10.3-year-old girl (bone age). (A) Preoperative radiograph. (B) Perfect alignment was achieved 2 years postoperatively when skeletal maturity was reached. *Hip-knee-ankle angle.
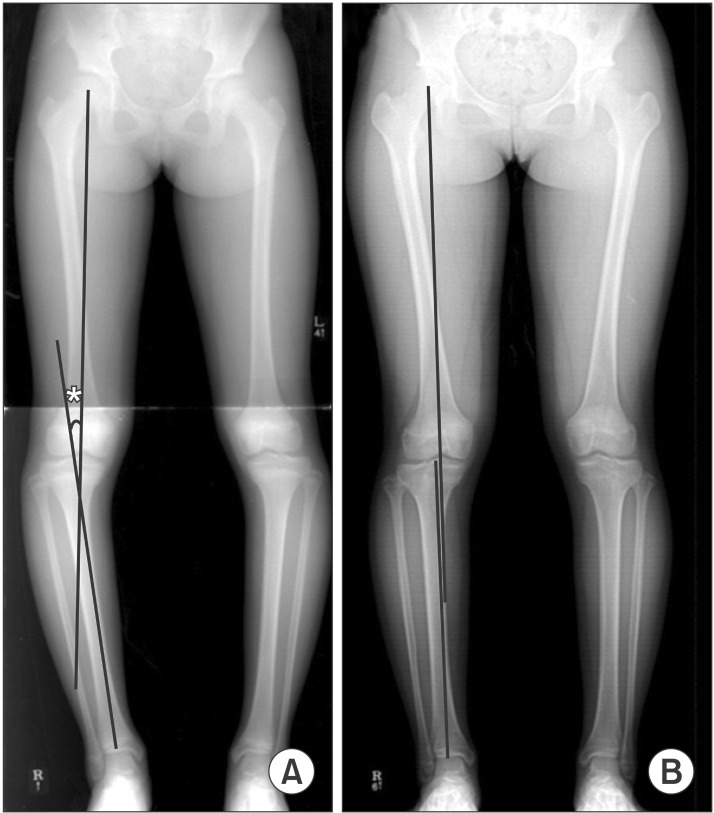
Fig. 4
Case number 11. A 12.3-year-old girl (bone age). (A) Preoperative radiograph. (B) There was no improvement of angular deformity at final follow-up. *Hip-knee-ankle angle.
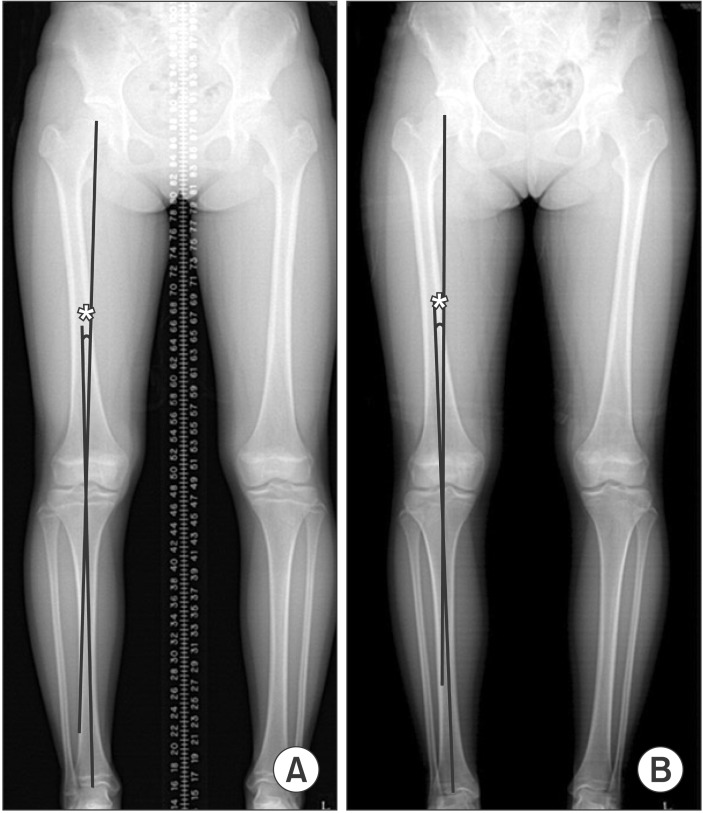
Table 1
Preoperative Patient Demographic Characteristics




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download