Abstract
We presented a surgical technique including a suture bridge technique with relatively small incision for the reduction and fixation of posterior ligament avulsion fractures. A suture anchor was used to hold the avulsed fragment and a knotless anchor was used to continuously compress the bony fragment into the fracture site, thereby maintaining reduction during healing.
Avulsion fractures of posterior cruciate ligament (PCL) represent a specific form of PCL injuries.1) Improper treatment of this injury results in an incompetent PCL that leads to knee instability and osteoarthritis.2) Therefore, previous reports recommend surgical treatment of displaced tibial avulsion fractures of the PCL for achieving anatomical reduction and knee stability.3456) Many operative methods of these fractures are reported. Conventional techniques using direct posterior or posteromedial approach are widely used despite the potential risk of complication, such as damage to the neurovascular structure, tearing of the gastrocnemius muscle and scarring of the wound.78) Arthroscopic surgery has an advantage of less soft tissue damage, however, it requires specialized equipment and experience.345)
Optimal fixation method is another controversial issue. Cancellous screws or cannulated screws are generally used for open reduction and internal fixation.7) However, screw fixation is indicated only for the large and noncomminuted fragment.7) Small or comminuted fragments are difficult to fix; in addition, there is a potential risk of fragmentation of the fracture fragment. In this study, we introduced a surgical technique, consisting of open reduction using posteromedial approach and internal fixation with suture bridge technique for tibial avulsion fracture of the PCL.
The indications for our approach were as follows: (1) isolated PCL avulsion fracture; and (2) posterior tibial sag present at 90° of knee flexion. Intra-articular lesions except PCL avulsion fracture were excluded using preoperative magnetic resonance image because of posteromedial approach and the consequential prone position. Operations were carried out under epidural or general anesthesia. A C-arm device was used to avoid the penetration of growth plate by the anchors in pediatric or adolescent patients. Patients were placed in the prone position, with the knee flexed 20° to 30°. An oblique incision of < 10 cm was made between semitendinosus tendon and medial head of the gastrocnemius (Fig. 1A). The medial head of the gastrocnemius was held laterally to expose the posterior capsule of the knee joint. Capsulotomy with an L-shaped incision was made longitudinally and then extended laterally to expose the fracture site (Fig. 1B). After debridement of fracture site, 2 suture based anchors (3.5 mm; Biomet Sports Medicine, Warsaw, IN, USA) were inserted into the superomedial and superolateral region of the fracture site. Sutures were passed through the osteotendinous junction in a mattress fashion and then tied. Each suture limb from the proximal row was placed through the hole at the end of the push-lock device (3.5 mm; Bio-PushLock, Arthrex Inc., Naples, FL, USA). Pilot holes for the push-lock device were created using a punch just inferior to the distal edge of the fracture site. A pushlock device was inserted into the pilot hole while maintaining a constant tension. After the device was fully engaged in the pilot hole, the sutures were cut. The use of a knotless anchor provides a compressive force and consequently fixes the reduced avulsion fragment strongly to the fracture bed (Fig. 1C-E). The wound was closed in layer, and a sterile dressing was applied. If the patients were children, the anchors were inserted so as not to penetrate a physeal plate.
A well-padded plaster splint was applied to the knee at 5° to 10° of flexion. On the first day, after surgery, the drain was removed and patients were encouraged to start quadriceps muscle strengthening exercise and begin non-weight bearing walking using crutches. After 2 weeks, protected range of motion exercise was started and partial weight bearing ambulation using crutches was permitted with locked brace in full extension. Six weeks later, the brace was unlocked and the patients began full weight bearing ambulation. At 8 weeks, the brace was removed and patients were encouraged to increase activity gradually.
A 20-year-old man presented with a right knee injury resulting from a motor vehicle accident. Clinical examination revealed a swollen knee, limited range of motion and posterior tibial sag at 90° on knee flexion. The operation was performed 2 days after the injury. The knee range of motion was 135° with a flexion 135° and flexion contracture 0° after 2 weeks postoperatively. Bony union was achieved after 4 months postoperatively. The patient was able to return to his usual daily activities after postoperative 6 months (Fig. 2).
A 13-year-old boy presented with left knee injury resulting from a fall. Clinical examination revealed hemarthrosis of the knee, limited range of motion, and posterior tibial sag. The operation was performed 1 day after the injury. The knee range of motion was 140° with flexion 140° and flexion contracture 0° after 4 weeks postoperative. Bony union was achieved after 3 months postoperative. The patient returned to his previous sports activities (Fig. 3).
Currently, open reduction or arthroscopic fixation is more commonly used in treatment of displaced PCL tibial bony avulsion.3456) The latter has both advantages and disadvantages. Since the site of attachment of the PCL to the tibia is located deep within the posterior tibial plateau, multiple arthroscopic sutures and tunnels are required, making the procedure more challenging and difficult. Furthermore, some authors reported that arthroscopic fixation using suspensory device needs a sizeable drill hole that may break thinner bone fragments.9) Open reduction can be performed with a traditional S-shaped approach, but this incision is associated with injury to adjacent neurovascular structures. In contrast, we used a less invasive posteromedial approach, which had several advantages, including exposure of the posterior capsule through the gap between the medial head of the gastrocnemius and the semitendinosus muscle. With the approach in this study, it is possible to minimize risks of damage to vessels and nerves, as well as providing satisfactory exposure of the fracture site.
Similar methods using posteromedial approach with suture anchors are previously reported.6) These studies used 2 suture anchors and fixed bony fragment by knotting with the sutures of 2 suture anchors. However, we used suture bridge fixation technique with suture anchors and sutureless anchors. The most important advantage of the present suture bridge fixation technique with posteromedial incision, is its indication for use regardless of the thickness, size, and comminution of bony fragment. This technique is similar to the double-row, trans-osseous equivalent or suture bridge techniques for rotator cuff repair or internal reduction and fixation of greater tubercle fractures of the humerus. It allows for a simple reproducible anatomic reduction and compression of the fracture fragment, even though the fragment is small or comminuted. Furthermore, suture anchor is relatively small, as compared to other fixation devices, such as cannulated screws, wires, sutures, and absorbable screws. In addition, no second operation is required to remove the fixation device. The anchor also offers strong purchase, and the attached suture can resist strong tension, resulting in reliable fixation. Previous study on anterior cruciate ligament avulsion fracture, reported that suture bridge construct provides superior fixation with regard to ultimate load, as compared with standard screw fixation and suture fixation in biomechanical analysis of suture bridge fixation for tibial eminence fractures.10) Similarly, the suture bridge mattress fixation in this study may provide enough ultimate load and compressive force to the avulsed fragment and thus maximize the surface area for bony healing. Furthermore, there is no risk of causing comminution.
In conclusion, the results of the study indicated that the posteromedial approach, combined with suture anchors, is a suitable treatment for isolated tibial avulsion fractures of the PCL.
Figures and Tables
Fig. 1
Posterior view of the right knee. (A) An oblique incision between semitendinosus tendon and medial head of the gastrocnemius. (B) The medial head of the gastrocnemius (arrow) is held laterally to expose the posterior capsule of the knee joint. Subsequently, capsulotomy with a longitudinal L-shaped incision is made and extended laterally to expose the fracture site. The forceps hold a bony fragment of the posterior cruciate ligament tibial attachment. (C) Fixation technique of the suture bridge method, with proximal to the left and distal to the right of the photo. (D) Illustration showing the position of the anchors in the coronal plane. (E) Illustration showing the position of the anchors in the sagittal plane.
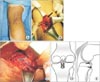
Fig. 2
Preoperative lateral simple radiograph (A) and computed tomography scan (B) of displaced posterior cruciate ligament avulsion fracture in a 20-year-old male. The arrow shows the bony fragment of posterior cruciate ligament avulsion fracture. (C) Postoperative lateral radiograph showing a healed avulsion fracture after surgical treatment using a suture bridge technique.

Fig. 3
(A) Preoperative lateral radiograph of displaced posterior cruciate ligament avulsion fracture in a 13-year-old male. The arrow shows the bony fragment of posterior cruciate ligament avulsion fracture. (B) Preoperative magnetic resonance imaging scan showing a thinner bone fragment. (C, D) Intraoperative fluoroscopic views showing the position of the anchors inserted so as not to penetrate a physeal plate. (E) Postoperative lateral radiograph showing the healed avulsion fracture after surgical treatment using a suture bridge technique.

References
1. Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME. MR imaging of the posterior cruciate ligament: normal, abnormal, and associated injury patterns. Radiographics. 1995; 15(3):551–561.

2. Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999; 27(3):276–283.

3. Horas U, Meissner SA, Heiss C, Schnettler R. Arthroscopic fixation of posterior cruciate ligament avulsion fractures: a new minimally invasive technique. Knee Surg Sports Traumatol Arthrosc. 2010; 18(6):781–783.

4. Kim SJ, Shin SJ, Cho SK, Kim HK. Arthroscopic suture fixation for bony avulsion of the posterior cruciate ligament. Arthroscopy. 2001; 17(7):776–780.

5. Wajsfisz A, Makridis KG, Van Den Steene JY, Djian P. Fixation of posterior cruciate ligament avulsion fracture with the use of a suspensory fixation. Knee Surg Sports Traumatol Arthrosc. 2012; 20(5):996–999.

6. Zhang X, Cai G, Xu J, Wang K. A minimally invasive postero-medial approach with suture anchors for isolated tibial avulsion fracture of the posterior cruciate ligament. Knee. 2013; 20(2):96–99.

7. Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res. 1990; (254):216–219.

8. Torisu T. Isolated avulsion fracture of the tibial attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 1977; 59(1):68–72.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download