Abstract
Background
Several tendon graft and fixation methods have been introduced in medial patellofemoral ligament (MPFL) reconstruction for recurrent patellar dislocation. The purpose of this study was to evaluate the results of MPFL reconstruction using a gracilis autograft fixation without bone tunnel in patients with recurrent patellar instability.
Methods
Nine patients (four males and five females) diagnosed with recurrent patellar instability from July 2009 to January 2013 and had MPFL reconstruction using a gracilis autograft were included. The average age of the patients was 24.6 years (range, 13 to 48 years), and the average follow-up period was 19.3 months (range, 12 to 30 months). For every patient, femoral attachment was fixed using suture anchors securing the patella by suturing the periosteum and surrounding soft tissue. Clinical evaluation included the Kujala, Lysholm, and Tegner scores; in addition, patients were examined for any complication including recurrent dislocation. The congruence angle and patella alta were assessed radiologically before and after surgery.
Results
The Kujala score improved from an average of 42.7 ± 8.4 before surgery to 79.6 ± 13.6 (p = 0.008) at final follow-up; the Lysholm score improved from 45.8 ± 5.7 to 82.0 ± 10.5 (p = 0.008); and the Tegner score improved from 2.8 ± 0.8 to 5.6 ± 1.5 (p = 0.007). The Insall-Salvati ratio changed from 1.16 ± 0.1 (range, 0.94 to 1.35) before surgery to 1.14 ± 0.1 (range, 0.96 to 1.29; p = 0.233) at the final follow-up without significance. The congruence angle significantly improved from 26.5° ± 10.6° (range, 12° to 43°) before surgery to -4.0° ± 4.3° (range, -12° to 5°; p = 0.008) at final follow-up. Subluxation was observed in one patient and hemarthrosis occurred in another patient 2 years after surgery, but these patients were asymptomatic.
In the past, risk of recurrent patellar dislocation was mostly attributed to anatomic factors including trochlear dysplasia, patella alta, excessive lateral patellar tilt, and excessive tibial tubercle-trochlear groove (TT-TG) distance. However, recent studies reveal the critical role of retinacular restraints, i.e., the medial patellofemoral ligament (MPFL), in patellofemoral stability. MPFL injury is reportedly identified in most patients with recurrent patellar dislocation.12) However, in many cases, primary repair of the MPFL is insufficient to recover appropriate tensile strength.3) Therefore, in the past few years, the important role of MPFL reconstruction is emphasized with development of many diverse techniques for securing stability of the patellofemoral joint.45) Remarkable developments have been made especially in graft choice and fixation methods, but determining the best method remains controversial.
Many graft materials for MPFL reconstruction have been introduced, including autologous semitendinosus tendon,6) gracilis,7) quadriceps tendon,89) patellar tendon,10) tibialis anterior allograft,11) and bioactive synthetic ligament,12) which were stronger than the native MPFL.13) The fixation methods introduced for MPFL reconstruction include sutures,14) suture anchors,15) spike washers,6) staples,16) interference screws,17) and EndoButtons.18) Pain occurs in 10% to 57% of implant fixations due to the implant (patella and femoral attachment site).1920) Patellar fracture is uncommon but usually relates to the use of bone tunnels for graft positioning and attachment.21)
We hypothesized that good results could be obtained through adequate fixation strength of the graft with soft tissue suture without a bone tunnel, based on reports of patellar fracture due to making a bone tunnel in the relatively small patella. Furthermore, better results are expected using a gracilis tendon graft closer to native MPFL strength, as compared to graft material that is stronger than the MPFL, which may cause increased patellofemoral contact pressure in flexion in case of inadequate graft positioning.
The purpose of this study was to evaluate the results of a patella fixation method using soft tissue suturing during MPFL reconstruction with a gracilis autograft fixation without bone tunnel in patients with recurrent patellar instability.
Thirteen patients diagnosed with recurrent patellar instability who underwent MPFL reconstruction using a gracilis autograft by one surgeon from July 2009 to January 2013 were evaluated. Four patients were excluded due to concurrent osteotomy of tibial tuberosity. Surgery was indicated when the patients did not show improvement on conservative treatment. The conservative treatment was defined by quadriceps setting exercise, closed kinetic chain exercise, and range of motion applying a patella brace during 6 months. Surgical indications suggested by Arendt22) are trochlear dysplasia type A or normal trochlea, no trochlear spur, a tubercle-sulcus angle between 0° and 10° valgus, and patella alta measurement < 1.4 (Insall-Salvati ratio). All patients had normal range of the horizontal distance between the tibial tubercle and the center of the groove (TT-TG distance). The four men and five women had an average age of 24.6 years (range, 13 to 48 years). Treatment sites included six left and three right knees, and the average follow-up period was 19.3 months (range, 12 to 30 months). The mechanism of injury was indirect in all nine cases. Single- and double-bundle reconstructions were conducted in five and four cases, respectively (Table 1). This study was approved by the Institutional Review Board of out institute (IRB File No. 2015-03-025-001).
For evaluation, we surveyed the Kujala, Lysholm, and Tegner scores before and after surgery. At the last follow-up, the incidence of recurrent dislocation, pain at the MPFL reconstruction site, range of motion of the knee joint, and signs of complications such as arthrofibrosis were evaluated. All patients had radiographs of the knee, including anteroposterior, 30° flexed lateral, and Merchant views, before and after surgery. The flexion and lateral radiographs were examined for signs of patella alta (Insall-Salvati ratio > 1.2) and trochlear dysplasia.23) Sulcus angles and congruence angles were measured and patellar dysplasia (type III and IV categories according to Baumgartl 24)) was evaluated on the Merchant views. Wilcoxon signed-rank tests were used to compare Kujala, Lysholm, and Tegner scores, Insall-Salvati ratios, and congruence angles before and after surgery. Significance was defined as a p-value < 0.05. The radiologic measurement was made by one surgeon who did not perform the MPFL reconstructions.
We first determined the sliding and tilting of the patella, cartilage state, and occurrence of any sign of a loose body using arthroscopy, and treated for any identified lesion before surgery. Approximately 3 cm longitudinal incision was made 2 cm medial to the tibial tubercle, and the gracilis tendon was checked at the deep portion of the sartorius fascia. The fascia was then incised to detach the gracilis tendon using a tendon stripper. Muscle tissues were removed from the collected tendon and a whip stitch was placed at each end.
Next, an approximately 4 cm longitudinal incision was made at the upper medial two thirds of the patella; and the medial retinaculum was examined by detaching subcutaneous tissue and fat. After making a submuscular tunnel at the lower portion of vastus medialis obliquus for penetration of the graft tendon, approximately 2 cm longitudinal incision was made to expose the distal portion of the adductor tubercle. Using fluoroscopy, the isometric point was marked slightly anterior to an elongation of the posterior femoral cortex in between the proximal origin of the medial condyle and the most posterior point of Blumensaat's line.15) This was followed by suture anchor fixation (Fig. 1). After fixing an end of the graft tendon with the thread attached to the suture anchor, the graft tendon was passed through the submuscular tunnel, and the graft end was sutured around the periosteum of the patella using No. 2 Ethibond (Ethicon, Somerville, NJ, USA) while keeping the knee joint bent in a 45° angle (Fig. 2). Subsequently, lateral retinacular release was carried out in 4 cases in which the tightness of the lateral retinaculum was maintained after MPFL reconstruction.
Depending on the severity of subluxation, single-bundle reconstruction was performed in five cases, and double-bundle reconstruction was performed in four cases. For single-bundle reconstruction, suturing was performed from the upper one-third of the patellar medial border as the starting point to the patellar midportion; and for double-bundle reconstruction, suturing was performed from the upper end and midpoint of the patellar medial border as the starting points to the patellar midportion. The lateral margin of the patella was displaced to coincide with the margin of the lateral femoral condyle, to confirm appropriate tension of the graft tendon. The graft was secured for suturing after holding an end of the graft tendon and patella with forceps. After successful fixation of the graft tendon, the lower border of the vastus medialis obliquus was advanced distally and laterally and sutured to the upper and medial border of the patella with the upper margin of the graft (Fig. 3). Finally, patellar stability was verified in various angles while moving the knee joint, and patellar tracking was confirmed by watching the patella motion under arthroscopy (Fig. 4). A medial retinacular imbrication (medial reefing) was carried out in four cases because of the persistent subluxation on knee flexion.
All patients wore a knee immobilizer for 2 weeks after surgery and performed quadriceps setting exercises. Thereafter, they began range of motion exercises to achieve a goal of 90° flexion for 6 weeks after surgery along with partial weight-bearing exercises. Subsequently, full weight bearing, full range of motion, and open kinetic chain exercises were permitted. The patients wore the knee brace until 3 months after surgery. In principle, light sports activities were allowed at 3 months after surgery, and all sports activities were allowed at 6 months after surgery, depending on the condition of muscle recovery.
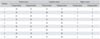
At the final follow-up examination, all patients had achieved full range of motion. The Kujala score was improved from an average of 42.7 ± 8.4 before surgery to 79.6 ± 13.6 (p = 0.008) at the final follow-up; the Lysholm score improved from 45.8 ± 5.7 to 82.0 ± 10.5, respectively (p = 0.008); and the Tegner score improved from 2.8 ± 0.8 to 5.6 ± 1.5, respectively (p = 0.007) (Table 2). The Insall-Salvati ratio was changed from 1.16 ± 0.1 (range, 0.94 to 1.35) before surgery to 1.14 ± 0.1 (0.96 to 1.29), without significance (p = 0.233), at the final follow-up. The congruence angle significantly decreased from 26.5° ± 10.6° (range, 12° to 43°) before surgery to -4.0° ± 4.3° (range, -12° to 5°; p = 0.008) at the final follow-up (Table 3). Patellar subluxation occurred in one patient who carried out both lateral release and medial reefing with a congruence angle of 4.8°, but the patient did not complain of any specific symptoms in daily activity (Fig. 5). Another patient had recurrent hemarthrosis 2 years after the surgery. He currently maintains a normal life without recurrence or symptoms after arthroscopic treatment.
We obtained good clinical and radiographic results without recurrence of subluxation or symptom in patients with recurrent patellar dislocation with MPFL reconstruction with a gracilis autograft using a soft tissue suturing method ion the patellar surface.
The MPFL has a mean tensile strength of 208 N and a stiffness of 8 N/mm as the primary soft tissue stabilizer preventing lateral patellar translation for the initial 30° of knee flexion.13) A prerequisite of graft tendon selection for MPFL reconstruction is that the stiffness of the graft tendon must be similar to that of the native MPFL, but greater strength is more desirable.22) However, the currently used graft tendon has a much higher strength and stiffness than the native MPFL. Mountney et al.3) reported possible problems related to patellar alignment arising from the use of over-tensioning when a hamstring graft was employed. Therefore, the gracilis tendon used in this study, is mainly used currently due to its similarity to the native MPFL.25)
Diverse methods are proposed including sutures,14) spiked washers,6) staples,16) interference screws,17) suture anchors,15) EndoButtons, and suture fixation using a docking technique 26) for fixation of the graft tendon to femur and patella Fixation using implants may cause multiple complications. Some authors reported that pain due to implants develops in 10% to 57% of patients,1620) and pain might arise from irritation at the insertion site by screws and anchors used for fixation. Moreover, fracture of the adductor tubercle may occur at the femoral tunnel during reconstruction,20) and several cases of iatrogenic fracture of the patella have also been reported.1417) Therefore, Petersen and Zantop 27) developed implant-free fixation technique; whereas, other authors introduced methods to fix the graft onto surrounding soft tissue instead of bone.142829) In this study, such implant-related complications were prevented by suturing the graft onto the soft tissues, as well as the periosteum of the patella. Moreover, even though an implant was not used, the soft tissue fixation is also advantageous because a bone tunnel can result in continuous pain after surgery.
After surgery, patellar dislocation should not occur with knee motion, and further flexion should be allowed without excessive constraint. Therefore, maintaining appropriate graft tension is important during fixation. Many studies recommended 25% to 50% or 10 mm lateral displacement of the patella.917) In addition, the fixation angle is critical. Many researchers conducted reconstructions with 20° to 90° of flexion, but the ideal angle remains controversial.91420) The MPFL plays a role of checkrein only during early flexion of the knee, hence, it may be desirable to conduct graft fixation at 30° to 40° of flexion.13) However, similar to Lee et al.,30) bony stability was achieved if the knee joint was bent at an angle larger than 50° to 60° after monitoring the patellar tracking under arthroscopy during motion. Moreover, Type A trochlea dysplasia was observed in 4 of 9 patients, while Type III patellar dysplasia was noted in three patients. Therefore, influence of the abnormal bone shapes on the biomechanics of the MPFL could not be excluded. This implies that fixation at a flexion condition less than 30° may not be beneficial. Therefore, MPFL was fixed to the graft at 45° of flexion and patellar tracking was observed at various angles to check for any subluxation or tilting in this study.
Drez et al.28) conducted a retrospective review of implant-free fixation; they reported 93% good and fair results in 19 cases of soft tissue suturing onto the tibia and femur with 31.5 months of follow-up with Fulkerson, Kujala, and Tegner scores of 93, 88, and 6.7, respectively. Ellera Gomes et al.14) reported 94% good and fair results in 16 cases of soft tissue suturing onto the femur with a median follow-up of more than 5 years. Lee et al.29) showed good results in 9 cases of suturing soft tissue onto the patella and femur with an average follow-up of 17.6 months with International Knee Documentation Committee, Kujala, Lysholm, and Tegner scores of 81.1, 81.4, 84.9, and 5.1, respectively. In this study, the MPFL reconstruction yielded good results with Kujala, Lysholm, and Tegner scores of 79.6, 82.0, and 5.6, respectively, as well adequate radiologic results with satisfactory congruence angles for most patients. Abnormal findings were detected in one patient, although the congruence angle improved from 36° to 5°. However, the patient was satisfied with the result of surgery and experienced no limitations in daily life. In another patient, recurrent hemarthrosis occurred at 2 years after the surgery, but was treated successfully with arthroscopic debridement. His knee has been in a normal condition without recurrence or complications such as infection, nerve injury, or stiffness for the last 12 months.
Limitations of this study included the lack of a biomechanical study of tensile strength of MPFL reconstruction using the soft tissue suture method, absence of a control group, a short-term follow-up period, case series, retrospective study, and relatively small number of patients. In addition, only one surgeon measured the radiologic results. The inconsistency of treatment may be another limitation because both single-bundle and double-bundle methods were used. Future studies are required to supplement these findings with biomechanical studies and long-term follow-up.
In medial patellofemoral ligament reconstruction to treat recurrent patellar dislocation, a patella fixation technique with a gracilis autograft and soft tissue suturing showed good results at short-term follow-up.
In conclusion, we achieved good results with a patellar fixation technique using MPFL reconstruction using a gracilis autograft employing soft tissue suturing without bone tunnel in patients with recurrent patellar dislocation.
Figures and Tables
Fig. 1
Femoral attachment site. (A) Under fluoroscopy, an isometric point marked the junction of the front of an extension leading from the posterior cortex of the femur, the distal portion of the posterior origin of the medial femoral condyle, and the proximal portion of the posterior point of Blumensaat's line suggested by Schottle et al.15) (B) This was followed by suture anchor fixation.

Fig. 2
Soft tissue suture of the patellar attachment site. After fixing the end of the graft tendon with the thread attached to the suture anchor, the graft tendon was passed through the submuscular tunnel and the double gracilis graft was sutured around the periosteum of the patella using No. 2 Ethibond (Ethicon) while keeping the knee joint bent in 45°.

Fig. 3
Vastus medialis obliquus (VMO) imbrication. After successful fixation of the graft tendon, the lower border of the VMO was advanced distally and laterally and sutured to the upper and medial borders of the patella with the upper margin of the graft.

Fig. 4
Radiographs. (A) Preoperative Merchant view shows subluxated patella. (B) Final follow-up radiograph shows well-located patella.
Fig. 5
Subluxation in one patient. (A) Preoperative Merchant view shows subluxated patella. (B) Final follow-up radiograph shows subluxation with a congruence angle of 5°, but the patient did not complain of any specific symptoms in daily activities.
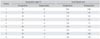
Table 1
Demographic Data
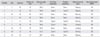
Table 2
Clinical Results
References
1. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002; 9(2):139–143.

2. Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996; 24(1):52–60.
3. Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005; 87(1):36–40.

4. Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993; 75(5):682–693.

5. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998; 26(1):59–65.

6. Nomura E, Inoue M. Hybrid medial patellofemoral ligament reconstruction using the semitendinous tendon for recurrent patellar dislocation: minimum 3 years' follow-up. Arthroscopy. 2006; 22(7):787–793.

7. Quirbach S, Smekal V, Rosenberger RE, El Attal R, Schottle PB. Anatomical double-bundle reconstruction of the medial patellofemoral ligament with a gracilis autograft. Oper Orthop Traumatol. 2012; 24(2):131–139.

8. Fink C, Veselko M, Herbort M, Hoser C. MPFL reconstruction using a quadriceps tendon graft: part 2: operative technique and short term clinical results. Knee. 2014; 21(6):1175–1179.
9. Noyes FR, Albright JC. Reconstruction of the medial patellofemoral ligament with autologous quadriceps tendon. Arthroscopy. 2006; 22(8):904.e1–904.e7.

10. Witonski D, Keska R, Synder M, Sibinski M. An isolated medial patellofemoral ligament reconstruction with patellar tendon autograft. Biomed Res Int. 2013; 2013:637678.
11. Cheatham S, Kolber MJ, Hanney WJ. Rehabilitation of a 23-year-old male after right knee arthroscopy and open reconstruction of the medial patellofemoral ligament with a tibialis anterior allograft: a case report. Int J Sports Phys Ther. 2014; 9(2):208–221.
12. Berruto M, Ferrua P, Uboldi F, et al. Medial patellofemoral ligament reconstruction with bioactive synthetic ligament is an option: a 3-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2014; 22(10):2419–2425.

13. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003; 10(3):215–220.

14. Ellera Gomes JL, Stigler Marczyk LR, Cesar de Cesar P, Jungblut CF. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004; 20(2):147–151.

15. Schottle P, Schmeling A, Romero J, Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009; 129(3):305–309.

16. Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000; 7(4):211–215.

17. Christiansen SE, Jacobsen BW, Lund B, Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008; 24(1):82–87.

18. Schock EJ, Burks RT. Medial patellofemoral ligament reconstruction using a hamstring graft. Oper Tech Sports Med. 2001; 9(3):169–175.

19. Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007; 35(11):1851–1858.

20. Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006; 34(8):1254–1261.

21. Thaunat M, Erasmus PJ. Recurrent patellar dislocation after medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008; 16(1):40–43.

22. Arendt EA. MPFL reconstruction for PF instability: the soft (tissue) approach. Orthop Traumatol Surg Res. 2009; 95:8 Suppl 1. S97–S100.

23. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994; 2(1):19–26.

24. Baumgartl F. Anatomical and clinical importance of the femoropatellar joint. Zentralbl Chir. 1966; 91(14):506–516.
25. Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM. Surgical biomechanics of the patellofemoral joint. Arthroscopy. 2007; 23(5):542–553.

26. Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009; 37(10):2021–2027.

27. Petersen W, Zantop T. Eine neue methode zur patellaren fixation von MPFL-transplantaten. Arthroskopie. 2009; 22(3):237–240.

28. Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001; 17(3):298–306.

29. Lee HS, Choi JY, Ha JK, et al. Anatomical reconstruction of the medial patellofemoral ligament: development of a novel procedure based on anatomical dissection. J Korean Orthop Assoc. 2011; 46(6):443–450.

30. Lee KB, Song SY, Lee SJ, Son WS. Medial patellofemoral ligament reconstruction using the autogenous hamstring tendon for recurrent patellar instability: a preliminary report. J Korean Knee Soc. 2010; 22(2):93–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download