Abstract
Background
In the present study, we aimed to compare clinical and radiographic outcomes between hook plate fixation and coracoclavicular (CC) ligament reconstruction for the treatment of acute unstable acromioclavicular (AC) joint dislocation.
Methods
Forty-two patients who underwent surgery for an unstable acute dislocation of the AC joint were included. We divided them into two groups according to the treatment modality: internal fixation with a hook plate (group I, 24 cases) or CC ligament reconstruction (group II, 18 cases). We evaluated the clinical outcomes using a visual analog scale (VAS) for pain and Constant-Murley score, and assessed the radiographic outcomes based on the reduction and loss of CC distance on preoperative, postoperative, and final follow-up plain radiographs.
Results
The mean VAS scores at the final follow-up were 1.6 ± 1.5 and 1.3 ± 1.3 in groups I and II, respectively, which were not significantly different. The mean Constant-Murley scores were 90.2 ± 9.9 and 89.2 ± 3.5 in groups I and II, respectively, which were also not significantly different. The AC joints were well reduced in both groups, whereas CC distance improved from a mean of 215.7% ± 50.9% preoperatively to 106.1% ± 10.2% at the final follow-up in group I, and from 239.9% ± 59.2% preoperatively to 133.6% ± 36.7% at the final follow-up in group II. The improvement in group I was significantly superior to that in group II (p < 0.001). Furthermore, subluxation was not observed in any case in group I, but was noted in six cases (33%) in group II. Erosions of the acromion undersurface were observed in 9 cases in group I.
Acromioclavicular (AC) joint dislocation is a relatively common injury that accounts for 50% of all sports-related shoulder injuries and occurs five times more frequently in men.1,2) The Rockwood classification system, which is based on the magnitude and direction of dislocation, is usually used to classify AC joint dislocations. Rockwood types I and II respond to short-term conservative treatment. However, surgical treatment is mandatory for types IV-VI and decisions regarding conservative versus surgical treatment are controversial for type III injuries.3,4,5,6)
Various surgical options have been developed for AC joint dislocation, including fixation across the AC joint, coracoacromial ligament transfer (Weaver-Dunn procedure), coracoclavicular (CC) fixation, and AC or CC reconstruction. However, the clinical superiority of these procedures remains debatable, and various complications have been reported.7,8,9)
Currently, two modern techniques-hook plate fixation and CC ligament reconstruction using a synthetic ligament-are widely used due to their good reported clinical outcomes.9,10) Hook plates have been developed as an alternative fixation method for fractures of the distal clavicle and dislocations of the AC joint and are used to promote natural healing of the ligaments.11,12,13) CC ligament reconstruction using a synthetic ligament has some advantages, including strong initial fixation compared with the native ligament, early mobilization, and no donor site morbidities.14,15,16) The main advantages are that implant removal is unnecessary and there is no risk of metal migration or implant failure.17) These two methods had their own advantages. However, to our knowledge, no comprehensive comparative study has addressed the clinical outcomes and complications associated with acute AC joint injury. Accordingly, in the present study, we aimed to evaluate and compare the clinical and radiographic outcomes between these two treatment modalities in patients with acute AC joint dislocation.
We retrospectively reviewed a consecutive series of 67 patients treated for traumatic AC joint dislocation using either hook plate fixation or CC ligament reconstruction with a synthetic ligament between March 2005 and December 2011. Patients with a Rockwood type V lesion and minimum clinical follow-up of 12 months were included, whereas those with a chronic AC joint lesion, history of shoulder stiffness, AC joint arthritis, or who received previous surgical intervention to the shoulder girdle were excluded. We excluded patients who underwent surgery more than 4 weeks after injury (13 patients), were lost to follow-up before 12 months postoperatively (11 patients), or had a history of previous shoulder surgery (1 patient).
Finally, forty-two patients were included in the current study. There were 33 men and nine women with an average age of 40.5 ± 13.4 years. Twenty-four patients were treated with hook plate fixation (Synthes GmbH, Oberdorf, Switzerland) (group I) and 18 were treated with CC ligament reconstruction (LIGASTIC, Orthomed, Orthomed, Nice, France) (group II). The mean age was 38.8 ± 14.2 years in group I and 42.2 ± 12.3 years in group II (p = 0.353). In addition, there were no significant differences between the two groups in terms of sex, dominant arm, injury mechanism, time from injury to surgery, or follow-up period (respectively, p > 0.05). The study protocol was approved by the Institutional Review Board of the Kyungpook National University Hospital.
For hook plate fixation, surgery was performed under general anesthesia, with the patient in a beach chair position and the injured limb freely mobile. After cutting the deltotrapezial fascia, the joint was reduced by direct visualization and fluoroscopy. Thereafter, an appropriately sized hook plate was chosen and applied with the hook positioned posterior-inferior with respect to the acromion. Finally, the plate was fixed to the clavicle using several screws.
For CC ligament reconstruction, graft material was passed around the coracoid process using a guidewire. Two anteroposterior tunnels were drilled through the clavicle using a motorized drill bit. The oblique medial tunnel was located downward and backward, whereas the oblique lateral tunnel was located upward and forward.
Progressive rehabilitation was initiated after 2 weeks. All patients were allowed to use their arm for daily activities, and nonrestricted movement was allowed at 6 weeks postoperatively. Strength-related activities were permitted at three months postoperatively. The hook plate was removed in a second surgery at a mean of 7.8 ± 1.3 months postoperatively.
Clinical outcomes were assessed using a visual analog scale (VAS) for pain and Constant-Murley score by one independent observer who was not involved in the current study.18) Final clinical assessments were performed at a mean of 16.7 ± 3.7 months postoperatively. The mean follow-up period was 16.0 ± 12.8 months in group I and 17.4 ± 4.3 months in group II (p = 0.280).
Radiological assessment was evaluated and compared with the contralateral side using preoperative, postoperative, and final follow-up plain radiographs. The images were analyzed and standardized to assess CC distance (height in percent to the contralateral shoulder between the upper border of the coracoid process and the inferior cortex of the clavicle). We considered increases in CC distance on final follow-up radiographs of 0%-50%, 50%-100% and > 100% with respect to the contralateral side as mild reduction loss, subluxation, and redislocation, respectively.12)
At final follow-up, subacrominal erosions were evaluated by plain radiographs in hook plate group. Subacromial erosion was identified in nine cases. During hook plate removal, diagnostic arthroscopy was performed in these 9 patients to assess erosion severities by the hook. We divided these patients into two groups based on the extent of erosion: mild erosion (defined when only the tip of the hook penetrated the subacromial cortex) or severe erosion (defined when the entire hook penetrated the subacromial cortex) (Fig. 1).
Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), and null hypotheses were rejected when p-values were < 0.05. Descriptive statistics, Student t-test, and the Mann-Whitney U-test were used to determine outcome differences between the two treatment groups.
With regard to the clinical outcomes, the mean VAS scores at the final follow-up were 1.6 ± 1.5 and 1.3 ± 1.3 in groups I and II, respectively (p = 0.543). The mean Constant-Murley scores were 90.2 ± 9.9 and 89.2 ± 3.5 in groups I and II, respectively (p = 0.630) (Table 1).
With regard to the radiographic outcomes, CC distances were reduced in both groups: from 215.7% ± 50.9% preoperatively to 106.1% ± 10.2% at the final follow-up in group I, and from 239.9% ± 59.2% preoperatively to 133.6% ± 36.7% at the final follow-up in group II; the improvement in group I was significantly superior to that in group II (p < 0.001) (Figs. 2 and 3).
With regard to the maintenance of reduction of the AC joint, recurrent subluxation was not observed in group I, but was evident in 6 cases (33%) in group II at the final follow-up. There was no redislocation on final follow-up radiographs in either group.
Subacromial erosion was evaluated during diagnostic arthroscopy in nine cases (37.5%, 9/24) in group I. Six of the nine cases were considered mild erosion, whereas three were considered severe erosion. There were no significant differences in VAS score (1.5 ± 1.0 vs. 1.7 ± 1.7; p = 0.789) or Constant-Murley score (88.2 ± 9.3 vs. 91.5 ± 10.4; p = 0.443) at the final follow-up between patients with erosion (n = 9) and without erosion (n = 15) in group I (Table 2). In radiologic finding, there was no difference in initial CC distance and final CC distance (p = 0.086 and p = 0.148, respectively).
Calcification of the CC ligament and osteolysis of the distal clavicle were observed in 2 patients in group II (Fig. 4); however, no clinical inferiority was observed in these cases. No other complications requiring surgical revision occurred in either group.
Traditionally, Kirschner wires or tension band wiring, a plate, and screws are used to treat AC joint dislocation. However, various complications, such as metal breakage, loosening, recurrence of instability, migration, and neurovascular system damage, have been reported using these techniques.
Recently, the hook plate has become widely used as it enables secure fixation against rotational, horizontal, and vertical forces, as well as early joint motion. Furthermore, it avoids direct joint injury because it is not fixed by pins or screws into the AC joint.19,20,21) Several previous studies have reported satisfactory clinical results of hook plate fixation for AC joint dislocation.13,22) However, removal of the plate is recommended due to subacromial impingement and implant failure.23) In addition, stress concentration at the hooks and altered joint kinematics may cause erosion of the acromion and fracture of the distal clavicle or scapula.8,24) In the present study, 37.5% (9/24) of patients demonstrated mild or severe subacromial erosion. Although there were no differences in clinical and radiologic outcome based on the presence of erosion, the relatively frequent occurrence might imply a considerable disadvantage of hook plate fixation.
Reconstruction of the AC joint using a suture, synthetic ligament, or allograft can be used to treat AC joint dislocation without violating the AC joint, and provides a better surgical solution from anatomic and biomechanical perspectives.25,26,27) In the present study, we used a synthetic polyester ligament, which has a thin microporous woven structure that promotes fibrous connections, and is known to possess sufficient mechanical properties to allow early rehabilitation.14) In addition, its nonabsorbable material causes fewer biologic reactions, reduces the rate of complications associated with metal fixation, and does not require subsequent implant removal. Previous studies have reported good clinical results of synthetic ligament reconstruction.14,28) Recently, arthroscopy-assisted synthetic ligament reconstruction with less morbidity has been introduced and the investigation of the presence of concomitant joint pathologies is being performed.29) However, recurrence of AC joint instability is a frequent problem. In the present study, 33% of patients showed subluxation, which is similar to the rate observed with other materials, such as polydioxanone and anchors. We believed that their problem originated from the reconstruction of solitary CC ligament without AC ligament not being able to stabilize the AC joint completely. Despite the subclinical symptoms exhibited by these patients, we need careful considerations with the potential for radiographic recurrence. Furthermore, with this technique, correct tunnel positioning should be conducted meticulously to avoid malpositioning which would induce remnant instability.
Our study has limitations that are inherent to similar, retrospective, nonrandomized studies. In particular, the hook plate group was not sufficiently large to draw statistical significance based on the degree of subacromial erosion. The relatively high incidence of subacromial erosion might have been due to delayed removal of the hook plate.
In the present study, internal fixation using a hook plate and synthetic ligament reconstruction yielded comparable clinical results in patients with acute unstable dislocation of the AC joint. However, based on radiographic maintenance of reduction, hook plate fixation is considered superior, despite the higher incidence of subclinical acromial erosion with this technique. Therefore, we believe that hook plate fixation is a better treatment modality, and we recommend that more detailed investigations should be conducted on this topic.
Figures and Tables
Fig. 1
Diagnostic arthroscopy during hook plate removal, showing subacromial erosion. (A) Mild erosion was considered present when only the tip of the plate penetrated the subacromial cortex. (B) severe erosion was considered present when the entire hook penetrated the subacromial cortex.

Fig. 2
Serial radiographs of a 25-year-old man treated with hook plate fixation, showing good maintenance of joint reduction after plate removal. (A) Preoperative. (B) Three months postoperative. (C) After plate removal.

Fig. 3
Serial radiographs of a 49-year-old man treated with synthetic ligament reconstruction, showing good joint reduction and maintenance of joint reduction. (A) Preoperative. (B) Two months postoperative.
Fig. 4
Radiographs obtained 16 months postoperatively, showing mild loss of reduction and distal clavicular osteolysis after synthetic ligament reconstruction.

Table 1
Clinical Outcome of Each Group
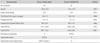
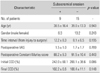
Table 2
Comparison according to Presence of Subacromical Erosions
References
1. Oussedik S. Injuries to the clavicle and acromioclavicular joint. Br J Hosp Med (Lond). 2007; 68(4):M68–M70.

2. Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: anatomy, diagnosis, and treatment. Phys Sportsmed. 2011; 39(1):116–122.

3. Ceccarelli E, Bondi R, Alviti F, Garofalo R, Miulli F, Padua R. Treatment of acute grade III acromioclavicular dislocation: a lack of evidence. J Orthop Traumatol. 2008; 9(2):105–108.

4. Duan X, Zhang H, Zhang H, Wang Z. Treatment of coracoid process fractures associated with acromioclavicular dislocation using clavicular hook plate and coracoid screws. J Shoulder Elbow Surg. 2010; 19(2):e22–e25.

5. Phillips AM, Smart C, Groom AF. Acromioclavicular dislocation: conservative or surgical therapy. Clin Orthop Relat Res. 1998; (353):10–17.
6. Spencer EE Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007; 455:38–44.
7. Bannister GC, Wallace WA, Stableforth PG, Hutson MA. The management of acute acromioclavicular dislocation: a randomised prospective controlled trial. J Bone Joint Surg Br. 1989; 71(5):848–850.

8. Hoffler CE, Karas SG. Transacromial erosion of a locked subacromial hook plate: case report and review of literature. J Shoulder Elbow Surg. 2010; 19(3):e12–e15.

9. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011; 20:2 Suppl. S70–S82.

10. Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJ. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009; 17(4):207–219.

11. Di Francesco A, Zoccali C, Colafarina O, Pizzoferrato R, Flamini S. The use of hook plate in type III and V acromioclavicular Rockwood dislocations: clinical and radiological midterm results and MRI evaluation in 42 patients. Injury. 2012; 43(2):147–152.

12. Eschler A, Gradl G, Gierer P, Mittlmeier T, Beck M. Hook plate fixation for acromioclavicular joint separations restores coracoclavicular distance more accurately than PDS augmentation, however presents with a high rate of acromial osteolysis. Arch Orthop Trauma Surg. 2012; 132(1):33–39.

13. von Heideken J, Bostrom Windhamre H, Une-Larsson V, Ekelund A. Acute surgical treatment of acromioclavicular dislocation type V with a hook plate: superiority to late reconstruction. J Shoulder Elbow Surg. 2013; 22(1):9–17.

14. Jeon IH, Dewnany G, Hartley R, Neumann L, Wallace WA. Chronic acromioclavicular separation: the medium term results of coracoclavicular ligament reconstruction using braided polyester prosthetic ligament. Injury. 2007; 38(11):1247–1253.

15. Nuchtern JV, Sellenschloh K, Bishop N, et al. Biomechanical evaluation of 3 stabilization methods on acromioclavicular joint dislocations. Am J Sports Med. 2013; 41(6):1387–1394.

16. Yoo YS, Seo YJ, Noh KC, Patro BP, Kim DY. Arthroscopically assisted anatomical coracoclavicular ligament reconstruction using tendon graft. Int Orthop. 2011; 35(7):1025–1030.

17. Mares O, Luneau S, Staquet V, Beltrand E, Bousquet PJ, Maynou C. Acute grade III and IV acromioclavicular dislocations: outcomes and pitfalls of reconstruction procedures using a synthetic ligament. Orthop Traumatol Surg Res. 2010; 96(7):721–726.

18. Bafus BT, Hughes RE, Miller BS, Carpenter JE. Evaluation of utility in shoulder pathology: correlating the American Shoulder and Elbow Surgeons and Constant scores to the EuroQoL. World J Orthop. 2012; 3(3):20–24.

19. Flinkkila T, Ristiniemi J, Lakovaara M, Hyvonen P, Leppilahti J. Hook-plate fixation of unstable lateral clavicle fractures: a report on 63 patients. Acta Orthop. 2006; 77(4):644–649.

20. Hackenbruch W, Regazzoni P, Schwyzer K. Surgical treatment of lateral clavicular fracture with the "clavicular hooked plate". Z Unfallchir Versicherungsmed. 1994; 87(3):145–152.
21. Meda PV, Machani B, Sinopidis C, Braithwaite I, Brownson P, Frostick SP. Clavicular hook plate for lateral end fractures: a prospective study. Injury. 2006; 37(3):277–283.

22. Salem KH, Schmelz A. Treatment of Tossy III acromioclavicular joint injuries using hook plates and ligament suture. J Orthop Trauma. 2009; 23(8):565–569.

23. ElMaraghy AW, Devereaux MW, Ravichandiran K, Agur AM. Subacromial morphometric assessment of the clavicle hook plate. Injury. 2010; 41(6):613–619.

24. Chiang CL, Yang SW, Tsai MY, Kuen-Huang Chen C. Acromion osteolysis and fracture after hook plate fixation for acromioclavicular joint dislocation: a case report. J Shoulder Elbow Surg. 2010; 19(4):e13–e15.

25. Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010; 19:2 Suppl. 37–46.

26. Jones HP, Lemos MJ, Schepsis AA. Salvage of failed acromioclavicular joint reconstruction using autogenous semitendinosus tendon from the knee. Surgical technique and case report. Am J Sports Med. 2001; 29(2):234–237.

27. Rios CG, Mazzocca AD. Acromioclavicular joint problems in athletes and new methods of management. Clin Sports Med. 2008; 27(4):763–788.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download