Abstract
Ponseti clubfoot treatment has become more popular during the last decade because of its high initial correction rate. But the most common problem affecting the long-term successful outcome is relapse of the deformity. Non-compliance with Ponseti brace protocol is a major problem associated with relapse. Although more comfortable braces have been reported to improve the compliance, they all have the same design and no significant changes have been made to the protocols. After refinement in the Ponseti method and emphasizing the importance of brace to parents, the relapse rate has been markedly decreased. Nevertheless, there are patients who do not have any recurrence although they are not completely compliant with the brace treatment, whereas other patients have a recurrence even though they are strictly compliant with the brace treatment. The aim of this article is to review the relapse of clubfoot and the function of the brace and to develop an individualized brace protocol for each patient by analyzing the mechanism of the brace and the biomechanical properties of muscles, tendons, and ligaments.
Congenital talipes equinovarus, i.e., congenital clubfoot, is one of the most common musculoskeletal abnormalities in childhood which affect the lower limb and can be challenging to treat. The deformity has four components: equinus, forefoot adductus, hindfoot varus, and cavus. Nowadays, conservative treatment is generally accepted as the first choice for correction of clubfoot and the most popular approach is the Ponseti method which consists of serial manipulations and specific casting along with or without an Achilles tenotomy.1,2,3,4) After full correction is achieved, the remaining treatment includes the use of a foot abduction orthosis (FAO) to maintain the correction for approximately 4 years.1,3,4,5,6,7) However, relapse of the deformity has proved to be quite challenging after full correction. Non-compliance with the Ponseti brace protocol was reported to be the leading cause of relapse and has a direct effect on the success of treatment.5) The most common reason for non-compliance with the brace treatment is discomfort.
In 1963, Ponseti and Smoley4) reported the results in 67 patients with 94 clubfeet who were treated at their clinic by means of serial manipulations and castings. The initial success rate was about 80%. This method was refined later on and has been used throughout the world particularly since 1990s after the long-term successful result was reported during an average of more than 30-year follow-up.1,8) This method was introduced in more and more medical centers.3,5,9,10) Herzenberg et al.9) treated 34 feet, of which only 1 foot required extensive posteromedial release after serial casting with or without percutaneous Achilles tenotomy. Colburn and Williams11) reported an initial correction rate of 95%. Moreover, other medical centers in different nations also reported that 92%-100% clubfeet in their patients, whose age at the time of presentation was usually less than 1 year, responded to initial manipulation and casting as described in the Ponseti protocol.1,6,10,12,13,14,15) Verma et al.16) found that the Ponseti method was also effective in children between the ages of 1 to 3 years, and they reported an initial successful rate of about 89%. The Ponseti method is also effective in the non-idiopathic clubfoot. Morcuende et al.17) and Boehm et al.18) reported an initial correction rate of 94% and 100%, respectively. Gerlach et al.19) reported that they obtained initial full correction in 96% of the myelomeningocele-related clubfeet. Also 86% of clubfeet in patients undergoing posteromedial release were responsive to the Ponseti method.20)
During the period of brace wear, great concern has been expressed about recognition and prevention of the relapse of clubfoot deformity because in nearly all of the cases recurrence of clubfoot deformity occurs during this phase. After the final cast, the foot is ready for bracing. The bar-connected brace maintains the completely corrected foot in 60 to 70 degrees of external rotation on the affected side and in 30 to 40 degrees of external rotation on the normal side. The bar should be bent 5 to 10 degrees with the convexity away from the child to hold the feet in a valgus position and it should be of sufficient length so that the heels of the shoes are at shoulder width. The shoes maintain the foot in 10 to 15 degrees of dorsiflexion while wearing the brace.1,3,4,5,6,7,12,15,21,22,23,24) The foot appears to be over-corrected into abduction, but it is not a real overcorrection, but full abduction.24) The brace should be worn full time (day and night) for the first 3 months after the final cast is removed. After that, the child should wear the brace for 12 hours at night and 2 to 4 hours during the day, for a total of 14 to 16 hours during each 24-hour period. This protocol is continued until the child is 3 to 4 years of age.7,24) After the successful management with the Ponseti method, the patient has a functional, pain-free, plantigrade foot, with good mobility and without calluses, and does not need to wear modified shoes.
As described by Ponseti, the proper use of this method can be clearly divided into two phases. The first phase is the correction phase and the second phase is the maintenance phase.3,4,12) During the second phase, traditional well-fitted, open-toed, high-top straight-last shoes attached to a Denis Browne bar or a bar-connected FAO are used to avoid recurrence of the deformity. If a patient is not compliant with the brace treatment, he/she is more likely to have a relapse than the compliant patient.3,5,6,12,15,21,25) The Iowa group defined recurrence as the reappearance of any of the components of the deformity, including either equinus, forefoot adductus, hindfoot varus, or cavus.12) Some reports considered recurrence of clubfoot after treatment using the Ponseti method as any deformity that required additional casting and/or surgical intervention. This is almost similar to the definition of the Iowa group.3,6,14,25,26)
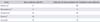
Many studies suggested that non-compliance with the brace treatment was closely associated with recurrence of the deformity.3,6,10,13,14,15,16,21,22,25,26,27) In addition, a few researches suggested that low educational level of parents, annual family income of < US $20,000, and Native American ethnicity were all significant risk factors for the recurrence of deformity following correction with the Ponseti method.3,14,15,21) However, non-compliance or poor-compliance with the Ponseti brace protocol was identified as the leading cause of relapse and had a direct effect on the success of treatment.5) With respect to the non-compliance rate and relapse rate, a variety of medical centers and researches reported different findings. Many authors reported that brace intolerance ranges from 0% to 51%.3,6,7,8,10,20,25,27) In the research by Haft et al.,25) the non-compliance rate was 49% and patients who did not adhere to the bracing protocol were 5 times more likely to have a relapse in comparison with children who wore the brace regularly. Dobbs et al.3) found that the non-compliance rate was 41% and children who discontinued wearing the brace were 183 times more likely to have recurrence of clubfeet. These two results from the study by Avilucea et al.14) were 36% and 120 times. Abdelgawad et al.6) observed a relapse in 60% of clubfeet in children who were not able to use the brace as prescribed compared to a relapse in 16% of clubfeet in patients who were compliant with the brace protocol during 3 or more than 3 years of follow-up. Moreover, Morcuende et al.12) from the University of Iowa suggested that non-compliance was associated with a 17 times greater odds of relapse compared with compliance. Despite as high as 43% non-compliance rate, the patients who were not in compliance with the brace protocol had 20 times more likelihood of relapse in our institute (the data not yet published). All of the children in these studies were prescribed the brace of same type, which kept the feet in abduction and dorsiflexion, but the results varied enormously (Table 1). Why?
We analyzed the publications and identified the following four causes.
(1) Variation in bracing protocol from different studies, in which the orthosis was worn full-time (22 to 23 hours a day) for two or three months and then at night (10 to 12 hours a day) for two to four years.1,4) Morcuende et al.12) suggested that the brace should be used on a full-time basis for 2-3 months and at night and during nap time for 3 to 4 years. More authors recommended using the brace for 23 hours during the first 3 months and subsequently at night time and nap time only without providing a definite time period.6,12,14,16) Some authors recommended wearing the brace only at night-time after using the orthosis full-time until the age of 2 to 4 years.10,28,29) Bouchoucha et al.23) suggested that the brace should be worn full time (23 hours per day) for 3 months, followed by a period of part-time wearing of the brace for 12 to 14 hours a day. Chen et al.7) prescribed the same brace protocol as that prescribed by Staheli.24) Although these discrepancies are not large, when the parents follow these protocols, it may result in significant differences.
(2) There is no consensus on the definition of 'non-compliance' or 'compliance.' Morcuende et al.12) suggested non-compliance when the foot abduction brace was not used for at least 10 hours a day. Dobbs et al.3) suggested non-compliance on complete discontinuation of the use of the orthosis. Abdelgawad et al.6) defined non-compliance as complete discontinuation of the use of the FAO. Avilucea et al.14) defined non-compliance as premature discontinuation of the use of the brace during the maintenance phase. Panjavi et al.15) defined non-compliance as lack of full-time bracing in the first 3 months, or at night time 9 months thereafter. Different definitions may result in different findings.
(3) In most of the researches, the time period for which the orthosis was used was calculated based on the parents' information, telephonic interview, or clinical follow-up.3,14,15) The parents may not accurately remember the exact time period during which the brace was used; therefore, leading to inaccurate recording of the brace wearing time. Currently, in none of the researches a heat or pressure sensor is mounted onto the orthosis to calculate the exact brace wearing time, which is similar to the brace treatment in patients with adolescent idiopathic scoliosis.30) Apart from this, when a child is crying it is difficult to distinguish between the pain due to these shoes and whether the child is annoyed. But many parents often assume that the child is crying due to the former reason, and hence they adjust the brace frequently. It is then difficult to determine the compliance with brace wearing and orthosis when the children are crying. Inappropriate wearing of the brace does not maintain the correction effectively. Therefore, the time recorded is not the same as the actual effective brace wearing time.
(4) Not all of the medical centers can provide handouts25) and conduct interviews through telephone calls to assess whether the patients are following the recommended brace protocol, especially in developing countries.14) Actually, these measures can improve the brace wear compliance, and thus the brace wearing time can be the same as that suggested in the prescribed brace protocol.
Ponseti and Smoley4) realized that recurrence of the deformity occurred almost immediately following complete correction when he first started using this new manipulation technique for management of clubfoot. The initial data from the Iowa group showed that the relapse rate was 56% because the initial brace protocol developed by the Iowa group recommended brace wearing only for about 2 years.4) When the recommendation for brace wearing was changed to 4 years the recurrence rate showed a drastic reduction.10) Hyperabduction in the final cast and emphasis on brace wearing led to improvement in the short-term and long-term success rates.1,4,8,12) Especially, the brace wearing time is a crucial factor during the whole treatment. Non-compliance results in insufficient brace wearing time and inappropriate brace wearing increases the risk of relapse.3,6,12,14,25) Hence, many braces improved the adherence to postcorrective bracing (Table 2). Ponseti and Smoley4) recommended the use of original Denis Browne splint, which consists of a bar with an L-shaped metal foot plate at either end with high-top shoes and well-molded heels, to avoid relapse of clubfoot. Markell brace has been the most popular FAO at the University of Iowa for decades. The device consists of a pair of open-toed shoes mounted on a length-adjustable aluminum bar by foot plates. Foot plates are attached to the bar by a steel bolt that fixes a serrated disk, which allows for the adjustment of rotation of the foot plates (Fig. 1A).24) The Mitchell-Ponseti brace which was developed by John Mitchell and Ignacio Ponseti includes detachable shoes and soft silicone inserts with a leather support and three leather straps.24,31) The Mitchell-Ponseti brace may be more attractive to some parents and more comfortable for children, but it does not provide better clinical results than the Denis Browne bar (Fig. 1B and C).31) Chen et al.7) described an articulated FAO design that allows active flexion and extension of each leg separately while maintaining the necessary external rotation of the foot. The articulating FAO is well tolerated by patients and results in a higher compliance rate and a lower complication rate than the traditional FAO.7) The Steenbeek brace was initially designed and produced for use in the developing countries because of its low cost24) and it was found to be effective in maintaining the correction.23) Furthermore, a much lighter FAO was prescribed to the neonates younger than 3 months of age in our institute (Fig. 1D). The newly designed FAO can either facilitate the compliance with orthosis wearing or cut down the cost. They have the same effect, i.e., preventing the recurrence of deformity. They all maintain the affected foot in 60 to 70 degrees of external rotation and in 10 to 15 degrees of dorsiflexion.24)
Ponseti32) suggested that relapses were caused by the same pathology that initiated the deformity rather than being a sign of undercorrection. Histomorphometric results indicated that the talar deformity was not the primary lesion. Histological and immunohistochemical findings showed that the posterior and medial ankle ligaments of clubfeet appeared to be the site of the earliest changes. They lost their spatial orientation of cells and collagen fibres and the soft tissues had contracted.33) Therefore, Ponseti2) hypothesized that the relapses may be related to retracting fibrosis of the ligaments and musculotendinous units of the posterior and medial ankle. At the end of three weeks of casting, the foot is abducted to an exaggerated amount and kept in an adequate degree of dorsal flexion. Then the children start using the FAO and its purpose is to maintain the correction after the final cast.2,12) A comparative research between the use of the bar-connected FAO and the ankle foot orthosis (AFO) to prevent relapse follow correction of idiopathic clubfoot with the Ponseti method suggested that the bar-connected FAO appeared to be very important in preventing recurrence of clubfeet treated with the Ponseti method and this cannot be achieved with an AFO because 60 to 70 degrees of external rotation, which is accomplished by the FAO, is necessary to stretch the medial soft tissues.26) Conversely, the AFO can only keep the foot in a neutral position without stretching the medial soft tissue. As we mentioned above the posterior and medial soft tissues are involved in the pathogenesis and relapse.2,32,33)
Currently, according to the recommended brace protocol, all of the patients should wear the brace for 12 hours at night and 2 to 4 hours in the middle of the day, for a total of 14 to 16 hours during each day. This protocol is continued until the child is 3 to 4 years of age.7,24) The age at which bracing can be stopped remains unclear. Some of the patients, who were not compliant with the brace treatment, did not have recurrence of the deformity. However, some other patients had recurrence even though they were compliant with bracing.3,6,14,25) In addition, we found that some children in our institute wore the FAO for less than 8 hours after 2 years of age (the data is not published); but, they did not have a recurrence. The question has been raised as to the need for all of the patients to adhere to the same bracing protocol. Some studies suggested that severity of the deformity and the age of the patient at the initiation of treatment did not have a significant effect on the risk of recurrence.21) Does the diversity of posterior and medial ankle soft tissues among individuals determine the minimum brace wearing time without the occurrence of a relapse?
The medial soft tissues remain stretched out only if the FAO is used after three weeks of casting.24) When a clubfoot is placed in the FAO, the affected foot is kept in 60 to 70 degrees of external rotation and in 10 to 15 degrees of dorsal flexion,24) and the posterior and medial ankle soft tissues such as tibialis anterior, tibialis posterior, flexor digitorum longus, flexor hallucis longus muscle and tendon, deltoid and spring ligaments which are involved in the deformity of clubfoot are under static stretching by the FAO. Thacker et al.5) found that the Dimeglio score of completely corrected clubfeet in the compliant group improved significantly during the brace maintenance phase. The mean score decreased from 3.5 to 1.0 between the time of FAO application and 6 to 9 months of follow-up. Bouchoucha et al.23) reported that a slight improvement in the amount of dorsal flexion of the ankle and a global decrease in stiffness was observed after full-time bracing. These findings suggested that the FAO can not only maintain the complete correction achieved by the cast but can also reduce the stiffness of soft tissues and increase the range of motion of the ankle. Another research suggested that although performing stretching exercises during the maintenance phase is not recommended in the original Ponseti method, it can still reduce the recurrence rate.15)
In fact, the weekly long-leg cast also provides a type of stretch which can gradually correct the deformity and decrease the stiffness of the ankle. Tendons and ligaments exhibit time-dependent behavior which is called creep and stress relaxation. Creep is defined an the time-dependent elongation of a tissue when subjected to a constant load, meanwhile stress relaxation is defined as the time-dependent decrease in load when the tissue is subjected to constant elongation.34) Hence, the manipulative correction in the Ponseti method can be consider as the creep; on the other hand, the cast immobilization and the FAO wearing can be consider as stress relaxation. We all know that although the cast can fully correct the deformity, sufficient time is needed to prevent a relapse.1,4,8,12) As the FAO is designed to maintain the foot as that by a post-tenotomy cast,24) when the foot is placed in the FAO the posterior and medial ankle ligaments and tendons are stretched and thus the stress relaxation begins. As time passes, the contractility of the ligaments and tendons which are involved in the primary deformity and recurrence decreases. Therefore, we can presume that when the contractility of all ligaments and tendons of the ankle reaches static equilibrium the deformity does not recur. Another research by Nakamura et al.35) suggested that a 4-week static stretch training program decreased the passive torque and increased the muscle-tendon junction (MTJ) displacement of the gastrocnemius at 30 degrees of dorsiflexion without causing changes in the muscle fascicle length. They thought that the increased MTJ displacement observed after the static stretch training program might be associated with factors other than muscle fiber length. When muscle fibers are immobilized under stretch, the immediate effect is that the fibers become longer and the constituent myofibrils lengthen. After several weeks, the whole muscle and fibers maintain their length. The sarcomere length returns to normal and the number of sarcomeres in the region of the MTJ increases. Therefore, time is needed for elongation of the soft tissues or for decreasing the contractility of tendons and ligaments. We know that different individual's have different tensile properties of the soft tissue;34) hence, the FAO wearing time for an individual may depend on the tensile properties. Therefore, the posteromedial soft tissues of clubfeet, which are presumed to have different characteristics, may need different time periods for changing their properties under stretch accomplished by using the FAO.
It has been universally agreed that the initial management of congenital clubfoot should be non-operative. The Ponseti method has been proved to be effective in this type of management by means of long-term follow-up evaluation. Nevertheless, relapse and its prevention still remain a great concern. Dr. Ignacio V. Ponseti of the University of Iowa developed a technique for the manipulative treatment of clubfeet based on the understanding of the anatomy and kinematics of the foot.14) This method consists of a number of the details including: (1) All the deformities are corrected simultaneously; the cavus is corrected together with the adduction; to elevate the first metatarsal and abduct the forefoot while applying counter-pressure with the thumb against the lateral aspect of the head of the talus; heel varus will be corrected when the entire foot is fully abducted under the talus, but the heel is never touched; residuary equinus is usually facilitated by a simple percutaneous tendoachilles tenotomy. (2) After full correction is achieved, the remaining treatment includes the use of bar-connected brace to maintain the correction and prevent relapse until the age of 3-4 years old.2,3,12,24,36) Although success has been achieved in obtaining the initial correction in clubfeet, maintaining the correction is more challenging. The most common problem is the poor compliance with brace wear. Many methods have been used to improve the compliance, such as reminding or motivating the parents14) and modifying the brace.7) But no level of motivation can compensate for an imperfect brace.24,31) Currently, the brace protocol is identical for all of the patients. The presence of collagen, vimentin, and myofibroblast-like cells in the thick, tight, and shortened medial and posterior tarsal ligaments seems to play an important role in the pathogenesis and relapse of the clubfoot deformity.32,33,37) It is important to use the FAO for stretching the posteromedial soft tissues and for preventing the relapse of deformity. Different tensile properties of posteromedial soft tissues may need different stretch time periods for preventing a relapse. Accordingly, researches on the time-dependent muscle, tendon, and ligament stretch may shed new light on the brace wearing time during the maintenance phase after complete correction with the Ponseti method.
In the future, it is important for clinicians to adhere to every details and principles of Ponseti method. Only following these details and principles as it was initially described can optimize its clinical outcomes. Moreover, future investigations on the different responses of the posterior and medial ankle soft tissues may led to improvement in the brace protocol. The offer of an individualized brace protocol is expected for each patient. And Ponseti method would be greatly optimized in this aspect.
Figures and Tables
References
1. Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am. 1980; 62(1):23–31.
2. Ponseti IV. Congenital clubfoot: fundamentals of treatment. Oxford: Oxford University Press;1996.
3. Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004; 86(1):22–27.
4. Ponseti IV, Smoley EN. The classic: congenital club foot: the results of treatment. 1963. Clin Orthop Relat Res. 2009; 467(5):1133–1145.
5. Thacker MM, Scher DM, Sala DA, van Bosse HJ, Feldman DS, Lehman WB. Use of the foot abduction orthosis following Ponseti casts: is it essential? J Pediatr Orthop. 2005; 25(2):225–228.
6. Abdelgawad AA, Lehman WB, van Bosse HJ, Scher DM, Sala DA. Treatment of idiopathic clubfoot using the Ponseti method: minimum 2-year follow-up. J Pediatr Orthop B. 2007; 16(2):98–105.
7. Chen RC, Gordon JE, Luhmann SJ, Schoenecker PL, Dobbs MB. A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop. 2007; 27(5):522–528.
8. Cooper DM, Dietz FR. Treatment of idiopathic clubfoot: a thirty-year follow-up note. J Bone Joint Surg Am. 1995; 77(10):1477–1489.
9. Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop. 2002; 22(4):517–521.
10. Lehman WB, Mohaideen A, Madan S, et al. A method for the early evaluation of the Ponseti (Iowa) technique for the treatment of idiopathic clubfoot. J Pediatr Orthop B. 2003; 12(2):133–140.
11. Colburn M, Williams M. Evaluation of the treatment of idiopathic clubfoot by using the Ponseti method. J Foot Ankle Surg. 2003; 42(5):259–267.
12. Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004; 113(2):376–380.
13. Changulani M, Garg NK, Rajagopal TS, et al. Treatment of idiopathic club foot using the Ponseti method: initial experience. J Bone Joint Surg Br. 2006; 88(10):1385–1387.
14. Avilucea FR, Szalay EA, Bosch PP, Sweet KR, Schwend RM. Effect of cultural factors on outcome of Ponseti treatment of clubfeet in rural America. J Bone Joint Surg Am. 2009; 91(3):530–540.
15. Panjavi B, Sharafatvaziri A, Zargarbashi RH, Mehrpour S. Use of the Ponseti method in the Iranian population. J Pediatr Orthop. 2012; 32(3):e11–e14.
16. Verma A, Mehtani A, Sural S, et al. Management of idiopathic clubfoot in toddlers by Ponseti's method. J Pediatr Orthop B. 2012; 21(1):79–84.
17. Morcuende JA, Dobbs MB, Frick SL. Results of the Ponseti method in patients with clubfoot associated with arthrogryposis. Iowa Orthop J. 2008; 28:22–26.
18. Boehm S, Limpaphayom N, Alaee F, Sinclair MF, Dobbs MB. Early results of the Ponseti method for the treatment of clubfoot in distal arthrogryposis. J Bone Joint Surg Am. 2008; 90(7):1501–1507.
19. Gerlach DJ, Gurnett CA, Limpaphayom N, et al. Early results of the Ponseti method for the treatment of clubfoot associated with myelomeningocele. J Bone Joint Surg Am. 2009; 91(6):1350–1359.
20. Nogueira MP, Ey Batlle AM, Alves CG. Is it possible to treat recurrent clubfoot with the Ponseti technique after posteromedial release?: a preliminary study. Clin Orthop Relat Res. 2009; 467(5):1298–1305.
21. Ramirez N, Flynn JM, Fernandez S, Seda W, Macchiavelli RE. Orthosis noncompliance after the Ponseti method for the treatment of idiopathic clubfeet: a relevant problem that needs reevaluation. J Pediatr Orthop. 2011; 31(6):710–715.
22. Porecha MM, Parmar DS, Chavda HR. Mid-term results of Ponseti method for the treatment of congenital idiopathic clubfoot: (a study of 67 clubfeet with mean five year follow-up). J Orthop Surg Res. 2011; 6:3.
23. Bouchoucha S, Smida M, Saied W, et al. Early results of the Ponseti method using the Steenbek foot abduction brace: a prospective study of 95 feet. J Pediatr Orthop B. 2008; 17(3):134–138.
24. Staheli L. Clubfoot: Ponseti management [Internet]. 3rd ed. Seattle, WA: Global HELP;2009. cited 2013 Nov 20. Available from: http://www.global-help.org/publications/books/book_cfponseti.html.
25. Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007; 89(3):487–493.
26. Janicki JA, Wright JG, Weir S, Narayanan UG. A comparison of ankle foot orthoses with foot abduction orthoses to prevent recurrence following correction of idiopathic clubfoot by the Ponseti method. J Bone Joint Surg Br. 2011; 93(5):700–704.
27. Bor N, Coplan JA, Herzenberg JE. Ponseti treatment for idiopathic clubfoot: minimum 5-year followup. Clin Orthop Relat Res. 2009; 467(5):1263–1270.
28. Segev E, Keret D, Lokiec F, et al. Early experience with the Ponseti method for the treatment of congenital idiopathic clubfoot. Isr Med Assoc J. 2005; 7(5):307–310.
29. Boehm S, Sinclair M. Foot abduction brace in the Ponseti method for idiopathic clubfoot deformity: torsional deformities and compliance. J Pediatr Orthop. 2007; 27(6):712–716.
30. Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010; 92(6):1343–1352.
31. Hemo Y, Segev E, Yavor A, Ovadia D, Wientroub S, Hayek S. The influence of brace type on the success rate of the Ponseti treatment protocol for idiopathic clubfoot. J Child Orthop. 2011; 5(2):115–119.
32. Ponseti IV. Relapsing clubfoot: causes, prevention, and treatment. Iowa Orthop J. 2002; 22:55–56.
33. Fukuhara K, Schollmeier G, Uhthoff HK. The pathogenesis of club foot: a histomorphometric and immunohistochemical study of fetuses. J Bone Joint Surg Br. 1994; 76(3):450–457.
34. Buckwalter JA, Einhorn TA, Simon SR. Orthopaedic basic science: biology and biomechanics of the musculoskeletal system. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons;2000. p. 581–616.
35. Nakamura M, Ikezoe T, Takeno Y, Ichihashi N. Effects of a 4-week static stretch training program on passive stiffness of human gastrocnemius muscle-tendon unit in vivo. Eur J Appl Physiol. 2012; 112(7):2749–2755.
36. Zhao D, Li H, Zhao L, Liu J, Wu Z, Jin F. Results of clubfoot management using the Ponseti method: do the details matter? A systematic review. Clin Orthop Relat Res. 2014; 472(4):1329–1336.
37. Sano H, Uhthoff HK, Jarvis JG, Mansingh A, Wenckebach GF. Pathogenesis of soft-tissue contracture in club foot. J Bone Joint Surg Br. 1998; 80(4):641–644.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download