Abstract
Purpose
Near-infrared fluorescence imaging with indocyanine green (ICG) has the potential to improve sentinel lymph node (SLN) mapping in breast cancer. In this clinical trial, we compared the potential value of ICG combined with blue dye with that of blue dye alone for detecting SLNs.
Methods
Patients undergoing SLN biopsy (SLNB) between November 2010 and November 2013 were included. Up to December 2011, SLNs were detected by using patent blue (PB) alone, and since January 2012, by using PB in combination with ICG. The patients were divided into the following two groups: group A (ICG-PB; n=96) and group B (PB; n=73), and SLN detection parameters were compared between the groups. All patients underwent level I and II axillary dissections after SLNB.
Results
In group A, the SLN detection rate was 96.9% (93/96), the accuracy of detection was 98.9% (92/93), and the false-negative rate (FNR) was 3.4% (1/29). In group B, the SLN detection rate was 84.9% (62/73), the accuracy of detection was 96.8% (60/62), and the FNR was 11.1% (2/18). The ICG-PB group showed significantly superior results compared to the PB group for SLN detection (p=0.005) and a greatly improved FNR.
The axillary lymph node status is the most significant prognostic factor in patients with breast cancer [1,2,3,4]. Sentinel lymph node biopsy (SLNB) is a well-established method for evaluating axillary node status [5]. Large validated studies, including the Axillary Lymphatic Mapping Against Nodal Axillary Clearance (ALMANAC) trial, have shown that SLNB in patients with breast cancer is a safe and reliable technique for accurate axillary lymph node staging [6].
SLNB is performed by using different techniques, such as injection of patent blue (PB) dye or radioactive colloids, or a combination of both [7]. A high rate of sentinel lymph node (SLN) detection is achievable by using these methods, but there is no consensus on the optimal technique [7,8]. The dye method has several benefits, including ease of use, cost effectiveness, and safety, but it has been reported that the detection rate is lower than that of the gamma probe method, or combined mapping with radiocolloids and blue dye [7]. Preoperative lymphoscintigraphy facilitates intraoperative identification of axillary nodes, but there are concerns about the limited availability and cost of radiocolloids, and the exposure of healthcare professionals to radiation [9,10]. In addition, the resolution of the lymphatic drainage pathway is poor when using radioisotope-based lymphoscintigraphy, and some surgeons prefer to use blue dye alone for SLN detection [11].
Studies have reported that indocyanine green (ICG) could be used for SLN detection in patients with breast cancer [12]. The photodynamic eye (PDE) readout of ICG allows clear visualization of the lymphatic drainage pathway, and offers accurate, real-time detection of the SLN during surgery [13]. However, few studies have reported the combined use of ICG with other tracers for SLN detection in patients with breast cancer.
Various factors can influence the outcome of SLNB, including the type of contrast agent used to mark SLNs. The aim of this study was to evaluate the clinical utility of using a combination of ICG with PB dye versus using blue dye alone for SLN detection in patients with breast cancer undergoing SLNB.
Preoperative diagnosis was determined on the basis of the results obtained with physical examination, mammography, ultrasonography, and core biopsy. Patients with a confirmed pathological diagnosis of early-stage breast cancer (N=169, all women), undergoing SLNB at the Breast Center of Dalian Central Hospital, were enrolled between November 2010 and November 2013. Up to December 2011, SLNs were detected by using PB dye alone, and since January 2012, by using a combination of PB and ICG. The patients were divided into group A (ICG-PB; n=96) and group B (PB; n=73). Inclusion criteria were histopathological diagnosis of breast cancer, a single lesion with a tumor diameter <3 cm, no previous breast or axillary surgery, and absence of clinically positive axillary lymph nodes. Axillary lymph node status was assessed before surgery by using ultrasonography with a 10-MHz linear transducer (Voluson 730 Expert; GE Healthcare, Chalfont St. Giles, UK). Exclusion criteria included previous surgeries and/or radiotherapy to the breast, neoadjuvant chemotherapy, and definite lymph node metastases, diagnosed on palpation and via ultrasonography. In patients diagnosed with ductal carcinoma in situ (DCIS) by using core needle biopsy, biopsy samples and imaging examinations were recommended to detect the SLN if the lesion was extensive or if palpable tumors were present, in order to avoid underestimating the patient's condition preoperatively. Written consent was obtained from all enrolled participants, and the study was approved by the institutional ethics committee of Dalian Central Hospital (IRB approval number: 2010003).
A 3-minute breast massage was performed following a subareolar injection of a 2.0-mL mixture containing ICG (10 mg) and PB (15 mg). Subsequent image acquisition was conducted by using a PDE (Hamamatsu Photonics, Hamamatsu, Japan) with the near-infrared light source provided by room fluorescent lighting (760 nm wavelength). The lymphatic transport of ICG was observed in real-time with fluorescence imaging for 5 to 10 minutes after the injection, by which time the ICG had generally reached the axillary lymph nodes. The fluorescence emitted by ICG was followed from the areola towards the axilla, and the observed subcutaneous lymphatic drainage pathway was marked on the skin at the point which the fluorescent signal disappeared. A skin incision was made at this point (Figure 1). All fluorescent and/or blue nodes were excised and regarded as SLNs.
After the administration of anesthesia, a 1% solution of PB (1 mL) was injected into the subareolar region and skin overlying the tumor. The whole breast was compressed and massaged for 5 minutes. All lymph nodes containing blue dye were harvested, and were considered the total population of SLNs.
Following SLNB, a level I and II axillary lymph node dissection was performed to verify axillary node status. Intraoperative frozen-section staining with haematoxylin and eosin (H&E) was performed. When this was negative, further serial sectioning was performed on paraffin-embedded tissue blocks. Ten sections were obtained from each block of tissue and stained with H&E, or immunostained for epithelial membrane antigen (EMA; DAKO, Glostrup, Denmark). Formalin-fixed, paraffin-embedded tissue sections of nonsentinel lymph nodes were stained with H&E.
Any remaining SLN tissue was formalin-fixed and paraffin-embedded for routine histopathological examination. The results of paraffin-embedded and frozen-section analysis were compared.
All data were analyzed by using the SPSS software statistical package for Windows version 12.0 (SPSS Inc., Chicago, USA). The Fisher exact test, chi-square test, and Student t-test were used to compare data between the two groups. p-values of ≤0.05 were considered statistically significant.
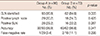
Characteristics of patients in groups A and B are presented in Table 1. There were 12 cases of DCIS with Tis stage in group A, and 11 cases of DCIS in group B, as determined from core biopsies taken preoperatively. However, postoperatively, six of 12 patients with Tis in group A, and six of 11 patients in group B had microinvasive carcinoma, as determined by assessment of paraffin-embedded tissue sections. The average number of SLNs detected in group A (3.8±0.9) was higher than that detected in group B (2.4±0.7).
Of the 96 SLNB procedures carried out in group A, 93 had SLNs successfully identified, an identification rate of 96.6% (93/96). There were 10 patients whose SLNs were identified only by using fluorescence. Thus, if blue dye alone had been used for the procedure, 10 patients would not have had SLNs identified, giving an identification rate of 86.4% (83/96). The false negative rate (FNR) was 3.4% (1/29), and the accuracy of detection was 98.9% (92/93) (Table 2). SLNs from four patients had micrometastases, with some of the corresponding axillary nodes also showing metastases. In contrast, 1 patient with micrometastasis in the axillary nodes had no positive SLNs, according to the final histology; this was a false-negative case. Twenty-eight patients in group A had detectable metastases in the SLNs, and three of these were fluorescence-positive but dye-negative. Two of the patients did not have metastases in lymph nodes other than SLNs, which were subsequently resected. Therefore, if ICG had not been used, the FNR would have reached 13.7% (4/29) (Table 3).
In group B, the SLN identification rate was 84.9% (62/73), the FNR was 11.1% (2/18), and the accuracy of detection was 96.8% (60/62). Micrometastases in the SLNs were detected in three patients, but the corresponding axillary nodes were micrometastases-free. In contrast, two patients with micrometastases in the axillary nodes had negative SLNs.
No statistically significant differences in the accuracy of detection were seen between the two groups. The SLN identification rate was significantly higher in group A than in group B (p=0.005). If ICG had not been used for the procedure in group A, there would have been no difference in the identification rate between the two groups (86.4% vs. 84.9%, p=0.778). There was a definite improvement in the FNR, from 11.1% to 3.4%, by using ICG, although there was no significant difference in this improvement between the two groups (p=0.296).
In recent years, there has been a focus on diagnostic and therapeutic benefits of lymphatic vessel and lymph node imaging for malignant and nonmalignant pathologies [14]. Lymphography, in preparation for SLNB, has come to the fore as a major field of application in lymphatic imaging for malignant neoplasia with potential lymphatic spread; it has also been shown to have a significant impact on overall prognosis [14,15].
Some studies have demonstrated an improved identification rate and lower FNR by using a combination of dye-based and radioisotope (RI) imaging [16]. McMasters et al. [17] reported an SLN identification rate of 98.0% and a FNR of 6.5%, when using a combination of RI (dermal injection) and isosulfan blue dye. The SLN identification rate when using dye-based methods alone, has been reported to be around 85% in a number of different studies, suggesting that the lower identification rate is intrinsic to the technique, and not related to the surgeon's performance [18].
ICG has been used as a tracer for over 40 years and has demonstrated an excellent safety profile in clinical use [19,20]. Kitai et al. [21] have previously demonstrated the utility of fluorescent imaging with ICG for SLNB in patients with breast cancer. Fluorescence-guided imaging with ICG has many advantages compared to conventional methods, including the combination of transcutaneous and in situ navigation, real-time lymphography, a low incidence of adverse reactions to ICG, and a high sensitivity, without the need for radiation [9,22]. Therefore, fluorescence imaging combines the advantages of the established radiocolloid and dye labeling methods for SLN detection.
In this study, all SLNs were identified exclusively by bright fluorescence and/or dye labeling (Figure 1). The identification rate of SLNs by using ICG-PB was similar to or better than previously reported rates obtained by using a gamma probe, or those by using a combination of a gamma probe and dye [8,23]. In addition, the ICG-PB guided detection rate was significantly better than PB-guided detection alone (p=0.005), and ICG-PB guided detection had the added advantage of transcutaneous real-time detection when using a PDE camera.
In the published literature, the FNR for SLNB when using PB alone is usually >5%, which, according to current guidelines, is considered unacceptable. The FNR in group B was >11%, considerably higher than the acceptable limit. Although the FNRs were not statistically different between the two methods in this study due to the relatively few false-negative results, the FNR was reduced with the use of ICG-PB, and this finding may be clinically meaningful. Therefore, the reduced FNR of <5%, obtained by using the combined technique in our study, is highly desirable and offers an excellent clinical benefit.
In our study, ICG-PB identified more SLNs per patient than PB alone, although the accuracy of detection between both techniques was comparable (p=0.341). The tendency for more SLNs to be identified by using ICG-PB is most likely due to the higher sensitivity of the ICG PDE device. In addition, Hojo et al. [24] suggested that an increased number of SLNs identified by using ICG could be due to the low molecular weight and high degree of diffusion of ICG that allows it to spread beyond the first SLN to the secondary draining lymph nodes, whereas the diffusion of PB may be limited.
During the procedure, a high number of SLNs were removed for analysis because a recent publication has shown that the examination of two nodes provides 91% to 98% accuracy of axillary nodal status, whereas the examination of four nodes provides >98% accuracy [25]. In four patients from group A, SLNs contained only micrometastases, while some of the axillary nodes removed were metastatic in these patients. This emphasizes the role of a thorough histopathological examination of SLNs for micrometastasis detection. There is an ongoing debate about whether every SLN-positive patient should undergo routine axillary lymph node dissection (ALND), especially in the case of micrometastasis [24,26]. The data presented here suggests that it would be safer to conduct ALND in all SLN-positive patients. In a small number of patients in group A, the PB dye did not detect metastases in the SLN, but in those patients, metastases were detected by ICG, suggesting that the dye method should be combined with the fluorescence method for cases that are difficult to diagnose.
A disadvantage of ICG is leakage and adaptation of ICG fluorescence that causes halation of the image, or an auto-fluorescent glow in the entire surgical field. When the first SLN is removed, ICG spreads throughout the surgical field, which can make identification of other fluorescent nodes difficult. In the current study, this problem was circumvented by ligating the main lymphatic duct at a site proximal to the first SLN, to avoid lymphatic fluid retention; ligation of the afferent lymphatic vessel prevents ICG from accumulating in the operative field.
There is a learning curve involved in the effective performance of SLNB [27,28]. SLNs can be detected more rapidly and precisely as a surgeon gains more experience of SLNB cases. The blue dye method is generally recognized as being more difficult to learn [29]. The addition of ICG fluorescence to blue dye enabled visualization of lymph flow from the breast to the axilla, and SLNs were identified and resected more rapidly by using this combined approach. The ICG method was particularly beneficial in difficult cases where SLNs were not readily identified by using the dye method.
Until recently, few studies have reported the combined use of ICG with other tracers for SLN detection in patients with breast cancer [24]. Although the initial data appear promising, no concrete data are available on FNRs because ALND was not performed.
This study demonstrated that SLNB by using the ICG-PB technique is feasible and safe for the intraoperative detection of SLNs, and does not require any specialized training. However, a further validation study is needed to evaluate its safety and feasibility in a large number of patients.
In summary, ICG-PB-based detection of SLNs permitted the real-time and intraoperative visualization of the lymphatic drainage pathway, from the areola towards the axilla. The combined use of ICG fluorescence with a visible dye is a highly sensitive and safe method for SLN identification, has a lower FNR, and does not involve exposure to radiation. This dual method is of increased clinical benefit in cases where no radiotracers are available.
Figures and Tables
Figure 1
Near-infrared fluorescence imaging during sentinel lymph node (SLN) mapping. (A) The periareolar injection site and afferent lymphatic duct are clearly observed. (B) A skin incision made at the point where the fluorescence disappeared, and a strong fluorescence is seen clearly after incision. (C) Lymphatic flow in the axilla is identified. (D) A resected SLN with fluorescence imaging reconfirmed by photodynamic eye.
References
1. Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006; 98:599–609.

2. Straver ME, Meijnen P, van Tienhoven G, van de Velde CJ, Mansel RE, Bogaerts J, et al. Sentinel node identification rate and nodal involvement in the EORTC 10981-22023 AMAROS trial. Ann Surg Oncol. 2010; 17:1854–1861.

3. Erb KM, Julian TB. Completion of axillary dissection for a positive sentinel node: necessary or not? Curr Oncol Rep. 2009; 11:15–20.

4. Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011; 305:569–575.

5. Julian TB, Krag D, Brown A, Anderson S, Harlow S, Ashikaga T, et al. Preliminary technical results of NSABP B-32, a randomized phase III clinical trial to compare sentinel node resection to conventional axillary dissection in clinical node negative breast cancer patients. Breast Cancer Res Treat. 2004; 88:Suppl. S511–S512.
6. Wang L, Yu JM, Wang YS, Zuo WS, Gao Y, Fan J, et al. Preoperative lymphoscintigraphy predicts the successful identification but is not necessary in sentinel lymph nodes biopsy in breast cancer. Ann Surg Oncol. 2007; 14:2215–2220.

7. Noguchi M, Inokuchi M, Zen Y. Complement of peritumoral and subareolar injection in breast cancer sentinel lymph node biopsy. J Surg Oncol. 2009; 100:100–105.

8. Teal CB, Slocum JP, Akin EA. Evaluation of the benefit of using blue dye in addition to radioisotope for sentinel lymph node biopsy in patients with breast cancer. Breast J. 2005; 11:391–393.

9. Sandrucci S, Casalegno PS, Percivale P, Mistrangelo M, Bombardieri E, Bertoglio S. Sentinel lymph node mapping and biopsy for breast cancer: a review of the literature relative to 4,791 procedures. Tumori. 1999; 85:425–434.

10. Stratmann SL, McCarty TM, Kuhn JA. Radiation safety with breast sentinel node biopsy. Am J Surg. 1999; 178:454–457.

11. Sardi A, Spiegler E, Colandrea J, Frishberg D, Sing H, Regan P, et al. The benefit of using two techniques for sentinel lymph node mapping in breast cancer. Am Surg. 2002; 68:24–28.
12. Ueno H, Hihara J, Shimizu K, Osaki A, Yamashita Y, Yoshida K, et al. Experimental study on fluorescent microspheres as a tracer for sentinel node detection. Anticancer Res. 2005; 25(2A):821–825.
13. Murawa D, Hirche C, Dresel S, Hünerbein M. Sentinel lymph node biopsy in breast cancer guided by indocyanine green fluorescence. Br J Surg. 2009; 96:1289–1294.

14. Doubrovsky A, De Wilt JH, Scolyer RA, McCarthy WH, Thompson JF. Sentinel node biopsy provides more accurate staging than elective lymph node dissection in patients with cutaneous melanoma. Ann Surg Oncol. 2004; 11:829–836.

15. Xing Y, Foy M, Cox DD, Kuerer HM, Hunt KK, Cormier JN. Meta-analysis of sentinel lymph node biopsy after preoperative chemotherapy in patients with breast cancer. Br J Surg. 2006; 93:539–546.

16. Derossis AM, Fey J, Yeung H, Yeh SD, Heerdt AS, Petrek J, et al. A trend analysis of the relative value of blue dye and isotope localization in 2,000 consecutive cases of sentinel node biopsy for breast cancer. J Am Coll Surg. 2001; 193:473–478.

17. McMasters KM, Wong SL, Martin RC 2nd, Chao C, Tuttle TM, Noyes RD, et al. Dermal injection of radioactive colloid is superior to peritumoral injection for breast cancer sentinel lymph node biopsy: results of a multiinstitutional study. Ann Surg. 2001; 233:676–687.

18. Hung WK, Chan CM, Ying M, Chong SF, Mak KL, Yip AW. Randomized clinical trial comparing blue dye with combined dye and isotope for sentinel lymph node biopsy in breast cancer. Br J Surg. 2005; 92:1494–1497.

19. Kang SW, Chung SE, Shin WJ, Lee JH. Polypoidal choroidal vasculopathy and late geographic hyperfluorescence on indocyanine green angiography. Br J Ophthalmol. 2009; 93:759–764.

21. Kitai T, Inomoto T, Miwa M, Shikayama T. Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer. 2005; 12:211–215.

22. Cox CE, Pendas S, Cox JM, Joseph E, Shons AR, Yeatman T, et al. Guidelines for sentinel node biopsy and lymphatic mapping of patients with breast cancer. Ann Surg. 1998; 227:645–651.

23. Hirche C, Murawa D, Mohr Z, Kneif S, Hünerbein M. ICG fluorescence-guided sentinel node biopsy for axillary nodal staging in breast cancer. Breast Cancer Res Treat. 2010; 121:373–378.

24. Hojo T, Nagao T, Kikuyama M, Akashi S, Kinoshita T. Evaluation of sentinel node biopsy by combined fluorescent and dye method and lymph flow for breast cancer. Breast. 2010; 19:210–213.

25. Cox CE, Kiluk JV, Riker AI, Cox JM, Allred N, Ramos DC, et al. Significance of sentinel lymph node micrometastases in human breast cancer. J Am Coll Surg. 2008; 206:261–268.

26. Christiansen P, Friis E, Balslev E, Jensen D, Møller S. Danish Breast Cancer Cooperative Group. Sentinel node biopsy in breast cancer: five years experience from Denmark. Acta Oncol. 2008; 47:561–568.

27. Bass SS, Cox CE, Reintgen DS. Learning curves and certification for breast cancer lymphatic mapping. Surg Oncol Clin N Am. 1999; 8:497–509.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download