Abstract
Purpose
The aim of this study was to investigate the clinical outcome of additional breast lesions identified with breast magnetic resonance imaging (MRI) in breast cancer patients.
Methods
A total of 153 patients who underwent breast MRI between July 2006 and March 2008 were retrospectively reviewed. Thirty-three patients (21.6&) were recommended for second-look ultrasound (US) for further characterization of additional lesions detected on breast MRI and these patients constituted our study population.
Results
Assessment for lesions detected on breast MRI consisted of the following: 25 benign lesions (73.5&), two indeterminate (5.9%), and seven malignant (20.6%) in 33 patients. Second-look US identified 12 additional lesions in 34 lesions (35.3%) and these lesions were confirmed by histological examination. Of the 12 lesions found in the 11 patients, six (50.0%) including one contralateral breast cancer were malignant. The surgical plan was altered in 18.2% (six of 33) of the patients. The use of breast MRI justified a change in treatment for four patients (66.7%) and caused two patients (33.3&) to undergo unwarranted additional surgical procedures.
Conclusion
Breast MRI identified additional multifocal or contralateral cancer which was not detected initially on conventional imaging in breast cancer patients. Breast MRI has become an indispensable modality in conjunction with conventional modalities for preoperative evaluation of patients with operable breast cancer.
Since surgical treatment of breast cancer is determined by several prognostic factors including tumor size, lymph node metastasis, and negative status of the resection margin, the value of breast magnetic resonance imaging (MRI) in breast cancer is increasing. The role of breast MRI covers every phases of breast cancer management such as early detection, preoperative planning, staging, monitoring neoadjuvant chemotherapy, and identifying recurrence [1-3]. Compared to other preoperative imaging modalities such as mammography and breast ultrasound (US), breast MRI has the highest sensitivity in breast cancer detection, ranging from 93% to 99%, and the ability to detect malignancy that is clinically or radiologically occult [4,5]. These advantages have resulted in the widespread use of breast MRI for other applications that include evaluation of tumor extent, identification of multifocality or multicentricity, screening for contralateral breast cancer, evaluation of the axillary lymph node, and determining the resection margin [2,4]. However, breast MRI as a preoperative diagnostic modality is associated with many limitations such as variable specificity (29% to 98%) and false positive rates, difficulty of percutaneous biopsy, high cost, and the possibility of over-treatment [6,7]. Several efforts have been made over the past few years in order to overcome these limits of breast MRI including introduction of multimodality scores of image interpretation, development of a MRI lexicon, and standardization of protocols and indications [8,9]. Despite of these attempts, specificity of breast MRI still remains lower than desired and is responsible for "decision dilemmas" in cases of abnormal lesions revealed by breast MRI that were not detected on other conventional imaging modalities. In particular, it is difficult to determine whether these lesions should be followed-up or biopsied. Recently, there were several reports that "second-look US" in the diagnostic work-up of MRI-detected breast lesions is useful [10,11]. It is also useful for breast cancer centers that are not equipped to perform breast MRI-guided biopsy [4].
The purpose of this study was to investigate the clinical outcome of additional lesions identified with breast MRI in breast cancer patients, and to evaluate the usefulness of breast MRI as a preoperative diagnostic modality.
A retrospective review was performed using the records of 161 consecutive breast cancer patients who underwent preoperative breast MRI between July 2006 and March 2008. Of these 161 patients, 7 patients who received neoadjuvant chemotherapy and a male breast cancer patient were excluded from the analysis. Breast MR images were acquired using a 1.5-T system (Siemens, Erlangen, Germany) and a dedicated CP breast array coil (Siemens). Gadobutrol (Bayer Schering Pharma, Berlin, Germany) was injected intravenously at a dose of 0.1 mmol/kg body weight at a flow rate of 1.5 mL/sec, followed by flushing with 20 mL of saline. The imaging sequence included a T2-weighted, fat suppression, turbo spin echo (TSE) sagittal image sequence followed by a T1-weighted, TSE sagittal image, T1 fast low angle shot (FLASH) 3D dynamic image. Section thickness was typically 2 mm with a 320×221 matrix and a 280-300 mm field of view. Subtraction images were obtained by subtracting the pre-contrast images from each of the five sets of post-contrast images, on a by pixel-by-pixel basis.
Breast MR images were interpreted by two experienced breast radiologists using the Breast Imaging Reporting and Data System (BI-RADS) MRI lexicon [12]. Lesions identified on breast MRI were described including morphology (shape, margin, and internal architecture), enhancement kinetics (enhancement rate, amount, and the shape of time/signal intensity curve), and signal intensity of the lesion on T2WI. Additional lesions detected on breast MRI were defined as follows: 1) located in a different quadrant, 2) separated by at least 1 cm of intervening normal-appearing tissue in the same quadrant, and 3) contiguous but extended at least 4 cm beyond the primary cancer in the same quadrant [13]. Depending on the degree of malignant suspicion of the lesion, it was classified as benign (BI-RADS Category 2 and 3), indeterminate (BI-RADS Category 4), and malignant (BI-RADS Category 5).
In cases of additional lesions detected on breast MRI, patients underwent second-look US. US with a 15-MHz linear-array transducer (Acuson Sequoia; Acuson, Mountain View, USA) was used for bilateral whole breast examination. If an additional lesion was identified by second-look US, US-guided core needle biopsy using a 14-guage spring-loaded automatic biopsy device (TSK Laboratory, Tochigi-ken, Japan) was taken in the same setting. Annual conventional imaging follow-up was used for lesions that were likely benign which were not detected by second-look US. Descriptive statistical techniques were used to evaluate frequency distribution. SPSS version 11.5 software package (SPSS Inc., Chicago, USA) was used for statistical analysis.
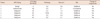
The clinicopathologic characteristics of 153 patients were shown in Table 1. Additional 34 lesions on breast MRI were found in 33 patients (21.6%) out of 153 patients. Lesions of 20 patients (60.6%) were included in definition 1 of breast MRI additional lesion, lesions of 8 patients (24.2%) were in definition 2, and lesions of 4 patients (12.1%) were in definition 3. One patient (3.1%) had 2 lesions of definition 2 and 3. Twenty-five lesions (73.5%) were assessed as benign lesions, two (5.9%) as indeterminate lesions, and seven (20.6%) as malignant lesions. Among 34 lesions, second-look US identified 12 lesions (35.3%): 6 (50.0%) lesions of definition 1, 4 (33.3%) lesions of definition 2, and 2 (16.7%) lesions of definition 3. Twenty-two patients (66.7%) who were not found to have correlated lesions by second-look US were recognized as having benign lesions based on breast MRI (Figure 1). Three of 25 benign lesions detected on second look US were assigned to two lesions of BI-RADS 3 and one lesion of BI-RADS 4A.
Twelve additional lesions were found in 11 patients; from the result of US-guided core needle biopsy, six lesions (50%) were malignant and the other six were benign (Table 2). Three of six malignant lesions were invasive ductal carcinoma (IDC), two lesions were invasive lobular carcinoma (ILC), and one lesion was ductal carcinoma in situ (DCIS) (Table 2). The size of the six malignant lesions ranged from 0.3 cm to 1.0 cm with a median size of 0.6 cm. One of the six malignant lesions was in the contralateral breast (Table 3). Representative breast lesion (patient number 6 in Table 3) identified with second-look US in patients with an additional breast lesion originally detected on MRI is shown in Figure 2. Consequently, surgical plan of this patient was changed to total mastectomy.
The surgical plan was changed for six out of the 33 patients (18.2%) who had additional lesions found on breast MRI. Among six patients confirmed to have malignant lesions by biopsy after second-look US, the surgical plan for four was changed to total mastectomy (three patients), and additional breast conserving surgery (BCS) (one patient). The other two patients among six patients with altered surgical plan were found to have benign lesions by biopsy, but additional local excision (LE) was performed in these individuals to treat contralateral lesions (Table 4). Therefore, change of surgical plan was an appropriate choice for four patients (66.7%), but not for two patients (33.3%).
There is still controversy concerning the usefulness of preoperative breast MRI in operable breast cancer patients because of false positive rates, cost, and possibility of over-treatment. Preoperative breast MRI may also increase patient anxiety through further test procedures, waiting for and receiving results, additional follow-up investigations such as biopsy, and treatment delays. However, in spite of these limitations, the diagnostic value of breast MRI as a preoperative evaluation modality is increasing. According to a study to examine usefulness of preoperative breast MRI, occult breast cancer which was not detected clinically or with conventional imaging was found by breast MRI in approximately 1% to 18% of the study patients [5]. Furthermore, other investigators reported that the sensitivity of breast MRI for detecting multicentric disease is up to 93%, and the sensitivity for detecting contralateral disease is up to 88% [4,14]. In addition, non-mass forming lesions, which are defined as duct dilatation with internal echoes, multivesicular pattern, and low echo area in the mammary gland on breast US, can be more specifically evaluated by breast MRI. Sotome et al. [15] reported that breast MRI is useful to find breast cancer if the possibility of malignancy of non-mass forming lesion identified by breast US cannot be excluded. Our study demonstrated that additional lesions on breast MRI were found in 33 (21.6%) out of 153 patients. Among these 33 patients, newly-identified additional breast cancer was found in six (3.9%); these results were similar to that of previous study [5].
Although the sensitivity of breast MRI is very high, some authors noted that the specificity is relatively limited [6,7]. This is because the specificity of breast MRI is affected by various factors such as the experience of the radiologist, the use of appropriate imaging techniques, and composition of the patient cohort [16]. Kuhl [1] also reported that for cases of DCIS, sensitivity and specificity of breast MRI are much lower than that for IDC. The mere detection of DCIS was limited due to the fact that enhancement is seen in only a fraction of DCIS cases, ranging from 70% to 80%. Therefore, the appropriate use of breast MRI for preoperative evaluation is currently one of the most debated issues in breast cancer treatment.
On the other hand, to reduce false positive rates, the findings of breast MRI are often correlated with findings from other breast imaging modalities. According to LaTrenta et al. [7], the likelihood of breast cancer was significantly higher among breast MRI-detected lesions with a US correlation (43%) than lesions without a US correlation (14%). Shin et al. [17] also reported that targeted US can play a useful role in the evaluation of additional suspicious lesions detected by breast MRI. In a study by Beran et al. [18], seventy-five additional suspicious lesions were detected by breast MRI in 52 out of 191 women. Targeted US identified 65 lesions (87%); consequently, targeted US may be a reliable method to confirm breast MRI abnormalities in breast cancer patients. In our result, 12 lesions of 34 lesions identified initially on breast MRI (35.3%) were detected by second-look US. This detection rate is higher than the rate (23%) reported by a previous study [7] but lower than rates (66-87%) reported by others [18,19]. During follow-up of 22 patients who were not found with lesion on second-look US, no additional lesions were detected on conventional imaging modalities until now.
Due to the high sensitivity of preoperative breast MRI, women may be screened for BCS eligibility and thus received more extensive surgical treatment (mastectomy or wider excision). Houssami and Hayes [5] performed a meta-analysis of 12 observational studies and reported that breast MRI changed surgical management, generally from BCS to more radical surgery, but found no evidence that breast MRI improved surgical treatment or outcomes. It was also reported that preoperative breast MRI does not significantly affect the overall rate of incomplete tumor excision but the mastectomy rate was increased due to the fact that the tumor extent was more widely evaluated with this technique than conventional imaging [6]. In contrast, Jin et al. [20] determined that among 154 patients who were evaluated by preoperative breast MRI, surgical plans of 14 patients were changed. Surgery for only three of the 14 patients (1.9%) was unnecessarily extended. Thus, these results suggested that additional multifocal or multicentric lesions could be diagnosed by preoperative breast MRI and influence surgical plans. Mann et al. [21] also reported that the re-excision rate of preoperative breast MRI group in invasive lobular carcinoma patients was remarkably lower than those who did not undergo preoperative MRI evaluation, and this difference is related to the decrease of the final mastectomy rate. Our study showed that the surgical plans were changed for six out of 33 patients (18.2%) in whom additional lesions were identified by breast MRI. Although surgery for two (33.3%) out of 6 patients was unnecessarily performed, it was an appropriate choice of treatment for four patients (66.7%). Therefore, we believe that breast MRI provides sufficient preoperative evaluation for breast cancer patients.
Fischer et al. [22] demonstrated that the recurrence rate and detection rate of contralateral cancer in the preoperative breast MRI group are lower than those of patients who did not undergo this evaluation. These results are due to the fact that breast MRI can diagnose breast cancer as accurately as US, correlate tumor histology through the pattern of time intensity, and identify the extent of intraductal spread more accurately than conventional imaging techniques [23]. The only evidence from a randomized trial regarding the impact of breast MRI on surgical planning comes from one randomized controlled trial that was designed to measure the effect of breast MRI on re-excision rates as its primary endpoint [24]. In this trial (Comparative Effectiveness of MRI in Breast Cancer, COMICE), 1,623 women scheduled for BCS were randomly assigned to preoperative evaluation with breast MRI or not. Re-excision rates were not statistically significant in women randomized to evaluation by conventional imaging (19.3%) or breast MRI in addition to conventional imaging (18.8%). Furthermore, there is no evidence that breast MRI improves surgical care or prognosis.
The current study has some important limitations, however, mostly stemming from a small number of patients and retrospective design. Additionally, we could not include the recurrence rate after surgery because of the short follow-up period. This is a considerable limitation of our study, so we recommend that additional randomized controlled trials with longer follow-up periods should be carried out.
In conclusion, preoperative breast MRI was effective in diagnosing additional multifocal or contralateral breast cancer which was not detected by conventional imaging techniques. Therefore, we find that breast MRI is a valuable preoperative diagnostic modality for operable breast cancer patients.
Figures and Tables
Figure 1
Assessment and pathologic results of additional lesions on magnetic resonance imaging (MRI). Additional 34 lesions on breast MRI were found in 33 patients. Twenty-two lesions which were assessed as benign lesion on breast MRI were not identified the additional lesions on second-look ultrasound (US). Twelve additional lesions in 11 patients have been diagnosed as follows.
*One patient has two malignant assessed lesions in each breast.

Figure 2
A 59-year-old woman with known right breast cancer (4-o'clock position) who underwent preoperative breast magnetic resonance imaging (MRI). (A) Subtraction axial MR image shows unexpected oval shaped enhancing lesion (arrow) at 3-o'clock position in the right breast. It was classified as malignant. (B) On second-look ultrasound, 0.7 cm sized, oval, ill defined, and hypoechoic lesion was found at the identical location. Sonographic findings suggest BI-RADS 4C and pathologic result was invasive ductal carcinoma.

References
2. Braun M, Pölcher M, Schrading S, Zivanovic O, Kowalski T, Flucke U, et al. Influence of preoperative MRI on the surgical management of patients with operable breast cancer. Breast Cancer Res Treat. 2008. 111:179–187.

3. Linda A, Zuiani C, Londero V, Bazzocchi M. Outcome of initially only magnetic resonance mammography-detected findings with and without correlate at second-look sonography: distribution according to patient history of breast cancer and lesion size. Breast. 2008. 17:51–57.

4. Wiratkapun C, Duke D, Nordmann AS, Lertsithichai P, Narra V, Barton PT, et al. Indeterminate or suspicious breast lesions detected initially with MR imaging: value of MRI-directed breast ultrasound. Acad Radiol. 2008. 15:618–625.

5. Houssami N, Hayes DF. Review of preoperative magnetic resonance imaging (MRI) in breast cancer: should MRI be performed on all women with newly diagnosed, early stage breast cancer? CA Cancer J Clin. 2009. 59:290–302.

6. Pengel KE, Loo CE, Teertstra HJ, Muller SH, Wesseling J, Peterse JL, et al. The impact of preoperative MRI on breast-conserving surgery of invasive cancer: a comparative cohort study. Breast Cancer Res Treat. 2009. 116:161–169.

7. LaTrenta LR, Menell JH, Morris EA, Abramson AF, Dershaw DD, Liberman L. Breast lesions detected with MR imaging: utility and histopathologic importance of identification with US. Radiology. 2003. 227:856–861.

8. Warren RM, Thompson D, Pointon LJ, Hoff R, Gilbert FJ, Padhani AR, et al. Evaluation of a prospective scoring system designed for a multicenter breast MR imaging screening study. Radiology. 2006. 239:677–685.

9. Schnall MD, Blume J, Bluemke DA, DeAngelis GA, DeBruhl N, Harms S, et al. Diagnostic architectural and dynamic features at breast MR imaging: multicenter study. Radiology. 2006. 238:42–53.

10. Abe H, Schmidt RA, Shah RN, Shimauchi A, Kulkarni K, Sennett CA, et al. MR-directed ("Second-Look") ultrasound examination for breast lesions detected initially on MRI: MR and sonographic findings. AJR Am J Roentgenol. 2010. 194:370–377.

11. Destounis S, Arieno A, Somerville PA, Seifert PJ, Murphy P, Morgan R, et al. Community-based practice experience of unsuspected breast magnetic resonance imaging abnormalities evaluated with second-look sonography. J Ultrasound Med. 2009. 28:1337–1346.

12. Tardivon AA, Athanasiou A, Thibault F, El Khoury C. Breast imaging and reporting data system (BIRADS): magnetic resonance imaging. Eur J Radiol. 2007. 61:212–215.

13. Liberman L, Morris EA, Dershaw DD, Abramson AF, Tan LK. MR imaging of the ipsilateral breast in women with percutaneously proven breast cancer. AJR Am J Roentgenol. 2003. 180:901–910.

14. Hollingsworth AB, Stough RG, O'Dell CA, Brekke CE. Breast magnetic resonance imaging for preoperative locoregional staging. Am J Surg. 2008. 196:389–397.

15. Sotome K, Yamamoto Y, Hirano A, Takahara T, Hasegawa S, Nakamaru M, et al. The role of contrast enhanced MRI in the diagnosis of non-mass image-forming lesions on breast ultrasonography. Breast Cancer. 2007. 14:371–380.

16. Mann RM, Kuhl CK, Kinkel K, Boetes C. Breast MRI: guidelines from the European Society of Breast Imaging. Eur Radiol. 2008. 18:1307–1318.

17. Shin JH, Han BK, Choe YH, Ko K, Choi N. Targeted ultrasound for MR-detected lesions in breast cancer patients. Korean J Radiol. 2007. 8:475–483.

18. Beran L, Liang W, Nims T, Paquelet J, Sickle-Santanello B. Correlation of targeted ultrasound with magnetic resonance imaging abnormalities of the breast. Am J Surg. 2005. 190:592–594.

19. Sim LS, Hendriks JH, Bult P, Fook-Chong SM. US correlation for MRI-detected breast lesions in women with familial risk of breast cancer. Clin Radiol. 2005. 60:801–806.

20. Jin JW, Yom CK, Koo MY, Moon BI, Choi KJ, Choi HY. The role and significance of preoperative breast MRI in the setting of breast cancer. J Breast Cancer. 2008. 11:146–150.

21. Mann RM, Loo CE, Wobbes T, Bult P, Barentsz JO, Gilhuijs KG, et al. The impact of preoperative breast MRI on the re-excision rate in invasive lobular carcinoma of the breast. Breast Cancer Res Treat. 2010. 119:415–422.

22. Fischer U, Zachariae O, Baum F, von Heyden D, Funke M, Liersch T. The influence of preoperative MRI of the breasts on recurrence rate in patients with breast cancer. Eur Radiol. 2004. 14:1725–1731.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download