Abstract
PURPOSE
This study evaluated the influence of abutment materials on the stability of the implant-abutment joint in internal conical connection type implant systems.
MATERIALS AND METHODS
Internal conical connection type implants, cement-retained abutments, and tungsten carbide-coated abutment screws were used. The abutments were fabricated with commercially pure grade 3 titanium (group T3), commercially pure grade 4 titanium (group T4), or Ti-6Al-4V (group TA) (n=5, each). In order to assess the amount of settlement after abutment fixation, a 30-Ncm tightening torque was applied, then the change in length before and after tightening the abutment screw was measured, and the preload exerted was recorded. The compressive bending strength was measured under the ISO14801 conditions. In order to determine whether there were significant changes in settlement, preload, and compressive bending strength before and after abutment fixation depending on abutment materials, one-way ANOVA and Tukey's HSD post-hoc test was performed.
RESULTS
Group TA exhibited the smallest mean change in the combined length of the implant and abutment before and after fixation, and no difference was observed between groups T3 and T4 (P>.05). Group TA exhibited the highest preload and compressive bending strength values, followed by T4, then T3 (P<.001).
CONCLUSION
The abutment material can influence the stability of the interface in internal conical connection type implant systems. The strength of the abutment material was inversely correlated with settlement, and positively correlated with compressive bending strength. Preload was inversely proportional to the frictional coefficient of the abutment material.
Endosseous dental implant is one of the methods for restoring partially1,2 or completely3,4 edentulous patients. The treatment has a high success rate, and is now common.5,6,7 Most implant systems are composed of an endosseous fixture and a prosthesis-supporting abutment, and each component is connected with a screw.8 During mastication, the interface between the prosthesis and implant abutment is subjected to various physiological loads. Should the magnitude of such loads exceed the safety limits of the interface area, failure due to the loosening of the interface configuration or fatigue fractures can occur.9,10,11 Factors affecting the stability of the interface include external loads,12,13 the preload of the abutment screw,14 and the implant-abutment connection type.14,15,16,17,18
In order to enhance the stability of the implant-abutment interface, external loads imposed on the screw-retained interface should be minimized, and the preload should be maximized.19 In order to reduce the external loads borne by implant-abutment interface, the implant should be located correctly and the prosthesis should be designed to minimize the length of lever. Further, occlusion should be designed such that the loads are transferred along the implant axis in order to prevent an excessive concentration of stress at implant-abutment joint.20,21,22
Abutment screws become elongated owing to torque during tightening, and compressive force is generated between the implant and abutment because of the elastic recovery of the screw. The tensile force thus generated within the screw is called preload.14 As the stability of the implant-abutment interface increases with the increase in magnitude of preload, the maximum possible elongation of the abutment screw within the range of its elastic recovery should be utilized in order to increase the preload.23 Martin et al.24 reported that the higher the tightening torque, the higher the magnitude of preload, and Simon25 have suggested that tightening torque should exceed 30 Ncm to reduce loosening of the screw. When a screw is tightened, 90% of the initial tightening torque is directed toward overcoming frictional force and only the remaining 10% is converted into preload.26 Frictional force occurs between the screw and fixture, the screw head and abutment, and the abutment end and fixture,24 and if the frictional force between these structures is reduced more force can be converted into preload.14 In attempts to reduce the frictional coefficient of the abutment screw, different screw materials have been investigated14,27 as has coating the surface of the screw.14,28 In their study on the influence of screw material and shape on preload, Jörnéus et al.27 reported that flat-headed gold alloy screws showed the highest preload magnitude, and Park et al.28 reported that coating the abutment screw reduced the frictional coefficient, thus increasing the preload.
The implant-abutment interface can be broadly divided into internal conical connection and external hex connection types.29 In the internal conical connection type implant systems, the tightening torque is manifested through the elongation of abutment screws, and also through the taper-lock effect owing to settlement of the conical abutment. The majority of functional loading is transferred along a tapered interface, resulting in a limited load on the abutment screw. Thus, internal conical connection type implants have been reported to have better screw joint stability than the external hex connection type.29,30,31
While several studies have investigated preload, screw loosening, fracture,14,15,16,17,18 abutment screw materials,14,27 and surface coating14,28 with a view to enhancing the stability of the implant-abutment interface, the influence of abutment materials on the stability of the implant-abutment interface has not yet been sufficiently studied. In this study, we measured and compared settlement, preload, and compressive bending strength before and after abutment fixation in order to investigate the influence of abutment materials on the stability of the interface in internal conical connection type implant systems.
In this study, internal conical connection type fixtures (GSII, Ø4.0 × H11.0 mm, Osstem Co., Seoul, Korea), cement-retained abutments (GSTA5610, Ø5.0 × H5.5 mm, Osstem Co., Seoul, Korea), and tungsten carbide-coated (CW/C) abutment screws were used (Fig. 1). Five uniformly sized abutments for each group were fabricated with commercially pure grade 3 titanium (group T3), commercially pure grade 4 titanium (group T4), or Ti-6Al-4V (group TA). A total of 15 sets of fixture, abutment, and abutment screw were used in the experiment, and the materials for the implant components are listed in Table 1.
In order to determine the amount of settlement of different abutment materials when tightening torque is applied, the length of each abutment screw was measured before and after tightening. Since it is difficult to define the baseline value prior to the application of tightening torque, the abutment was placed on the fixture by applying 5 Ncm tightening torque to the abutment screw with a digital torque gauge (MGT12E, MARK-10 Corp., New York, NY, USA) and the length from the upper top of the abutment to the bottom end of the fixture was measured. Then, an additional tightening torque of 30 Ncm was applied, followed by re-measuring of the implant length and subsequent calculation of the difference between the 2 measurements (Fig. 2). This process was repeated 5 times for each specimen using a 1-µm precision micrometer (Mitutoyo Corp., Kanagawa, Japan).
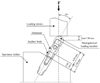
Measurement of the preload of an abutment screw must be preceded by measurement of the tensile force of the screw, or the compressive force between the abutment and the implant. In this study, the compressive force between the abutment and the implant was measured by the SlimLine force sensor (9132B21, Kistler Instrument Corp., Novi, MI, USA). If the sensor is placed directly between the abutment and the implant, the difference in screw-tightening length and the morphological change in the interface can lead to errors. To prevent this, the implant body model was made using the same material and internal structure to the GSII implant system. The model was made up of the upper and lower parts, and the sensor was placed between them (Fig. 3). The preload was measured while tightening the abutment screw at a tightening torque of 30 Ncm with a digital torque gauge (MGT12E, MARK-10 Corp., New York, NY, USA).
A fixture-implant specimen fastened using a tightening torque of 30 Ncm was fixed to a universal testing machine (Instron8841, Instron Corp., Mass, Norwood, MA, USA) under the test condition of marginal bone resorption of 3 mm as specified in the dental implant test standards (ISO14801). A cylindrical metal tube constituting to the superstructure of the prosthesis was fabricated, with a hemispheric upper end. After cementing the metal tube to the abutment with temporary resin cement (Premier Implant Cement, Premier Dental Product Company, Plymouth Meeting, PA, USA), an inclined load was applied at a loading angle of 30° (ISO14801) at a speed of 1 mm/min (Fig. 4). The maximum load was measured right before the implant and abutment complex was irreversibly bent.
One-way ANOVA using SPSS (Release 12.0, SPSS Inc., Chicago, IL, USA) was performed in order to assess the significance of changes in implant length, preload, and compressive bending strength in relation to abutment materials, which was then verified with Tukey's honestly significant difference (HSD) post-hoc test.
Table 2 outlines the mean values of settlement, preload, and compressive bending strength measured after abutment fixation. Group TA showed the smallest mean values of settlement, and no differences were observed between groups T3 and T4 (P>.05, Fig. 5). Group TA exhibited the highest preload values, followed by T4 and T3 (Fig. 6), demonstrating significant intergroup differences (P<.001, Fig. 7).
To improve the joint stability of the implant-abutment interface, a higher preload should be produced during screw tightening and preserved when functional load is applied to the prosthesis.32 When tightening torque is applied to the screw or a functional load is applied to the prosthesis, the phenomenon of settlement takes place at the initial contact point, provided that the loading exceeds the yield strength. Once the initial contact surface is flattened as a result of morphological changes, affecting the micro surface roughness and shortening the distance between abutment and fixture, the settlement of the abutment leads to shortening the abutment screw and loss of preload.33 Lee and Lee34 reported that the effect of different abutment materials on abutment settling in the conical connection implant system. In their study, there was no significant difference between abutment materials. In present study, however, group TA showed significantly less settlement (P<.05). Since the abutments used in our experiment are all TiN-coated to improve the esthetic color appeal of the peri-implant mucosa35 and to reinforce the surface hardness and abrasion resistance,36,37 the frictional coefficient, surface hardness, and abrasion resistance were expected to be similar among all experimental groups. The abutment materials tested were, in increasing order of strength,38 commercially pure grade 3 titanium (group T3), commercially pure grade 4 titanium (group T4), and Ti-6Al-4V (group TA). In the limitations of this study, the amount of abutment settlement under tightening torque is influenced more by the material that the abutments are comprised of than their surface coatings. The phenomenon of settlement occurs not only under tightening torque, but also under functional loading. Therefore, using abutments comprised of high-strength materials may diminish preload losses (i.e., screw loosening) caused by abutment settlement under functional loads and reduce changes in occlusion.33
The preload generates a compressive force between the implant and abutment and resists external loads. External loads imposed on a screw joint cause fine slipping between screw threads, resulting in screw length reduction and thus partial preload loss. If the preload loss progresses to the point that it falls below the threshold value, external loads or vibratory energy trigger the rotation of screw threads, leading to screw loosening.39 Therefore, a higher preload confers proportionally higher resistance against screw loosening and fatigue fracture, due to the reduced potential of external load-induced joint separation.14,23 Increasing the preload involves the frictional force as well as the tightening torque of the screw, and there are studies reporting that higher preloads were obtained by reducing the frictional coefficients of abutment screws14,27,28 as in the case of the tungsten carbide-coated screws used in our study. Yet, as well as the frictional force occurring between the abutment and fixture, that occurring between the abutment and screw,24 and the materials that the abutment is comprised of, can be important determinants of the magnitude of preload. Corazza et al.40 reported that the carbon film coating of abutment surface reduced abutment screw loosening. In their study, the carbon film coating improved hardness, adaptation at the implant-abutment interface and scratch resistance, and reduced the friction coefficient of the abutment-screw head interface. In present study, group TA showed the highest preload followed by groups T4 and T3 (P<.001). All three groups were subjected to the same conditions, and all of the abutment screws were coated with tungsten carbide; thus, the difference in the materials that the abutments were comprised of is thought to have been responsible for the differences in the frictional force generated between the screw and abutment observed between the groups. As the frictional coefficient of Ti-6Al-4V is smaller than that of commercially pure titanium,41 that the highest preload was exhibited by group TA may be attributable to the smaller frictional force generated between the screw and abutment as compared to the other 2 groups, which contributed to an increase in the tightening torque used for elongation of the abutment screw.
The compressive bending strength of the implant-abutment interface was highest in the TA group, and lowest in the T3 group, and all groups differed significantly from each other (P<.001). Since the strength of the abutment material used in group TA, which exhibited significantly higher preload values (P<.001), was higher than that of groups T3 and T4, the differences in compressive bending strength evidently resulted from the differences in abutment material strength and preload. However, given that in the real-life oral situation loads are not static, rather fatigue is caused by repetitive dynamic loads, further studies are necessary.
The results of this study suggest that the abutment material plays an important role in the interface stability of implants of the internal conical connection type. Provided that biological risks can be excluded, it would be recommendable to use abutment materials with high strength and low frictional coefficients to improve the mechanical stability of the implant-abutment interface.
Figures and Tables
Fig. 1
The GSII implant system used in this study. (A) GS II implant assembly, (B) Fixture, (C) Abutment, (D) Abutment screw.
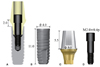
Fig. 2
Measurement of settlement. (A) Before tightening torque application, (B) After tightening torque application.

Fig. 3
Schematic diagram of the preload measuring apparatus. The "a" means implant-abutment interface and "b" means implant-screw interface. (A) Implant assembly, (B) Implant body model.
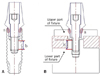
Table 1
Features of the implant-abutment systems

| Group | Abutment materials | Abutment surface | Fixture | Abutment screw |
|---|---|---|---|---|
| T3 | CP-Ti grade 3 | TiN coating | CP-Ti grade 4 | Titanium alloy WC/C coating |
| T4 | CP-Ti grade 4 | |||
| TA | Titanium alloy |
References
1. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981; 10:387–416.
2. Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990; 5:347–359.
3. van Steenberghe D, Lekholm U, Bolender C, Folmer T, Henry P, Herrmann I, Higuchi K, Laney W, Linden U, Astrand P. Applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: a prospective multicenter study on 558 fixtures. Int J Oral Maxillofac Implants. 1990; 5:272–281.
4. Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clin Oral Implants Res. 1996; 7:329–336.
5. Eckert SE, Wollan PC. Retrospective review of 1170 endosseous implants placed in partially edentulous jaws. J Prosthet Dent. 1998; 79:415–421.
6. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part I: Surgical results. J Prosthet Dent. 1990; 63:451–457.
7. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: Problems and complications encountered. J Prosthet Dent. 1990; 64:185–194.
8. Steinebrunner L, Wolfart S, Ludwig K, Kern M. Implantabutment interface design affects fatigue and fracture strength of implants. Clin Oral Implants Res. 2008; 19:1276–1284.
9. Rangert B, Jemt T, Jörneus L. Forces and moments on Branemark implants. Int J Oral Maxillofac Implants. 1989; 4:241–247.
10. Burguete RL, Johns RB, King T, Patterson EA. Tightening characteristics for screwed joints in osseointegrated dental implants. J Prosthet Dent. 1994; 71:592–599.
11. Haack JE, Sakaguchi RL, Sun T, Coffey JP. Elongation and preload stress in dental implant abutment screws. Int J Oral Maxillofac Implants. 1995; 10:529–536.
12. Rangert B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants. 1995; 10:326–334.
13. Taylor TD. Prosthodontic problems and limitations associated with osseointegration. J Prosthet Dent. 1998; 79:74–78.
14. Khraisat A, Abu-Hammad O, Al-Kayed AM, Dar-Odeh N. Stability of the implant/abutment joint in a single-tooth external-hexagon implant system: clinical and mechanical review. Clin Implant Dent Relat Res. 2004; 6:222–229.
15. Kitagawa T, Tanimoto Y, Odaki M, Nemoto K, Aida M. Influence of implant/abutment joint designs on abutment screw loosening in a dental implant system. J Biomed Mater Res B Appl Biomater. 2005; 75:457–463.
16. Tsuge T, Hagiwara Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J. 2009; 28:373–381.
17. Khayat PG, Hallage PG, Toledo RA. An investigation of 131 consecutively placed wide screw-vent implants. Int J Oral Maxillofac Implants. 2001; 16:827–832.
18. Balfour A, O'Brien GR. Comparative study of antirotational single tooth abutments. J Prosthet Dent. 1995; 73:36–43.
19. Smedberg JI, Nilner K, Rangert B, Svensson SA, Glantz SA. On the influence of superstructure connection on implant preload: a methodological and clinical study. Clin Oral Implants Res. 1996; 7:55–63.
20. Rangert BR, Sullivan RM, Jemt TM. Load factor control for implants in the posterior partially edentulous segment. Int J Oral Maxillofac Implants. 1997; 12:360–370.
21. English CE. Biomechanical concerns with fixed partial dentures involving implants. Implant Dent. 1993; 2:221–242.
22. Weinberg LA. Reduction of implant loading with therapeutic biomechanics. Implant Dent. 1998; 7:277–285.
23. McGlumphy EA, Mendel DA, Holloway JA. Implant screw mechanics. Dent Clin North Am. 1998; 42:71–89.
24. Martin WC, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J Prosthet Dent. 2001; 86:24–32.
25. Simon RL. Single implant-supported molar and premolar crowns: a ten-year retrospective clinical report. J Prosthet Dent. 2003; 90:517–521.
26. Motosh N. Development of design charts for bolts preloaded up to the plastic range. J Manuf Sci Eng. 1976; 98:849–851.
27. Jörnéus L, Jemt T, Carlsson L. Loads and designs of screw joints for single crowns supported by osseointegrated implants. Int J Oral Maxillofac Implants. 1992; 7:353–359.
28. Park JK, Choi JU, Jeon YC, Choi KS, Jeong CM. Effects of abutment screw coating on implant preload. J Prosthodont. 2010; 19:458–464.
29. Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000; 15:519–526.
30. Norton MR. An in vitro evaluation of the strength of an internal conical interface compared to a butt joint interface in implant design. Clin Oral Implants Res. 1997; 8:290–298.
31. Hansson S. Implant-abutment interface: biomechanical study of flat top versus conical. Clin Implant Dent Relat Res. 2000; 2:33–41.
32. Theoharidou A, Petridis HP, Tzannas K, Garefis P. Abutment screw loosening in single-implant restorations: a systematic review. Int J Oral Maxillofac Implants. 2008; 23:681–690.
33. Winkler S, Ring K, Ring JD, Boberick KG. Implant screw mechanics and the settling effect: overview. J Oral Implantol. 2003; 29:242–245.
34. Lee JS, Lee JS. Effect of various abutment systems on the removal torque and the abutment settling in the conical connection implant systems. J Korean Acad Prosthodont. 2012; 50:92–98.
35. Bressan E, Paniz G, Lops D, Corazza B, Romeo E, Favero G. Influence of abutment material on the gingival color of implant-supported all-ceramic restorations: a prospective multicenter study. Clin Oral Implants Res. 2011; 22:631–637.
36. Tamura Y, Yokoyama A, Watari F, Kawasaki T. Surface properties and biocompatibility of nitrided titanium for abrasion resistant implant materials. Dent Mater J. 2002; 21:355–372.
37. Mengel R, Meer C, Flores-de-Jacoby L. The treatment of uncoated and titanium nitride-coated abutments with different instruments. Int J Oral Maxillofac Implants. 2004; 19:232–238.
38. Niinomi M. Mechanical properties of biomedical titanium alloys. Mater Sci Eng A. 1998; 243:231–236.
39. Bickford J. An Introduction to the design and behavior of bolted Joints. 3rd ed. New York: Marcel Dekker;1995.
40. Corazza PH, de Moura Silva A, Cavalcanti Queiroz JR, Salazar Marocho SM, Bottino MA, Massi M, de Assunção e Souza RO. Carbon film coating of abutment surfaces: effect on the abutment screw removal torque. Implant Dent. 2014; 23:434–438.
41. Budinski KG. Tribological properties of titanium alloys. Wear. 1991; 151:203–217.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download