Abstract
Background
The risk of tuberculosis (TB) infection among health care workers (HCWs) is higher than as noted among workers in the general population. The prevalence and risk factors of TB infection among HCWs were assessed in a tertiary hospital in South Korea, resulting in a conclusion of an intermediate TB burden within the country.
Methods
This cross-sectional study enrolled HCWs who underwent a QuantiFERON-TB Gold In-Tube (QFT-GIT) test to detect the presence of a latent TB infection (LTBI), in patients admitted to a tertiary hospital in South Korea in 2017. The departments of the hospital were divided into TB-related and TB-unrelated departments, which were based on the risk of exposure to TB patients. In this sense, the risk factors for LTBI, including current working in the TB-related departments, were analyzed.
Results
In this case, a total of 499 HCWs (54 doctors, 365 nurses and 80 paramedical personnel) were enrolled in this study. The median age of the subjects was 31 years (range, 20–67 years), 428 (85.8%) were female, and 208 (41.7%) were working in the TB-related departments. The prevalence of LTBI was 15.8% based on the QFT-GIT. Additionally, the prevalence of experience of exposure to pre-treatment TB patents was higher among HCWs working in the TB-related departments, than among HCWs working in the TB-unrelated departments (78.8% vs. 61.9%, p<0.001). However, there was no significant difference in the prevalence of LTBI between the two groups (17.3% vs. 14.8%, p=0.458). On a review of the multivariate analysis, only the factor of age was independently associated with an increased risk of LTBI (p=0.006).
Compared to general population, health care workers (HCWs) are at increased risk of tuberculosis (TB) infection through occupational exposure to TB patients12. Considering that about 5%–15% of TB infected people are at risk for developing TB during their lifetime3, HCWs with latent TB infection (LTBI) are potential risk group for TB leading to transmission of Mycobacterium tuberculosis to other HCWs and patients. Therefore, LTBI screening and treatment for HCWs is an important component of TB infection control measures in the hospitals4.
In hospitals, many HCWs from different occupations are working in various departments. And, studies conducted in South Korea have reported varying prevalence of LTBI among HCWs from 17% to 37%567. Therefore, it is important to find out who is at high risk for TB infection in order to determine the priority of LTBI screening and treatment.
Because the risk of TB infection depends on the proximity and duration of exposure to infectious TB patients, HCWs working in the respiratory medicine, emergency department, medical intensive care unit, pulmonary function test and bronchoscopy unit and laboratory processing suspected or confirmed M. tuberculosis specimens are known to be at high risk of TB infection4689. Thus, the Korea Centers for Disease Control and Prevention (KCDC) recommended that HCWs working in the departments with increased risk of TB infection (TB-related departments) receive annual screening for LTBI10.
Recently, interferon-gamma release assay like QuantiFERON-TB Gold In-Tube (QFT-GIT) is widely used for the diagnosis of LTBI because it has several advantages over the tuberculin skin test (TST) such as higher specificity without cross-reactivity with bacillus Calmette-Guérin strains or environmental mycobacteria11. And, several studies targeting HCWs have suggested that a positive QFT-GIT result is a better indicator of LTBI than a positive TST result612.
To date, the risk factors of TB infection of HCWs using QFT-GIT have not been thoroughly evaluated in South Korea, an intermediate TB burden country with the annual notification rate of new TB cases as 60.4 per 100,000 population in 201610. Therefore, analyzing the prevalence and various risk factors of TB infection of HCWs, including current working in the TB-related departments, is important for determining the priority for LTBI screening and treatment in South Korea.
This study assessed the prevalence and the risk factors for LTBI, including current working in the TB-related departments, among HCWs working in a tertiary referral hospital in South Korea.
This cross-sectional study was conducted from June 2017 to December 2017 in a 700-bed tertiary referral hospital in South Korea. Approximately 350 TB patients are treated at the hospital annually. Of the 540 HCWs involved in the patient care, 515 underwent QFT-GIT test according to the national LTBI screening program, excluding 25 HCWs who had history of TB treatment or were positive for previous LTBI test (TST or interferon-γ release assay). They also underwent chest radiography to exclude active TB. Of the 515 HCWs who underwent QFT-GIT test, 499 agreed to participate in the study. A questionnaire was administered to each participant to collect demographic data and known risk factors of TB infection; occupation (doctor, nurse, paramedical personnel), specific departments in which they work, duration of employment as a HCW, experience of exposure to pre-treatment TB patients both inside and outside the hospital. The departments of the hospital were divided into TB-related and TB-unrelated departments according to KCDC recommendation10. TB-related departments include outpatient and inpatient departments of respiratory medicine and infection, outpatient department of pediatric respiratory medicine, pulmonary function test and bronchoscopy unit, emergency department, medical intensive care unit, chest section of radiology department, microbiology section of laboratory. TB-unrelated departments include outpatient and inpatient departments of internal medicine and pediatrics not included in the TB-related departments, obstetrics, and gynecology, etc. The study protocol was approved by the Institutional Review Board of the Dankook University Hospital (2017-06-015) and written informed consents were provided by all participants.
QFT-GIT was used for the diagnosis of LTBI in this study. QFT-GIT test was performed according to the manufacturer's recommendations (Qiagen Ltd., Carnegie, VIC, Australia). The blood samples were mixed with M. tuberculosis specific antigens (early secreted antigenic target-6, culture filtrate protein 10, and TB 7.7), mitogen phytohemagglutinin (positive control) and saline (negative control) and incubated for 16–24 hours. The detection and quantification of interferon-gamma by enzyme-linked immunosorbent assay was used to measure in vitro responses to TB antigens. All values were interpreted after subtracting the value of the negative control. The QFT-GIT test results were interpreted as positive if the interferon-γ level in response to TB antigen ≥0.35 IU/mL and >25% of Nil value.
Data are expressed as a number (%) or median (range or interquartile range). All statistical analyses were performed using the SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). Comparison between HCWs working in the TB-related and TB-unrelated departments were analyzed using the chi-square test for categorical variables. Continuous variables were analyzed using Mann-Whitney U test. Risk factors for LTBI were evaluated using logistic regression analysis. Independent variables for multivariate analysis were selected on the basis of their statistical significance in univariate analysis and clinical significance. A two-tailed p-value of <0.05 was considered to be statistically significant.
Of the 499 participants, 428 (85.8%) were female and the median age was 31.0 years (range, 20–67 years). The median length of employment as a HCW was 7.0 years (range, 1–38 years). The occupations of the HCWs includes 54 doctors (10.8%), 365 nurses (73.1%), and 80 paramedical personnel (16.0%) (radiology and laboratory technicians, nursing assistants, etc.). All were human immunodeficiency virus test negative. Nine (1.8%) were medicated with diabetes mellitus, and 18 (3.6%) were current smoker. Of the 499 participants, the prevalence of LTBI based on QFT-GIT positivity was 15.8%. There were no radiologically active TB patients among the participants.
Clinical characteristics of 291 HCWs working in the TB-unrelated departments and 208 HCWs working in the TB-related departments are shown in Table 1. The median age of HCWs working in the TB-unrelated and related departments was 32.0 years (range, 20–64 years) and 30.0 years (range, 20–67 years), respectively. The median length of work as a HCW in the TB-unrelated and related departments was 7.0 years (range, 1–38 years) and 6.0 years (range, 1–35 years), respectively. There were no differences between the two groups in age (Figure 1), duration of work as HCWs (Figure 2), and sex. But, prevalence of experience of exposure to pre-treatment TB patients was higher in HCWs working in the TB-related departments than HCWs working in the TB-unrelated departments (78.8% vs. 61.9%, p<0.001). More doctors were included in the TB-unrelated departments and more paramedical personnel were included in the TB-related departments. The prevalence of LTBI among HCWs working in the TB-related departments was higher than that of HCWs working in the TB-unrelated departments, but it was not statistically significant (17.3% vs. 14.8%, p=0.458).
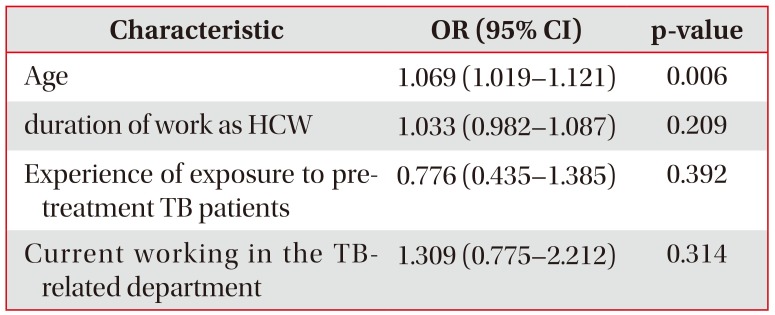
On univariate logistic regression analysis, age (odds ratio [OR], 1.094; 95% confidence interval [CI], 1.064–1.124) and duration of work as HCW (OR, 1.096; 95% CI, 1.065–1.128) were significantly associated with increased risk of LTBI (Table 2). Other known risk factors such as current working in the TB-related departments, occupation, experience of exposure to pre-treatment TB patients were not associated with increased risk of LTBI. Multivariate analysis showed that only age was independently associated with increased risk of LTBI (OR, 1.069; 95% CI, 1.019–1.121) (Table 3).
LTBI treatment is known to be one of the important strategies to prevent the development of TB and block the transmission of M. tuberculosis to other people. However, since the benefit of LTBI treatment is not prominent compared to the cost for screening and treatment for LTBI, LTBI screening and treatment is generally recommended for people whose benefit outweighs the cost13. It is therefore important to determine who is at high risk for TB infection in order to select the target groups for LTBI screening and treatment.
In general, HCWs working in the TB-related departments are known to be at high risk for TB infection48. Thus, the KCDC recommended that HCWs who are working in the TB-related departments receive annual screening for LTBI10. As expected, this study showed that experience of exposure to pre-treatment TB patients were more frequent in HCWs working in the TB-related departments than HCWs working in the TB-unrelated departments (78.8% vs. 61.9%). Considering that TB patients have the highest infectivity before treatment, this finding suggests that HCWs working in the TB-related departments are at higher risk of TB infection than those working in the TB-unrelated departments.
This study showed that the prevalence of LTBI among HCWs working in the TB-related departments was higher than that of HCWs working in the TB-unrelated departments, but unexpectedly it was not statistically significant (17.3% vs. 14.8%, p=0.458). Possible explanations for this unexpected result are as follows. In large hospitals, HCWs may work in several departments in rotation. And, HCW might have moved from TB-unrelated department to TB-related department recently. Considering that it takes about 8 weeks for QFT-GIT conversion after exposure to infectious TB patients, QFT-GIT may give false-negative result if it is conducted during the window period14. Considering the high prevalence of TB in South Korea, it seems that out-hospital exposure to TB patients also diluted the difference between the two groups10. In a multicenter study conducted in South Korea also showed that current working in the TB-related departments was not associated with positive QFT-GIT result. However, HCWs with experience of working in the TB-related departments was independently associated with positive QFT-GIT result6. Another study conducted at a tertiary hospital in South Korea showed that the positive rate QFT-GIT was higher among HCWs who had frequent direct contact with TB patients in the TB-related departments than those who had no history of direct contact with TB patient in the TB-unrelated departments15. Another study conducted in military hospitals of South Korea also showed that the risk of LTBI was higher in HCWs who took care of TB patients for one year or more16. These findings suggest that longer duration of work in the TB-related departments is better risk factor of LTBI than the current working in the TB-related departments in South Korea.
The transmission of TB in the hospital is also affected by the efficiency of TB infection control measures. In resource-limited countries, HCWs are at increased risk of exposure to TB patients within the hospitals due to lack of isolation rooms and inadequate TB infection control measures. In these settings, LTBI among HCWs was consistently associated with markers of occupational exposure to TB patients such as working in TB clinic, long duration of employment as HCW1718. However, in resource-rich countries, the risk of TB infection among HCWs becomes closer to general population because transmission of TB in the hospitals is reduced or prevented by implementation of effective TB infection control measures1. In a study conducted in the United States, a resource-rich country, showed that non-occupational factors such as old age and foreign birth account for most of TB infections arising among HCWs19. In most tertiary hospitals in South Korea, including the hospital included in this study, patients diagnosed or suspected of having TB are admitted to isolation rooms equipped with negative pressure ventilation until they are no longer infectious. And HCWs and visitors entering such rooms are required to wear N95 respirators. In the present study, known risk factors for TB infection such as current working in the TB-related departments, experience of exposure to pre-treatment TB patients were not associated with increased risk of LTBI among HCWs. These findings suggest that TB infection control measures employed by the hospital of this study have mitigated the transmission of TB in the hospital2021. In a study conducted in Taiwan, an intermediate TB burden country like South Korea, also showed that experience of unprotected exposure to TB patients was not associated with increased risk of LTBI among HCWs11.
Compared to young HCWs, older HCWs are more likely to be exposed to TB patients during their life either within the hospital or in the community. It is not surprising, therefore, that several studies, including this study, have shown that old age was significantly associated with increased risk of LTBI among HCWs622.
It is generally known that there is a correlation between LTBI prevalence among HCWs and regional TB prevalence because high prevalence of TB in the community increases the risk of TB infection of HCWs both inside and outside of the hospital23. Therefore, national TB control programs to reduce the incidence of TB in the community also reduce the risk of TB infection for HCWs. The South Korean government has implemented various TB control programs, including LTBI screening and treatment for HCWs, to reduce the incidence of TB, and it has been steadily declining in recent years10. The results of this study can be used as a useful data for the government of South Korea to establish LTBI screening and treatment programs for HCWs.
The purpose of conducting LTBI screening and treatment for HCWs is to block the spread of TB by preventing infected persons from progressing to active TB. However, currently available diagnostic tests for LTBI have several limitations; variable specificity, cannot distinguish between LTBI and active TB, do not predict who will progress to active TB, controversies on the conversion from negative to positive result24. Thus LTBI screening and treatment should be targeted to HCWs at high risk for LTBI and progression to active TB. However, it is not well known who is at increased risk of developing active TB among LTBI positive HCWs. Therefore, further study is needed on the risk factors for predicting who will develop active TB among LTBI positive HCWs.
The limitation of this study is that participants of this study did not undergo LTBI screening before starting work at the hospital. Therefore, it is not possible to exclude the possibility that a QFT-GIT positive HCW has already been infected with M. tuberculosis before starting work at the hospital. And since this study was conducted only in a single tertiary hospital, it is difficult to say that the people who participated in this study represent the HCWs of South Korea in general. Therefore, in order to better understand the pattern and risk factors of LTBI of HCWs in South Korea, multi-center prospective studies are needed for HCWs who are LTBI test negative when they start working at the hospital1525.
Acknowledgments
The author gratefully acknowledges Professor Kwon Ho-Jang of department of preventive medicine of Dankook University College of Medicine for his assistance with the statistics used in this paper.
References
1. Menzies D, Joshi R, Pai M. Risk of tuberculosis infection and disease associated with work in health care settings. Int J Tuberc Lung Dis. 2007; 11:593–605. PMID: 17519089.
2. Joshi R, Narang U, Zwerling A, Jain D, Jain V, Kalantri S, et al. Predictive value of latent tuberculosis tests in Indian healthcare workers: a cohort study. Eur Respir J. 2011; 38:1475–1477. PMID: 22130764.

3. Marks GB, Bai J, Simpson SE, Sullivan EA, Stewart GJ. Incidence of tuberculosis among a cohort of tuberculin-positive refugees in Australia: reappraising the estimates of risk. Am J Respir Crit Care Med. 2000; 162:1851–1854. PMID: 11069825.
4. Jensen PA, Lambert LA, Iademarco MF, Ridzon R. CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005; 54:1–141.
5. Lee KJ, Kang YA, Kim YM, Cho SN, Moon JW, Park MS, et al. Screening for latent tuberculosis infection in South Korean healthcare workers using a tuberculin skin test and whole blood interferon-gamma assay. Scand J Infect Dis. 2010; 42:672–678. PMID: 20482459.
6. Jo KW, Hong Y, Park JS, Bae IG, Eom JS, Lee SR, et al. Prevalence of latent tuberculosis infection among health care workers in South Korea: a multicenter study. Tuberc Respir Dis. 2013; 75:18–24.

7. Park HY, Jeon K, Suh GY, Kwon OJ, Chung DR, Yoonchang SW, et al. Interferon-gamma release assay for tuberculosis screening of healthcare workers at a Korean tertiary hospital. Scand J Infect Dis. 2010; 42:943–945. PMID: 20936910.
8. Jo KW, Woo JH, Hong Y, Choi CM, Oh YM, Lee SD, et al. Incidence of tuberculosis among health care workers at a private university hospital in South Korea. Int J Tuberc Lung Dis. 2008; 12:436–440. PMID: 18371271.
9. Moon HW, Kim H, Hur M, Yun YM, Lee A. Latent tuberculosis infection screening for laboratory personnel using interferon-gamma release assay and tuberculin skin test in Korea: an intermediate incidence setting. J Clin Lab Anal. 2011; 25:382–388. PMID: 22086790.
10. Korea Centers for Disease Control and Prevention. National TB elimination project [Internet]. Cheongju: Korea Centers for Disease Control and Prevention;2017. cited 2018 Feb 25. Available from: http://www.cdc.go.kr/CDC/eng/contents/CdcEngContentView.jsp?cid=74227&menuIds=HOME002-MNU0576-MNU0582.
11. Hung WT, Lee SS, Sy CL, Wu KS, Chen JK, Tsai HC, et al. Prevalence of latent tuberculosis infection in BCG-vaccinated healthcare workers by using an interferon-gamma release assay and the tuberculin skin test in an intermediate tuberculosis burden country. J Microbiol Immunol Infect. 2015; 48:147–152. PMID: 24071516.

12. Pai M, Zwerling A, Menzies D. Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann Intern Med. 2008; 149:177–184. PMID: 18593687.

13. Zammarchi L, Casadei G, Strohmeyer M, Bartalesi F, Liendo C, Matteelli A, et al. A scoping review of cost-effectiveness of screening and treatment for latent tubercolosis infection in migrants from high-incidence countries. BMC Health Serv Res. 2015; 15:412. PMID: 26399233.

14. Lee SH. Diagnosis and treatment of latent tuberculosis infection. Tuberc Respir Dis. 2015; 78:56–63.

15. Kim SY, Park MS, Kim YS, Kim SK, Chang J, Kang YA. Conversion rates of an interferon-gamma release assay and the tuberculin skin test in the serial monitoring of healthcare workers. Infection. 2013; 41:511–516. PMID: 23104257.
16. Yoon CG, Oh SY, Lee JB, Kim MH, Seo Y, Yang J, et al. Occupational risk of latent tuberculosis infection in health workers of 14 military hospitals. J Korean Med Sci. 2017; 32:1251–1257. PMID: 28665059.

17. Mirtskhulava V, Kempker R, Shields KL, Leonard MK, Tsertsvadze T, del Rio C, et al. Prevalence and risk factors for latent tuberculosis infection among health care workers in Georgia. Int J Tuberc Lung Dis. 2008; 12:513–519. PMID: 18419886.
18. Drobniewski F, Balabanova Y, Zakamova E, Nikolayevskyy V, Fedorin I. Rates of latent tuberculosis in health care staff in Russia. PLoS Med. 2007; 4:e55. PMID: 17298167.

19. Lambert LA, Pratt RH, Armstrong LR, Haddad MB. Tuberculosis among healthcare workers, United States, 1995-2007. Infect Control Hosp Epidemiol. 2012; 33:1126–1132. PMID: 23041811.

20. Lee JY. Tuberculosis infection control in health-care facilities: environmental control and personal protection. Tuberc Respir Dis. 2016; 79:234–240.

21. Jo KW. Preventing the transmission of tuberculosis in health care settings: administrative control. Tuberc Respir Dis. 2017; 80:21–26.

22. Kwon Y, Kim SJ, Kim J, Kim SY, Song EM, Lee EJ, et al. Results of tuberculosis contact investigation in congregate settings in Korea, 2013. Osong Public Health Res Perspect. 2014; 5(Suppl):S30–S36. PMID: 25861578.

23. Belo C, Naidoo S. Prevalence and risk factors for latent tuberculosis infection among healthcare workers in Nampula Central Hospital, Mozambique. BMC Infect Dis. 2017; 17:408. PMID: 28595594.

24. Herrera V, Perry S, Parsonnet J, Banaei N. Clinical application and limitations of interferon-gamma release assays for the diagnosis of latent tuberculosis infection. Clin Infect Dis. 2011; 52:1031–1037. PMID: 21460320.
25. Lee K, Han MK, Choi HR, Choi CM, Oh YM, Lee SD, et al. Annual incidence of latent tuberculosis infection among newly employed nurses at a tertiary care university hospital. Infect Control Hosp Epidemiol. 2009; 30:1218–1222. PMID: 19848602.

Figure 1
QuantiFERON-TB Gold In-Tube (QTF-GIT) positive rate according to age. There was no difference in the QFT-GIT positive rate between tuberculosis (TB)-related and TB-unrelated departments in each age group.
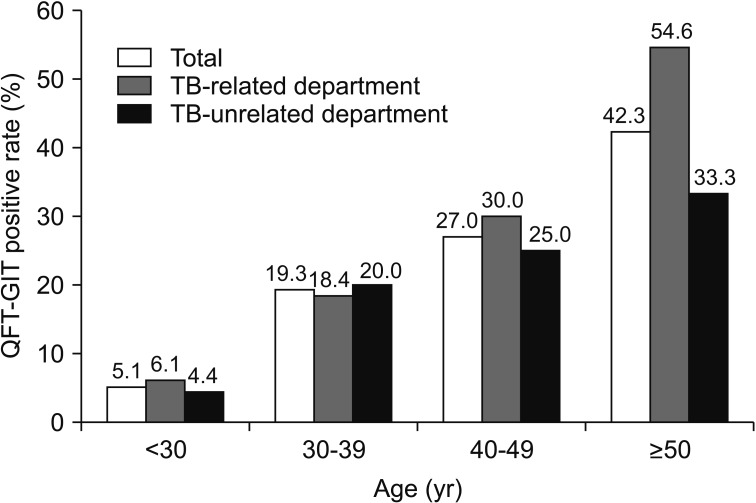
Figure 2
QuantiFERON-TB Gold In-Tube (QFT-GIT) positive rate according to duration of work as health care worker (HCW). There was no difference in the QFT-GIT positive rate between the tuberculosis (TB)-related and TB-unrelated departments in each duration of work as a HCW group.
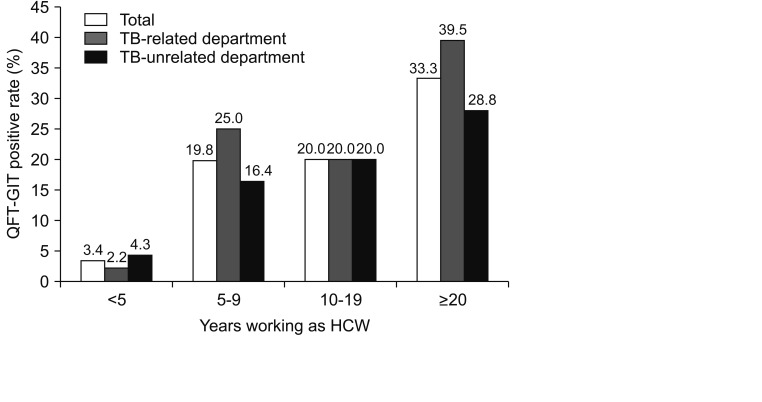
Table 1
Clinical characteristics and QunatiFERON-TB Gold In-Tube results of participants
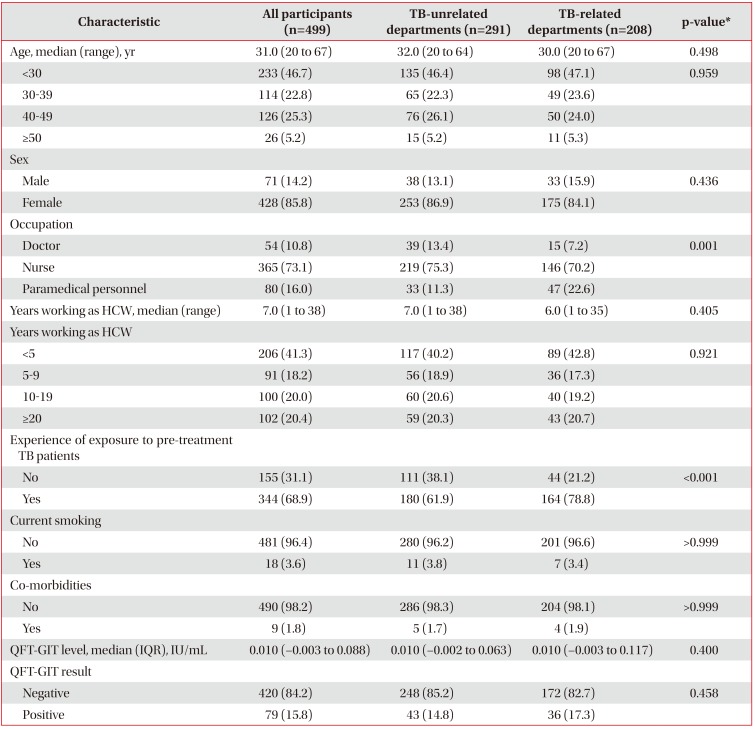
Table 2
Univariate logistic regression analysis of risk factors for latent TB infection among HCWs
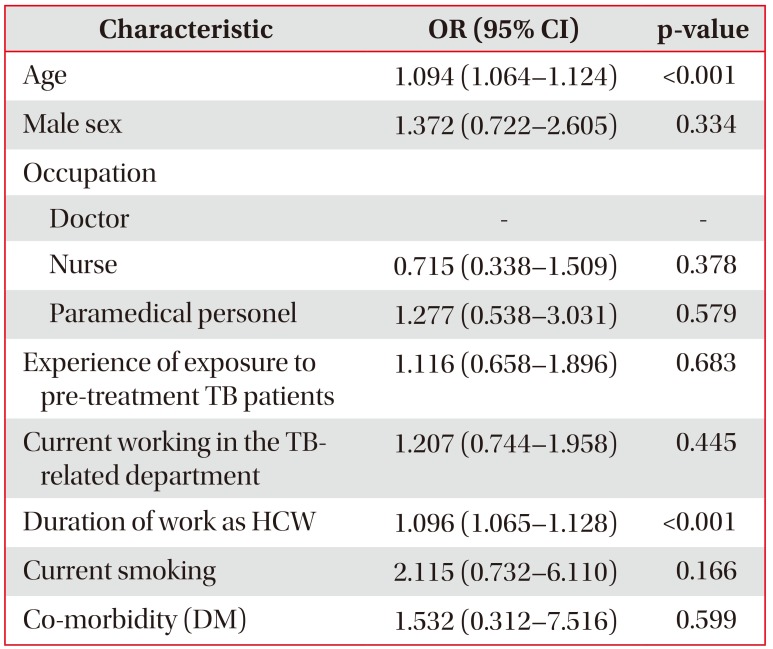
Table 3
Multivariate logistic regression analysis of risk factors for latent TB infection among HCWs




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download