Abstract
The drug reaction with eosinophilia and systemic symptom (DRESS) syndrome is a severe adverse drug-induced reaction which includes a severe skin eruption, fever, hematologic abnormalities (eosinophilia or atypical lymphocytes) and internal organ involvement. The most frequently reported drug was anticonvulsants. The diagnosis of DRESS syndrome is challenging because the pattern of cutaneous eruption and the types of organs involved are various. The treatments for DRESS syndrome are culprit drug withdrawal and corticosteroids. Here we report a 71-year-old man with skin eruption with eosinophilia and hepatic and renal involvement that appeared 4 weeks after he had taken anti-tuberculosis drugs (isoniazid, ethambutol, rifampicin, and pyrazinamide), and resolved after stopping anti-tuberculosis drugs and the administration of systemic corticosteroids. DRESS recurred after re-challenging isoniazid, we identified isoniazid was causative drug.
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a rare, potentially life-threatening, drug-induced hypersensitivity reaction that includes skin eruption, hematologic abnormalities (eosinophilia, atypical lymphocytes), lymphadenopathy, and internal organ involvement (liver, kidney, lung, and etc.)1,2. DRESS syndrome is characterized by a long latency (2 to 8 weeks) between drug exposure and disease onset, a prolonged course with frequent relapses despite the discontinuation of the culprit drug, and frequent association with the reactivation of a latent human herpes virus (HHV) infection2. The pathogenesis of DRESS syndrome is partially understood. Different mechanisms have been implicated in its development, including detoxification defects leading to reactive metabolite formation and subsequent immunological reactions3, slow acetylation and reactivation of human herpes, including Epstein-Barr virus and HHV-6 and -74,5,6. Identification and prompt withdrawal of the offending drug is the mainstay of treatment for patients with DRESS syndrome.
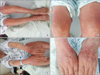
A 71-year-old man visited our hospital because of skin eruption. He had no other remarkable allergy history. But he had taken anti-tuberculosis drugs without other drugs for 2 months because of tuberculous meningitis. His anti-tuberculosis drugs were composed of isoniazid (INH) 300 mg, rifampicin (RFP) 450 mg, ethambutol (EMB) 800 mg, and pyrazinamide (PZA) 1,000 mg. On physical examination, generalized skin eruption was shown in whole body and his skin was exfoliated but not itching (Figure 1). Blood pressure was 120/80 mm Hg, the pulse 90 beats per minute, the oral temperature 36.7℃, the respiratory rate 20 breaths per minute, and the oxygen saturation 95.1%, pH 7.39, and PaO2 74.5 mm Hg, PaCO2 32.2 mm Hg while the patient was breathing ambient air. Laboratory examinations showed a hemoglobin concentration of 14.0 g/dL, a leukocyte count of 6,540/mm3 (neutrophils 46.8%, lymphocytes 21.9%, monocytes 20.9%, and eosinophils 9.8%), an aspartate aminotransferase level of 90 IU/L, an alkaline aminotransferase level of 74 IU/L, an alkaline phosphatase level of 46 IU/L, lactic dehydrogenase 607 IU/L, a total protein 5.2 g/dL, albumin level of 3.0 g/dL, a total bilirubin level of 1.7 mg/dL, a glucose level of 86 mg/dL, blood urea nitrogen 21.5 mg/dL, creatinine 1.4 mg/dL, and a C-reactive protein level of 10.99 mg/dL. An electrocardiogram revealed normal sinus rhythm. Active consolidative lesion nor mass were not detected on chest radiographs. But, computed tomography of the chest identified extensive centri- and paraseptal emphysematous change on both lungs, especially on both upper lobes. After admission, we discontinued all anti-tuberculosis drugs and started corticosteroid therapy. His skin lesion was gradually resolved over 3 weeks (Figure 2). Because we worried about that his tuberculous meningitis got worse if all anti-tuberculosis drugs were interrupted for a long time, restarted anti-tuberculosis drugs on RFP 150 mg at first dose and increased the dose of RFP. At that time his skin lesion did not reappear. And then his skin lesion on whole body reappeared following INH 100 mg for 3 days (Figure 3). So we diagnosed DRESS syndrome after re-challenging INH, anti-tuberculosis drug. We discontinued challenging drug, INH, and prescribed systemic corticosteroids (intravenous methylprednisolone 2 mg/kg/day for 5 days, tapered over 2 weeks). Eventually he fully recovered after stopping INH and administration of systemic corticosteroids. He have taken secondary anti-tuberculosis drugs (RFP and streptomycin, and moxifloxacin) and followed up for 3 months without any other complication.
DRESS syndrome is a rather distinct severe adverse drug reaction characterized by skin rash, fever, lymph node enlargement and internal organ involvement, which starts within 8 weeks after the initiation of the therapy7. The death rate is about 10%, mostly due to liver damage thought to be mediated by infiltration of eosinophils8,9,10,11.
The diagnosis of DRESS syndrome should be highly suspected with the presence of skin rash, liver involvement, fever, eosinophilia, and lymphadenopathy2. The treatment of DRESS syndrome is the prompt withdrawal of causative drug and prescription of systemic corticosteroids as standard of care. But efficacy of systemic corticosteroids is uncertain12. Therefore further studies are needed to recommend specific treatment guidelines.
Most patients with DRESS syndrome recover completely in weeks to months after causative drug withdrawal2. The prevalence of sequelae following DRESS syndrome is unknown. Improving the management of DRESS syndrome is closely linked to better knowledge of its pathogenesis, including identification of the culprit drugs and viral reactivation. The drug re-challenging test is generally accepted as the gold standard for confirming the culprit drug, and minimizes anti-tuberculosis treatment interruption13. DRESS syndrome has been initially described as the anticonvulsant hypersensitivity syndrome3. Anticonvulsants including carbamazepine, lamotrigine, and phenobarbital accounted for one third of the drugs causing DRESS syndrome3. In contrast, the vast majority of the other drugs were only associated with one case of DRESS syndrome. Recently some cases of DRESS syndrome associated with first- or second-line anti-tuberculosis drug were reported. But in most cases of them, causative drug of DRESS syndrome was determined based on medication history and subjective clinical decisions. A culprit drug was identified by drug re-challenging test in only a handful of cases12,13,14. RFP was most common offending drug associated DRESS syndrome. However, most of anti-tuberculosis drugs could be associated with DRESS syndrome12. As treatment of DRESS syndrome caused by anti-tuberculosis drug, all anti-tuberculosis drug was stopped with or without systemic corticosteroids in other reported cases. Symptoms and laboratory abnormalities gradually resolved over 2-4 weeks.
Here, we report a rare case of DRESS syndrome caused by INH. We identified that INH was a causative drug through the drug re-challenge. But unlike INH and RFP, the drug rechallenge of PZA and EMB was not done in this case. So we are not sure if PZA and EMB are causative drugs of DRESS syndrome or not. This point is a limitation of our case. INH is commonly use as component of first-line anti-tuberculosis regimen. Clinicians who prescribe anti-tuberculosis drugs must be aware of this severe hypersensitivity reaction to anti-tuberculosis drugs.
Figures and Tables
Figure 1
Generalized skin eruption and exfoliation showed in whole body on the first day of admission. Leg (A), thigh (B), arm (C), and hand (D).
References
1. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996; 15:250–257.
2. Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: a literature review. Am J Med. 2011; 124:588–597.
3. Shear NH, Spielberg SP. Anticonvulsant hypersensitivity syndrome: in vitro assessment of risk. J Clin Invest. 1988; 82:1826–1832.
4. Descamps V, Valance A, Edlinger C, Fillet AM, Grossin M, Lebrun-Vignes B, et al. Association of human herpesvirus 6 infection with drug reaction with eosinophilia and systemic symptoms. Arch Dermatol. 2001; 137:301–304.
5. Ichiche M, Kiesch N, De Bels D. DRESS syndrome associated with HHV-6 reactivation. Eur J Intern Med. 2003; 14:498–500.
6. Picard D, Janela B, Descamps V, D'Incan M, Courville P, Jacquot S, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): a multiorgan antiviral T cell response. Sci Transl Med. 2010; 2:46ra62.
7. Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update. Dermatology. 2003; 206:353–356.
8. Tas S, Simonart T. Drug rash with eosinophilia and systemic symptoms (DRESS syndrome). Acta Clin Belg. 1999; 54:197–200.
9. Roujeau JC. Treatment of severe drug eruptions. J Dermatol. 1999; 26:718–722.
10. Callot V, Roujeau JC, Bagot M, Wechsler J, Chosidow O, Souteyrand P, et al. Drug-induced pseudolymphoma and hypersensitivity syndrome. Two different clinical entities. Arch Dermatol. 1996; 132:1315–1321.
11. Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994; 331:1272–1285.
12. Palmero D, Castagnino J, Musella RM, Mosca C, Gonzalez Montaner P, de Casado GC. Difficult clinical management of anti-tuberculosis DRESS syndrome. Int J Tuberc Lung Dis. 2013; 17:76–78.
13. Kim JH, Jang SH, Kim DH, Park S, Kim DG, Jung KS. A case of DRESS syndrome induced by the antituberculosis drugs, prothionamide, and para-aminosalycilic acid. Ann Allergy Asthma Immunol. 2013; 110:118–119.
14. Rodríguez R, Jover V, Orozco I, Domenech J. DRESS syndrome in a 19-year-old patient following the administration of first-line antituberculosis drugs. J Investig Allergol Clin Immunol. 2012; 22:380–381.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download