Abstract
Here, we report a case of pulmonary paragonimiasis that was improved with initial anti-tuberculosis (TB) therapy but confused with reactivated pulmonary TB. A 53-year-old Chinese female presented with a persistent productive cough with foul smelling phlegm and blood streaked sputum. Radiologic findings showed subpleural cavitary consolidation in the right upper lobe (RUL). Bronchoscopic and cytological examination showed no remarkable medical feature. She was diagnosed with smear-negative TB, and her radiologic findings improved after receiving a 6-month anti-TB therapy. The chest CT scans, however, obtained at 4 months after completion of anti-TB therapy showed a newly developed subpleural consolidation in the RUL. She refused pathologic confirmation and was re-treated with anti-TB medication. Nevertheless, her chest CT scans revealed newly developed cavitary nodules at 5 months after re-treatment. She underwent thoracoscopic wedge resection; the pathological examination reported that granuloma caused by Paragonimus westermani. Paragonimiasis should also be considered in patients assessed with smear-negative pulmonary TB.
Paragonimiasis is a foodborne parasitic disease common in Southeast Asia, especially in Japan, Korea, the Philippines, Taiwan, and parts of China1. Infection results from ingestion of raw, inadequately cooked, or pickled crustaceans (crabs or crayfish), which are intermediate hosts for the organism during its transition from the cercarial to metacercarial larval stages1. It mainly presents as pleural effusion, intrapulmonary nodules, and pneumothorax with respiratory symptoms2. Patients with paragonimiasis reveal a wide variety of radiographic and computed tomography (CT) findings, including pulmonary noules or masses, and sometimes they are suspected to have a lung malignancy3. As the clinical and radiological features of pulmonary paragonimiasis are similar to those of pulmonary tuberculosis (TB) and lung cancer, some patients with paragonimiasis are initially diagnosed as having lung cancer or smear-negative TB. We report a case of pulmonary paragonimiasis that was improved with initial anti-TB therapy and confused with reactivated pulmonary TB.
A 53-year-old Chinese female presented with a persistent productive cough with foul smelling phlegm and blood streaked sputum of several months.' This was not associated with significant weight loss or fever. She was in good general health, and physical examination showed no unremarkable results. The patient's temperature was normal, her respiratory rate was 16 breaths per minute, her blood pressure was 134/74 mm Hg, and her pulse was 64 beats per minute. Right upper lung crackles were noted. Her total white blood cell count was 4,700/mm3, with 2.9% eosinophilia, and the high-sensitivity C-reactive protein level was 0.03 mg/dL. A tuberculin skin test (TST) was 16 mm and QuantiFERON-TB (QFT-G; Cellestis Ltd., Carnegie, Australia) test was also positive.
The chest radiograph carried out on presentation showed small nodular opacity in the suprahilar region of right upper lobe (Figure 1). Chest CT scans revealed focal parenchymal mass-like consolidation with cavitation and ground glass opacity in posterior segment of right upper lobe (Figure 2A, C), and pleural thickening in right lower lobe. Bronchoscopy revealed bronchial stenosis with hemorrhage that was associated with mucosal edema of the posterior segmental bronchus of the right upper lobe. Two samples of acid-fast bacilli (AFB) stain and one of polymerase chain reaction for Mycobacterium tuberculosis were negative. Cytological examination of the bronchial washing fluid showed no significant result. Although the patient had taken several courses of antibiotics, there were no clinical and radiological improvement observed. Though the microbiologic results were negative, the case showed radiological signs consistent with TB, and no response with antibiotics trial, and therefore smear-negative TB had been diagnosed based on algorithms4. The patient was started on anti-TB therapy. After receiving 6 months of anti-TB therapy, her chest radiograph with CT scans proved improvement with remnant mass-like consolidation on posterior segment of right upper lobe (Figure 2B, D). Purulent phlegm and hemoptysis, however, lasted intermittently during and after treatment.
Follow-up chest radiograph obtained at 4-months after completion of anti-TB therapy, showed newly developed mass-like consolidation on right upper lobe (Figure 3A, D). Bronchoscopy with bronchoalveolar lavage (BAL) was performed and sent for examinations. Results of cytology, AFB stain, and polymerase chain reaction for Mycobacterium tuberculosis were negative, as were cultures for bacteria, fungi, and mycobacteria. We could not observe eggs in sputum, or BAL fluid. Bronchoscopic biopsy showed chronic inflammation with a giant cell. According to complete blood cell count finding of the patient follow-up, there was no signal of peripheral blood eosinophilia. Therefore, we recommended pathologic confirmation with thoracoscopic examination, however the patient refused it. She was re-treated with anti-TB medication, and made transient aggravation at 2 months, and subsequent improvement at 3 months after re-treatment (Figure 3B, E). Although we considered the possibility of the paradoxical response with anti-TB treatment, the patient suffered recurrent hemoptysis and her chest CT scans revealed newly developed cavitary nodules within right upper lobe at 5 months after re-treatment (Figure 3C, F). She underwent thoracoscopic pulmonary wedge resection because the lesion was not appropriate for conducting percutaneous needle aspiration or biopsy. Thoracoscopic pulmonary wedge resection was applied for the mass measuring approximately 2×2-cm size in the posterior segment of right upper lung, and the gross findings of transected specimen on operative field showed a movable parasitic worm measured about 1×0.5 cm in cavitary lesion to be surrounded with organized and yellowish pulmonary parenchymal tissue. The pathological examination reported no malignant findings in the lung, and granuloma, acute and chronic inflammatory cell infiltration with eosinophils caused by Paragonimus westermani was diagnosed (Figure 4). Enzyme-linked immunosorbent assay (ELISA) antibody was positive for anibodies against P. westermani. A subsequent discussion with the patient revealed that she had eaten raw fresh water crabs several times before immigration to Korea from China several years ago. Anti-tuberculous medication was discontinued and praziquantel 75 mg/kg/day in three divided doses for 2 days were given. She was discharged with improvement of symptoms and signs. After that event, her symptoms and radiologic findings have maintained within normal range during 1-year follow-up period.
Paragonimiasis is a food-borne parasitic disease caused by the trematode P. westermani, which is endemic in East Asia (such as Japan, Korea, China, and Indochina)3. Infection in humans occurs by ingestion of raw or incompletely cooked freshwater crab or crayfish infected with lung fluke metacercaria5. The classic symptoms of pulmonary paragonimiasis include a chronic cough with rusty-brown sputum, hemoptysis, pleurisy, and fever with radiographic findings of patchy density, linear infiltration, nodules, pleural effusion, and pulmonary cavities5,6. As these clinical manifestations are similar to those of TB or lung malignancy, many paragonimiasis patients are initially treated for other diseases by confusion. According to retrospective study by Jeon et al.6, based on the initial clinical and radiologic findings, the correct initial diagnosis of pulmonary paragonimiasis was made in only 8%, and presumptive diagnoses were made of other pulmonary diseases, including pulmonary TB (30%), lung cancer (28%), pleural TB (14%), bronchiectasis (11%), pulmonary infiltration with eosinophilia syndrome (6%), or chronic bronchitis (3%).
Common radiologic findings of pleuropulmonary paragonimiasis included pleural effusion, hydropneumothorax, pulmonary nodules, or air-space consolidation, and cysts3. In the previous reports, the most common manifestation observed was pleural lesions7. According to the reports of one hospital in Korea, however, pleural lesions were relatively rare (28%), and the frequency of intrapulmonary parenchymal lesions was high (72%) compared to the reports of previous studies5,6,7. A report by Kim et al.7 suggested that the main features of chest CT scans of pleuropulmonary paragonimiasis were pulmonary nodules, including multiple nodules. Since these clinical manifestations and the radiological appearance of paragonimiasis are similar to those of TB or lung malignancy, the diagnosis is often confused, leading to improper and inadequate treatment3,5,8,9,10,11. In the present case, the lesion of mass-like consolidation with cavitation in the upper lobe led us to consider the findings as reactivated pulmonary TB. Kim et al.7 emphasized that although minimal and easily overlooked, focal fibrotic pleural or fissural thickening opacities (presumably worm migration tracks) adjacent to a pulmonary nodule could be an important clue in the diagnosis of pleuropulmonary paragonimiasis on CT scans. The patient in our case had also migrating peripheral nodules with subfissural linear opacity.
Until recently, distinguishing between pulmonary paragonimiasis and pulmonary TB has frequently proven to be quite difficult, and constitutes a diagnostic dilemma in areas in which TB and paragonimiasis coexist. Several studies revealed that 50%-70% of their patients with pulmonary paragonimiasis initially received a diagnosis of TB and were receiving anti-TB therapy2,6,9,12. In this case, empiric TB therapy was started after she failed to respond to several courses of antibiotics. This is based on the fact that TB is a common cause of hemoptysis and unresolved pneumonia in Asia. Smear-negative TB is currently defined as symptomatic illness in a patient with at least two sputum smear examinations negative for AFB on different occasions in whom pulmonary TB is later confirmed by other investigations including radiological features4. In this patient showed radiological improvement after first anti-TB treatment, and there was no evidence that she had other diagnosis other than pulmonary TB. In spite of the fact TST is of limited value in diagnosing pulmonary TB in populations with either a high prevalence of TB or a policy of Bacillus Calmette-Guérin (BCG) immunization at an early age4, she showed positive results in both TST and interferon γ release assay (QuantiFERON-TB test). However, another diagnosis was suspected when the new lesion was appeared after completion of her anti-TB therapy and aggravated during re-treatment. Her diagnosis was concluded using thoracoscopic wedge resection.
Peripheral blood examinations show leukocytosis and eosinophilia in many patients with pulmonary paragonimiasis5. Especially, eosinophilia may serve as an important parameter leading to the suspicion of paragonimiasis in the differential diagnosis because of its relatively high sensitivity5,7. Our patient, however, didn't have serum and sputum eosinophilia. The ELISA test, an immunoserologic test for Paragonimus-specific IgG antibody is highly sensitive and specific for P. westermani antibodies13. Unfortunately, due to the rarity of this disease and its protean clinical presentation, serologic testing may only be ordered as a confirmatory test in retrospect after the organisms are identified on pathologic evaluation of biopsy tissue, as in our case. Jeon et al.6 reported that sputum cytology examinations for the detection of eggs were performed in 72% and Paragonimus eggs were detected in the sputum of 46%, however, in our patients, no ova in the sputum or BAL fluid was detected. Although few reports of the bronchoscopic findings of pulmonary paragonimiasis exist, bronchial stenosis with mucosal changes including edematous swelling and mucosal nodularity is the most common bronchoscopic finding of pulmonary paragonimiasis, and Paragonimus eggs on cytologic examination of bronchial washing fluid was detected in more patients with endobronchial lesions on bronchoscopy14. We performed bronchoscopy twice and her bronchial mucosa showed a thickened, swollen, edematous appearance with hemorrhage in the right upper lobar bronchus however, there was no parasites or eggs from BAL fluid. In addition, bronchial mucosal biopsy specimens showed only chronic inflammation without evidence of eosinophilic infiltration nor ova. Considering fissural thickening opacity adjacent to a nodular lesion on CT scans and the presence of a positive dietary history, in combination with ELISA test for paragonimiasis, surgical lung biopsy itself was unnecessary for the diagnosis or treatment of pulmonary paragonimiasis in our patient.
In this report, we present a case of paragonimiasis belatedly identified as a parasitic migration to another site of the same lobe after an initial misdiagnosis of reactivated pulmonary TB with paradoxical response. Although it was not completely disappeared, the cavitary nodular lesion was grew slightly during initial anti-TB medications, that might lead to delayed diagnosis. Human infection of Paragonimus occurs with the ingestion of crustaceans infected with metacercariae. Upon infection, the metacercariae excysts in the duodenum and pass to the peritoneal cavity, then into the pleural cavity via the diaphragm. In the lung, it becomes encapsulated and develops into adult worms9. Because of this life history of P. westermani, our patient might seem to be improved with anti-TB medication. In the stage of 'migrating larvae' or 'mature worms', the size and densities are subject to change, growing small or enlarging or even to disappear completely and also may reappear, depending upon the degree of pericystic reaction1. Thereafter in the stage of 'recovery', the infesting parasites would sooner or later die either spontaneously or following treatment1. In our patient, considering the fact that sequelae like linear and minimal nodular lesion which remained after first treatment in chest CT scans still remained, it is considered that the lesion improved after the anti-TB medication was not resected. Nevertheless, the lesion was still maintained as same state in 1-year follow-up CT scans and there were no findings of exacerbation. Most papers have mentioned cure rates of around 90%-100% and even untreated, the prognosis with paragonimiasis is good15. The recent series, however, have reported some treatment failure after an initial set praziquantel medication and cure rate of only 75.0% after the first set of praziquantel and pleural drainage15. Our patient suffered surgical resection and succeeding treatment with praziquantel, and she had not shown any symptom or interval aggravation of chest radiograph and CT scans during 1-year follow-up period after the treatment.
In summary, this patient presented with symptomatically persistent and recurrent pulmonary paragonimiasis. It may be possible that ova could not be detected in sputum including BAL fluid, and biopsy specimen because adult flukes could not form worm cysts and lay ova in the lung, depending on the stages. The presence of a positive dietary history, negative TB cultures and lack of response to anti-TB therapy should prompt a revision of diagnosis, as in this case. Especially in endemic regions with a high prevalence of food-borne parasitic diseases and TB, paragonimiasis should be also considered in the patient initially assessed with smear-negative pulmonary TB. Continuous follow-up of chest radiograph to detect migrating lesions, and serologic test with ELISA method to detect parasite-specific IgG antibodies would be quite useful for the diagnosis of paragonimiasis in patients with unusual clinical course.
Figures and Tables
Figure 1
The initial chest radiography at our institute shows the suspiciously small nodular opacity (arrow) in the suprahilar region of the right upper lobe.

Figure 2
(A, C) Lung setting of the initial chest high resolution computed tomography (CT) scans show the subpleural focal consolidation with cavitation (arrow) in the right upper lobe. (B, D) Lung setting of the chest CT scans, after receiving 6 months of anti-tuberculosis medication, shows a decrease in the extent of the subpleural consolidation with cavitation in the right upper lobe.
Figure 3
(A, D) Lung setting of chest computed tomography (CT) scans at four months after completion of the anti-tuberculosis medication shows the newly developed subpleural consolidations in the right upper lobe. (B, E) Lung setting of the chest CT scans at three months after re-treatment show a decrease in the extent of the pre-existing consolidations and the newly developed subpleural nodule (arrow) in the right upper lobe. (C, F) Lung setting of the chest high resolution CT scans at five months after re-treatment show the pre-existing nodule with newly developed cavitation (arrow) in the right upper lobe.
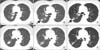
Figure 4
Pathologic findings of the thoracosopic wedge resection specimen and microscopic findings. (A) Histopathologic examination reveals cavitary parasitic granuloma with eggs of Paragonimus westermani and hemorrhage and acute and chronic inflammatory cell infiltration, including eosinophilis (arrow) (H&E stain, ×10). (B) Biopsy showed distorted and yellowish refractile eggs on high power view (H&E stain, ×40).

References
1. Yang SP, Huang CT, Cheng CS, Chiang LC. The clinical and roentgenological courses of pulmonary paragonimiasis. Dis Chest. 1959; 36:494–508.
2. Singh TS, Mutum SS, Razaque MA. Pulmonary paragonimiasis: clinical features, diagnosis and treatment of 39 cases in Manipur. Trans R Soc Trop Med Hyg. 1986; 80:967–971.
3. Kim KU, Lee K, Park HK, Jeong YJ, Yu HS, Lee MK. A pulmonary paragonimiasis case mimicking metastatic pulmonary tumor. Korean J Parasitol. 2011; 49:69–72.
4. Siddiqi K, Lambert ML, Walley J. Clinical diagnosis of smear-negative pulmonary tuberculosis in low-income countries: the current evidence. Lancet Infect Dis. 2003; 3:288–296.
5. Song JU, Um SW, Koh WJ, Suh GY, Chung MP, Kim H, et al. Pulmonary paragonimiasis mimicking lung cancer in a tertiary referral centre in Korea. Int J Tuberc Lung Dis. 2011; 15:674–679.
6. Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS, Lee KS, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005; 128:1423–1430.
7. Kim TS, Han J, Shim SS, Jeon K, Koh WJ, Lee I, et al. Pleuropulmonary paragonimiasis: CT findings in 31 patients. AJR Am J Roentgenol. 2005; 185:616–621.
8. Sim YS, Lee JH, Hong SC, Chang JH, Kang SR, Yang HJ, et al. Paragonimus westermani found in the tip of a little finger. Intern Med. 2010; 49:1645–1648.
9. Tay NS, Ong KC, Tan SY, Kaw GJ. Tuberculosis mimicry. Eur Respir J. 2005; 26:554–556.
10. Moon YR, Lee YD, Park SH, Cho YS, Na DJ, Cho YS, et al. A case of paragonimiasis that was suspicious for a lung malignancy by PET/CT. Tuberc Respir Dis. 2007; 63:521–525.
11. Ryu YH, Woo DH, Park JE, Kim HJ, Shin KC, Chung JH, et al. A case of paragonimiasis suspected lung cancer. Yeungnam Univ J Med. 2010; 27:69–73.
12. Johnson JR, Falk A, Iber C, Davies S. Paragonimiasis in the United States: a report of nine cases in Hmong immigrants. Chest. 1982; 82:168–171.
13. Boland JM, Vaszar LT, Jones JL, Mathison BA, Rovzar MA, Colby TV, et al. Pleuropulmonary infection by Paragonimus westermani in the United States: a rare cause of eosinophilic pneumonia after ingestion of live crabs. Am J Surg Pathol. 2011; 35:707–713.
14. Jeon K, Song JU, Um SW, Koh WJ, Suh GY, Chung MP, et al. Bronchoscopic findings of pulmonary paragonimiasis. Tuberc Respir Dis. 2009; 67:512–516.
15. Oh IJ, Kim YI, Chi SY, Ban HJ, Kwon YS, Kim KS, et al. Can pleuropulmonary paragonimiasis be cured by only the 1st set of chemotherapy? Treatment outcome and clinical features of recently developed pleuropulmonary paragonimiasis. Intern Med. 2011; 50:1365–1370.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download