Abstract
Miliary brain metastasis from the lung is uncommon and has a poor therapeutic response. We report a case of pulmonary adenocarcinoma combined with multiple brain cystic lesions that were initially misdiagnosed as neurocysticercosis. A 53-year-old male who never smoked was admitted to our hospital with complaints of agitation and cognitive impairment. Brain magnetic resonance imaging showed innumerable, small nodular lesions with a central, low signal intensity in whole brain parenchyma. His symptoms were not improved by the empirical praziquantel medication for disseminated neurocysticercosis. After a transbronchial biopsy from the right middle lobe, we could diagnose the primary lung adenocarcinoma with a single nucleotide polymorphism in the epidermal growth factor receptor exon 20 at codon 787 (Q787Q). His neurologic symptoms and imaging findings have been gradually improving with a first-line Gefitinib treatment for five months. We recommend a more active diagnostic approach including biopsy in case of atypical imaging findings.
Figures and Tables
Figure 1
The initial chest X-ray shows multiple miliary nodular lesions in the lower right lung fields. (B) After 1 month of the gefitinib treatment, the lesions are remarkably improved on X-ray. (C) Chest CT shows irregular nodular interstitial thickenings and consolidations combined with innumerable tiny nodules in the right middle and lower lobes. (D) After 1 month of the gefitinib treatment, the lesions are remarkably improved on CT scan. CT: computed tomography.
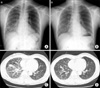
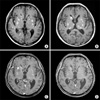
Figure 2
(A) The initial brain MRI of an outside hospital shows multiple cystic lesions with tiny scattered calcified nodules. (B) After 4 months, a follow-up MRI shows innumerable, small nodular lesions (up to 1.6 cm) with a central, low signal intensity in the whole brain parenchyma, suggestive of disseminated neurocysticercosis at the vesicular stage. (C) The cystic and nodular lesions are improved by a gefitinib treatment for 1 month. (D) The cystic and nodular lesions are improved by a gefitinib treatment for 5 months. MRI: magnetic resonance imaging.
References
1. Klos KJ, O'Neill BP. Brain metastases. Neurologist. 2004. 10:31–46.
2. Ruppert AM, Stankoff B, Lavolé A, Gounant V, Milleron B, Seilhean D. Miliary brain metastases in lung cancer. J Clin Oncol. 2010. 28:e714–e716.
3. Porta R, Sánchez-Torres JM, Paz-Ares L, Massutí B, Reguart N, Mayo C, et al. Brain metastases from lung cancer responding to erlotinib: the importance of EGFR mutation. Eur Respir J. 2011. 37:624–631.
4. Katayama T, Shimizu J, Suda K, Onozato R, Fukui T, Ito S, et al. Efficacy of erlotinib for brain and leptomeningeal metastases in patients with lung adenocarcinoma who showed initial good response to gefitinib. J Thorac Oncol. 2009. 4:1415–1419.
5. Kim JE, Lee DH, Choi Y, Yoon DH, Kim SW, Suh C, et al. Epidermal growth factor receptor tyrosine kinase inhibitors as a first-line therapy for never-smokers with adenocarcinoma of the lung having asymptomatic synchronous brain metastasis. Lung Cancer. 2009. 65:351–354.
6. Jackman DM, Holmes AJ, Lindeman N, Wen PY, Kesari S, Borras AM, et al. Response and resistance in a non-small-cell lung cancer patient with an epidermal growth factor receptor mutation and leptomeningeal metastases treated with high-dose gefitinib. J Clin Oncol. 2006. 24:4517–4520.
7. García HH, Del Brutto OH. Imaging findings in neurocysticercosis. Acta Trop. 2003. 87:71–78.
8. Iguchi Y, Mano K, Goto Y, Nakano T, Nomura F, Shimokata T, et al. Miliary brain metastases from adenocarcinoma of the lung: MR imaging findings with clinical and post-mortem histopathologic correlation. Neuroradiology. 2007. 49:35–39.
9. Ruppert AM, Stankoff B, Lavolé A, Gounant V, Milleron B, Seilhean D. Miliary brain metastases in lung cancer. J Clin Oncol. 2010. 28:e714–e716.
10. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004. 22:2865–2872.
11. Soffietti R, Cornu P, Delattre JY, Grant R, Graus F, Grisold W, et al. EFNS Guidelines on diagnosis and treatment of brain metastases: report of an EFNS Task Force. Eur J Neurol. 2006. 13:674–681.
12. Kvale PA, Simoff M, Prakash UB;. American College of Chest Physicians. Lung cancer. Palliative care. Chest. 2003. 123:1 Suppl. 284S–311S.
13. Cataldo VD, Gibbons DL, Pérez-Soler R, Quintás-Cardama A. Treatment of non-small-cell lung cancer with erlotinib or gefitinib. N Engl J Med. 2011. 364:947–955.
14. Mu XL, Li LY, Zhang XT, Wang MZ, Feng RE, Cui QC, et al. Gefitinib-sensitive mutations of the epidermal growth factor receptor tyrosine kinase domain in chinese patients with non-small cell lung cancer. Clin Cancer Res. 2005. 11:4289–4294.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download