Abstract
Objective
The aim of this retrospective study was to evaluate and compare the changes in the pharyngeal airway (PA), maxillary sinus volume, and skeletal parameters after rapid maxillary expansion (RME) and alternate rapid maxillary expansion and constriction (Alt-RAMEC) followed by facemask (FM) therapy.
Methods
The records of 40 patients with skeletal Class III malocclusion due to maxillary retrognathism were collected, and the patients were assigned into two groups. The first group comprised 8 male and 12 female patients (mean age, 10.0 ± 1.1 years) treated using RME/FM for an average of 10 months. The second group comprised 10 male and 10 female patients (mean age, 9.64 ± 1.3 years) treated using Alt-RAMEC/FM for an average of 12 months. Cone-beam computed tomography images acquired before (T0) and after treatment (T1) were evaluated.
Results
Regarding the skeletal effects, significant differences between the groups were the increase in ANS-HRP (perpendicular distance of ANS to the horizontal reference plane, 0.99 mm, p <0.05) in the Alt-RAMEC/FM group and the decrease in PP-SN (palatal plane to Sella-Nasion plane, 0.93°, p < 0.05) in the RME/FM group. Maxillary sinus volumes increased significantly in both the groups, and the increase was statistically significantly higher in the Alt-RAMEC/FM group. Although no significant intergroup differences were observed in PA volumes, both lower (1,011.19 mm3) and total (1,601.21 mm3), PA volume increased significantly in the Alt-RAMEC/FM group.
Class III malocclusion is one of the most difficult malocclusions to diagnose and treat.1 Since the 1970s, researchers have agreed that most Class III malocclusions have maxillary retrognathism as a part of their etiology.2
In growing patients, maxillary protraction with a facemask (FM) following rapid maxillary expansion (RME) has been proven to have an effect on correcting malocclusions in both skeletal and soft-tissue structures.3 In terms of RME, both conventional expansion methods (Hyrax, Haas, etc.) and the alternate rapid maxillary expansion and constriction (Alt-RAMEC) protocol can be successfully performed.4 Studies have suggested that using the Alt-RAMEC protocol prior to FM therapy might increase the forward movement of the maxilla rather than when using the conventional methods.45 However, the effects of these treatment methods on the pharyngeal airway (PA) remain controversial. Most of the relevant studies in the literature evaluated the effects of the RME/FM protocol on airway dimensions. While some of the studies showed increases in nasopharyngeal6789 or oropharyngeal68 airway dimensions, other studies reported no significant changes in airway dimensions.101112 Moreover, the effects of the Alt-RAMEC/FM protocol on airway changes have not been evaluated thoroughly. Only Celikoglu and Buyukcavus13 examined PA changes two-dimensionally after the Alt-RAMEC/FM protocol and reported an increase in upper PA dimensions. However, the expansion device used in that study contained a Hyrax screw and was activated twice a day, which was different from the routine Alt-RAMEC protocol introduced by Liou and Tsai.4
In the literature, only one study has evaluated the maxillary sinuses after RME followed by FM therapy. This study reported that the increases in maxillary sinus volumes were due to the normal growth of individuals.12
Most of the studies measured airway changes by using two-dimensional (2D) cephalometric images, which can only show anteroposterior linear changes. Recently, cone-beam computed tomography (CBCT) has allowed volumetric assessment, which is more favorable for evaluating the morphology of the airway structures.14 Hence, the aim of this study was to evaluate and compare the three-dimensional (3D) changes in PA and maxillary sinus volumes, as well as skeletal changes, after RME and Alt-RAMEC protocols followed by FM therapy in patients with skeletal Class III malocclusion characterized by maxillary retrognathism.
This single-center, single-blinded retrospective study was reviewed and approved by the ethical committee of Marmara University, Institute of Health Sciences (Istanbul, Turkey, 23.02.2015-5).
The CBCT records of 78 patients with Class III malocclusion treated using orthopedic approaches between 2006 and 2016 were retrieved from the archives of Department of Orthodontics, Faculty of Dentistry, Marmara University. The inclusion criteria were as follows: 1) patients in the active growth period determined according to the cervical vertebral maturation method; 2) skeletal Class III malocclusion due to maxillary retrognathism (N perpendicular to A point < −1 mm, SNA < 80°, maxillary depth < 90°), with a normal/low-angle growth pattern; 3) patients with primary or mixed dentition; and 4) patients treated with FM following either the RPE or Alt-RAMEC protocols. The exclusion criteria were as follows: 1) congenital deformities in the craniofacial area, 2) airway dysfunction history, 3) missing or unclear records, and 4) patients reported to have cooperation problems during treatment. The flow diagram of patient selection based on the CONSORT statement is shown in Figure 1. Finally, 40 patients were assigned into two groups according to treatment type. Twenty patients (12 females and eight males) treated with RME/FM and 20 patients (10 males and 10 females) treated with Alt-RAMEC/FM were included in the study. The mean age of the patients in the RME/FM group was 10.0 ± 1.1 years, while that of patients in the Alt-RAMEC/FM group was 9.64 ± 1.3 years. A power analysis revealed that a minimum number of 24 patients would provide sufficient statistical power (n > 24, α level of 0.05, and power of 0.80).
In the RME/FM group, a Hyrax acrylic cap device (Leone A0620; Leone Orthodontic Products, Sesto Fiorentino, Italy) was used for the expansion protocol (Figure 2A), followed by maxillary protraction with an ORMCO®-Adjustable Dynamic Protraction Facemask™ (Ormco Corp., Orange, CA, USA). The Hyrax screw was activated twice a day (0.5 mm/day) for 7 days, and on the seventh day, the patients were instructed to wear the FM for a minimum of 16 hours/day.
In the Alt-RAMEC/FM group, a double-hinged expansion screw (US Patent No. 6334771B1; Bestdent, Kaohsiung, Taiwan)4 was used for the expansion protocol (Figure 2B), followed by maxillary protraction with an ORMCO®-Adjustable Dynamic Protraction Facemask™. The screw was activated at a rate of 1 mm/day (two turns in the morning and two turns in the evening) for 1 week; in the following week, the screw was closed at a rate of 1 mm/day (two turns in the morning and two turns in the evening) as described in the routine protocol.4 The opening and closing processes were repeated for 9 weeks. After 9 weeks, the patients were instructed to wear the FM for a minimum of 16 hours/day.
In both the groups, the treatment was completed when full-cusp Class II canine and molar relationships were achieved for overcorrection in order to compensate for late mandibular growth and relapse possibilities. The total treatment times were, on average, 10 months for the RME/FM group and 12 months for the Alt-RAMEC/FM group.
In both the groups, two sets of CBCT images were acquired, one before treatment (T0, before cementing the expansion appliance) and one after treatment (T1, right after the removal of the Hyrax in the RME/FM group following the termination of FM therapy and after retention with the Bionator in the Alt-RAMEC/FM group). The CBCT images were acquired using an Iluma Imtec Imaging Machine (3M, Ardmore, OK, USA; X-ray tube voltage: 120 kV; X-ray tube current: 1–4 mA; scanning time: 40 seconds maximum and 7.8 seconds minimum; field of view: 14.2 × 21.1 cm; voxel size: 0.0936 mm; grey scale: 14 bit) while the patients were sitting in an upright position with their Frankfurt horizontal plane adjusted parallel to the floor. All volumetric and skeletal changes were analyzed using Mimics version 19.0 software (Materialise Europe, World Headquarters, Leuven, Belgium). All measurements were performed by the same examiner who was blinded to the type of treatment protocols and was not involved in treating the patient.
After uploading the DICOM data to the Mimics 19.0 software, a head mask with a threshold value for the skeletal tissue (minimum 226 Hounsfield unit [HU] and maximum 3,071 HU as instructed in the Mimics software) and a 3D image were created. The horizontal reference plane (HRP) was created between the right and left porion points and the right infraorbital point. The vertical reference plane (VRP) was created with a plane passing through the right and left porion points perpendicular to the HRP (Figure 3). In order to evaluate the changes achieved by treatment, the pretreatment and posttreatment 3D images were superimposed on the cranial base. The skeletal measurements were performed using the same reference planes as those created on the pretreatment images (Figure 3).
After creating the mask for the airway (minimum −1,024 HU and maximum −400 HU),15 the following borders were created to measure the PA volume. The superior border was defined as the point before the last slice where the posterior wall of the pharynx and the nasal septum fused. The superior border was first identified on the axial slice and it was then marked on the sagittal slice. The inferior border was defined using a plane parallel to the HRP that passed from the most anterior and inferior points of the second vertebra (CV2). The superior-anterior border was defined using a plane between the points of the superior border and the posterior nasal spine (PNS). The posterior pharyngeal wall formed the posterior border. After cropping the airway mask with the selected borders, a 3D image of the airway was created and divided into two, by using a plane parallel to the HRP that passed from the most anterior and inferior points of the first vertebra (CV1). The total PA, upper PA, and lower PA volumes were calculated separately (Figure 4).
The masks for the maxillary sinuses were created using the same threshold values as those used for the PA. The right and left sinuses were evaluated separately with respect to their outer borders. If polyps were observed in the sinus, they were also included in the mask, since their place was normally occupied by air (Figure 5).
IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. To assess intraexaminer reliability, the measurements were repeated for eight randomly selected patients 1 week after the first measurements. The conformity of the parameters to the normal distribution was assessed using the Shapiro-Wilks test. Student's t-test was used for the intergroup comparisons of the parameters with a normal distribution. The paired-samples t-test was used for the within-group comparisons of parameter changes from the T1 values to the T0 values. The intraclass correlation coefficient (ICC) was calculated for analyzing the method error. Significance was evaluated at a level of p < 0.05.
All the measurements were repeated by the same operator. ICCs, which were calculated for each variable to assess the reliability of the measurements, ranged from 0.851 to 1.000 and showed a high level of agreement.
There was no statistically significant difference between the groups in terms of the mean ages (p < 0.05).
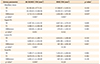
No significant changes were observed in any of the PA volumes in the RME/FM group. In the Alt-RAMEC/FM group, the lower and total PA volumes increased significantly (1,011.19 and 1,601.21 mm3, respectively). However, no statistically significant difference was observed between the two groups regarding the volume changes in PA measurements (Table 1).
The results showed statistically significant increases in the volumes of the maxillary sinuses in both the groups, which was significantly higher in the Alt-RAMEC/FM group (2,712.14 mm3) (Table 1).
In the RME/FM group, the A point moved 2.53 ± 1.01 mm forward with significant increases of 2.68 ± 1.1° in the SNA angle and 2.59 ± 1.48° in the ANB angle (p < 0.05). The B-VRP and SNB did not show any statistically significant changes. The PP-SN angle presented a significant decrease of 0.93 ± 1.13° due to the downward movement of the PNS point by a mean of 1.07 ± 0.85 mm (p < 0.05). The distances related to vertical face height (S-Go, N-Me, and ANS-Me) also showed statistically significant increases (Table 2).
In the Alt-RAMEC/FM group, the A point moved significantly forward with an increase of 2.73 ± 0.99 mm, and the significant increases in the SNA and ANB angles confirmed the forward movement (2.71 ± 1.23° and 2.36 ± 1.18°, respectively). The B-VRP and SNB did not show any statistically significant changes. The ANS and PNS points presented statistically significant downward movements according to the HRP (0.99 ± 0.74 mm and 1.05 ± 0.87 mm, respectively). Statistically significant increases were also observed in the parameters of vertical face height (1.92 ± 1.48 mm in S-Go, 3.04 ± 1.64 mm in N-Me, 2.48 ± 1.60 mm in ANS-Me, 0.89 ± 0.9° in FMA, and 0.87 ± 0.86° in GoMe-SN) (Table 2).
When changes achieved after the treatment protocols were compared between the groups, only the PP-SN and ANS-HRP showed statistically significant differences. The palatal plane angle (−0.93°) decreased in the RME/FM group during the treatment, and the ANS point (0.99 mm) moved downward in the Alt-RAMEC/FM group (Table 2).
Growing patients with Class III malocclusion presenting maxillary retrognathism can be treated successfully with FM therapy.3 The application of RME with either the conventional or Alt-RAMEC protocols prior to FM therapy is thought to have a stimulating effect on the circummaxillary sutures, as well as increasing the forward movement of the maxilla.1617 Additionally, studies have reported that the amount of maxillary forward movement with the Alt-RAMEC protocol exceeds the amount that was reported with the conventional methods because of increased sutural activity.45 Therefore, the aim of this study was to compare the skeletal changes of these two methods together with the effects on the PA and maxillary sinus volumes since no previous study had compared these treatment protocols by using CBCT images.
It is important to comply with the ALARA (as low as reasonably achievable) principle and the SEDENTEXCT guidelines18 and use CBCT in only selected orthodontic cases. The 3D imaging techniques were used in this retrospective study because of the complex morphological structures of the PA and maxillary sinuses, which limit the evaluation using 2D imaging methods.
Numerous 3D methods for measuring the PA volume have been suggested, but no researchers follow the exact same method. We endeavored to use the most reasonable points and planes that were used in recent studies and were least affected by the treatment protocols. The points were mostly defined by hard bony landmarks rather than unstable and flexible soft-tissue ones. In addition, we concentrated on limiting the number of defined points to decrease the subjective and systemic errors in the measurements. We used the most anteroinferior point of CV2 to define the inferior border of the pharynx instead of the epiglottis, which is an unstable and flexible soft-tissue landmark, as was done by El and Palomo.19 Most of the airway studies141920 used the palatal plane as a border between the nasopharynx and oropharynx. However, the palatal plane is affected by the treatment protocols, and this might have an impact on airway volume changes. Therefore, a plane parallel to the HRP passing through CV1 was used in our study to separate the PA into the upper and lower PA. The description of El and Palomo19 for the superior limit of the nasopharynx was the last slice before the fusion of the nasal septum with the posterior wall of the pharynx, and because of its reproducibility, we preferred to use it as a reliable definition in our study.
In the RME/FM group, the maxilla moved 2.53 mm forward, which was similar to the results found in the literature.12212223 No significant movement was observed in the ANS, while the PNS moved 1.07 mm downward. As a result, the palatal plane angle (PP-SN) showed a significant decrease of 0.93°, which coincided with prior findings.1221222324 In agreement with previous studies,725 the angular measurements related to the vertical measurements did not show any significant changes, while the anterior (N-Me and ANS-Me) and posterior (S-Go) face heights showed statistically significant increases in our study.
In the Alt-RAMEC/FM group, the maxilla showed a statistically significant forward movement (2.73 mm). Previous studies have reported different findings regarding the movement of the A point following the Alt-RAMEC protocol. Liou and Tsai4 showed a 5.8-mm forward movement of the A point; however, in their study, non-compliance intraoral protraction springs were used for 24 hours/day as a protraction method in patients with cleft lip and palate, whereas the FM was used for 16 hours/day in our patients. Furthermore, they used cephalometric images, which we believe are not favorable for determining the A point in patients with cleft lip and palate. In contrast, Kaya et al.5 protracted the maxilla by using miniplates after the Alt-RAMEC protocol, and they reported a 2-mm forward movement of the A point. In the Alt-RAMEC/FM study of Celikoglu and Buyukcavus,13 a significant increase of 3.34° in the SNA angle was reported. However, only Liou and Tsai4 used a double-hinged expander as in our study. The differences in methodology (several evaluation methods, treatment protocols, expansion devices, etc.) in these studies might have caused the diversity in the results. The ANS and PNS points both moved downward almost by the same amount (0.99 mm and 1.05 mm, respectively). Consequently, no significant change was observed in the palatal plane angle. Accordingly, all measurements related to the anterior and posterior face heights increased in agreement with the findings of previous studies.51317
In our study, no significant difference was observed when the forward movement of the maxilla was compared between the groups. However, previous studies4513 reported that the Alt-RAMEC protocol enhanced the forward movement of the maxilla, unlike in the present study. Evaluation methods such as cephalometry versus CBCT, treatment protocols, different expansion devices, severity of Class III malocclusion, treatment duration, age, and patient cooperation across studies might cause differences in the results. With respect to the vertical movement of the palatal plane, the RME/FM group presented solely posterior extrusion of the maxilla, whereas the Alt-RAMEC group showed a parallel downward movement of the maxilla. The difference in the direction of palatal plane movement might have been caused by the difference in the type of expansion screw used in the Alt-RAMEC/FM group, which was a double-hinged expander claimed to allow the maxillary halves to freely move forward by carrying the center of rotation to the contact points between the pterygoid plate and tuberosity.
Because denying treatment to children with Class III malocclusion would be unethical, we were unable to include a control group in our study. Some prior studies have reported changes in the PA volumes with normal growth.262728 However, in those studies, either the airway volumes of patients with Class I malocclusion or single-time data of patients with Class III malocclusion were assessed. Therefore, we could not compare our results to those of such studies to ensure that we did not reach incorrect conclusions since patients having different skeletal discrepancies may show different amounts of airway growth.
In our study, no statistically significant difference was observed in any of the PA volumes in the RME/FM group. Most prior studies analyzing the PA dimensions after RME/FM treatment were based on 2D evaluations, and they obtained a range of results. Similar to our results, Mucedero et al.11 reported favorable skeletal changes after FM with or without RME, even though those changes did not reflect the sagittal changes in the nasopharyngeal and oropharyngeal dimensions. Hiyama et al.10 did not report any significant changes in upper airway dimensions either. In the 3D study by Chen et al.,27 significant increases in the nasopharyngeal and velopharyngeal airway volumes were reported contrary to our results. The authors found no significant changes in the glossopharyngeal and hypopharyngeal airway volumes, which was similar to the lower PA changes observed in our study. In contrast, Pamporakis et al.12 reported insignificant increases in the PA volume of the RME/FM group, as seen in our study. They attributed this result to the downward movement of the PNS point and counterclockwise rotation of the palatal plane, which might cause a downward movement of the surrounding soft tissues.
No 3D data were available for evaluating the PA volume following Alt-RAMEC/FM. Only one cephalometric study13 evaluated the changes in PA dimensions after the Alt-RAMEC/FM protocol. In this study, an increase in the upper PA dimension was reported because of the significant forward movement of the maxilla (a 3.34° increase in SNA), whereas no significant change was found in the lower PA dimension. The factors that differentiate their study and ours are the measurement method and expansion devices used. Another factor may be that the authors used 2D images to evaluate a 3D structure. The significant increase in the lower and total PA volumes might be related to the increase in the GoMe-SN and FMA angles in our study. However, no differences were found between the RME/FM and Alt-RAMEC/FM groups regarding PA volume changes.
In terms of the changes in maxillary sinus volume, a statistically significant difference was observed between the two groups in our study, and it was higher in the Alt-RAMEC/FM group. The difference might be related to the parallel downward movement of the palatal plane in the Alt-RAMEC group. In the literature, only one study evaluated maxillary sinus changes after RME followed by FM, and it concluded that the increases in maxillary sinus volume were due to the normal growth of individuals.12 However, no data were available on maxillary sinus volume changes due to growth in patients with Class III malocclusion. Most studies2930 report maxillary sinus growth in patients without any skeletal discrepancy. Therefore, we could not conclude whether the changes in the groups were due to treatment or normal growth of the individuals.
The present study was a retrospective study, which was one of its limitations. The second limitation was the absence of 3D data from an untreated control group with the same skeletal malocclusion. Therefore, future prospective studies including untreated Class III control groups with available CBCT images for evaluating airway changes are suggested.
• Both treatment approaches showed similar skeletal effects except the increase in the ANS-HRP (0.99 mm, p < 0.05) in the Alt-RAMEC/FM group and the decrease in the PP-SN (0.93°, p < 0.05) in the RME/FM group.
• Maxillary sinus volume increased significantly in both the groups and was significantly higher in the Alt-RAMEC/FM group.
• Although no significant differences were observed between the groups in PA volumes, the lower and total PA volumes presented statistically significant increases in the Alt-RAMEC/FM group.
Figures and Tables
Figure 1
The flow diagram of patient selection based on the CONSORT statement guidelines.
FM, Facemask; RME, rapid maxillary expansion; Alt-RAMEC, alternate rapid maxillary expansion and constriction; 3D, three-dimensional.

Figure 2
A, Intraoral photo of the Hyrax screw. B, Intraoral photo of the double-hinged expansion screw.

Figure 3
Skeletal measurements. 1, PP-SN (°); 2, GoMe-SN (°); 3, SNA (°); 4, SNB (°); 5, ANB (°); 6, FMA (°); 7, AVRP (mm); 8, B-VRP (mm); 9, ANS-HRP (mm); 10, PNSHRP (mm); 11, S-Go (mm); 12, ANS-Me (mm); 13, N-Me (mm).
PP-SN, The angle between palatal plane and sella-nasion plane; GoMe-SN, the angle between gonion-menton plane and sella-nasion plane; SNA, the angle between sella, nasion and A points; SNB, the angle between sella, nasion and B points; ANB, the angle between A, nasion and B points; FMA, the angle between Frankfort horizontal reference plane and mandibular plane; A-VRP, the distance between A point and the vertical reference plane; B-VRP, the distance between B point and the vertical reference plane; ANS-HRP, the distance between anterior nasal spine point and the horizontal reference plane; PNS-HRP, the distance between posterior nasal spine point and the horizontal reference plane; S-Go, the distance between sella and gonion points; ANS-Me, the distance between anterior nasal spine and menton points; N-Me, the distance between nasion and menton points.
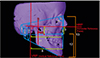
Figure 4
Three-dimensional reconstruction of the pharyngeal airway (PA).
Ch, The point before the last slice where the posterior wall of the pharynx and the nasal septum fuse; CV1, the most anterior and inferior points of the first cervical vertebra; CV2, the most anterior and inferior points of the second cervical vertebra; PNS, posterior nasal spine; HRP, horizontal reference plane.

Table 2
Evaluation of skeletal changes

Values are presented as mean ± standard deviation.
Alt-RAMEC, Alternate rapid maxillary expansion and constriction; FM, facemask; PA, pharyngeal airway.
*p < 0.05; †Student's t-test and ‡paired-samples t-test.
Definition of each landmark has been described in the legends of Figure 3.
Notes
References
1. Keles A, Tokmak EC, Erverdi N, Nanda R. Effect of varying the force direction on maxillary orthopedic protraction. Angle Orthod. 2002; 72:387–396.

2. Ellis E 3rd, McNamara JA Jr. Components of adult Class III malocclusion. J Oral Maxillofac Surg. 1984; 42:295–305.


3. Kama JD, Ozer T, Baran S. Orthodontic and orthopaedic changes associated with treatment in subjects with Class III malocclusions. Eur J Orthod. 2006; 28:496–502.


4. Liou EJ, Tsai WC. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J. 2005; 42:121–127.


5. Kaya D, Kocadereli I, Kan B, Tasar F. Effects of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions; a pilot study. Angle Orthod. 2011; 81:639–646.


6. Oktay H, Ulukaya E. Maxillary protraction appliance effect on the size of the upper airway passage. Angle Orthod. 2008; 78:209–214.


7. Kaygisiz E, Tuncer BB, Yüksel S, Tuncer C, Yildiz C. Effects of maxillary protraction and fixed appliance therapy on the pharyngeal airway. Angle Orthod. 2009; 79:660–667.


8. Kilinç AS, Arslan SG, Kama JD, Ozer T, Dari O. Effects on the sagittal pharyngeal dimensions of protraction and rapid palatal expansion in Class III malocclusion subjects. Eur J Orthod. 2008; 30:61–66.


9. Sayinsu K, Isik F, Arun T. Sagittal airway dimensions following maxillary protraction: a pilot study. Eur J Orthod. 2006; 28:184–189.


10. Hiyama S, Suda N, Ishii-Suzuki M, Tsuiki S, Ogawa M, Suzuki S, et al. Effects of maxillary protraction on craniofacial structures and upper-airway dimension. Angle Orthod. 2002; 72:43–47.

11. Mucedero M, Baccetti T, Franchi L, Cozza P. Effects of maxillary protraction with or without expansion on the sagittal pharyngeal dimensions in Class III subjects. Am J Orthod Dentofacial Orthop. 2009; 135:777–781.


12. Pamporakis P, Nevzatoğlu Ş, Küçükkeleş N. Three-dimensional alterations in pharyngeal airway and maxillary sinus volumes in Class III maxillary deficiency subjects undergoing orthopedic facemask treatment. Angle Orthod. 2014; 84:701–707.


13. Celikoglu M, Buyukcavus MH. Changes in pharyngeal airway dimensions and hyoid bone position after maxillary protraction with different alternate rapid maxillary expansion and construction protocols: a prospective clinical study. Angle Orthod. 2017; 87:519–525.


14. Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009; 135:468–479.


15. Yilmaz BS, Kucukkeles N. Skeletal, soft tissue, and airway changes following the alternate maxillary expansions and constrictions protocol. Angle Orthod. 2014; 84:868–877.


16. Gautam P, Valiathan A, Adhikari R. Skeletal response to maxillary protraction with and without maxillary expansion: a finite element study. Am J Orthod Dentofacial Orthop. 2009; 135:723–728.


17. Canturk BH, Celikoglu M. Comparison of the effects of face mask treatment started simultaneously and after the completion of the alternate rapid maxillary expansion and constriction procedure. Angle Orthod. 2015; 85:284–291.


18. The SEDENTEXCT Project. Radiation protection: cone beam CT for dental and maxillofacial radiology: evidence based guidelines 2011 (v2.0 final) [Internet]. The SEDENTEXCT Project;2011. Available from: www.sedentexct.eu/files/guidelines_final.pdf.
19. El H, Palomo JM. Airway volume for different dentofacial skeletal patterns. Am J Orthod Dentofacial Orthop. 2011; 139:e511–e521.

20. Iwasaki T, Hayasaki H, Takemoto Y, Kanomi R, Yamasaki Y. Oropharyngeal airway in children with Class III malocclusion evaluated by cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009; 136:318.e1–318.e9. discussion 318-9.

21. Ngan P, Hägg U, Yiu C, Merwin D, Wei SH. Soft tissue and dentoskeletal profile changes associated with maxillary expansion and protraction headgear treatment. Am J Orthod Dentofacial Orthop. 1996; 109:38–49.


22. Baik HS. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995; 108:583–592.


23. Kapust AJ, Sinclair PM, Turley PK. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998; 113:204–212.


24. Cordasco G, Matarese G, Rustico L, Fastuca S, Caprioglio A, Lindauer SJ, et al. Efficacy of orthopedic treatment with protraction facemask on skeletal Class III malocclusion: a systematic review and meta-analysis. Orthod Craniofac Res. 2014; 17:133–143.


26. Li H, Lu X, Shi J, Shi H. Measurements of normal upper airway assessed by 3-dimensional computed tomography in Chinese children and adolescents. Int J Pediatr Otorhinolaryngol. 2011; 75:1240–1246.


27. Chen X, Liu D, Liu J, Wu Z, Xie Y, Li L, et al. Three-dimensional evaluation of the upper airway morphological changes in growing patients with skeletal Class III malocclusion treated by protraction headgear and rapid palatal expansion: a comparative research. PLoS One. 2015; 10:e0135273.

28. Taylor M, Hans MG, Strohl KP, Nelson S, Broadbent BH. Soft tissue growth of the oropharynx. Angle Orthod. 1996; 66:393–400.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download